Fever & Rashes – By Dr. Manel Panapitiya
advertisement

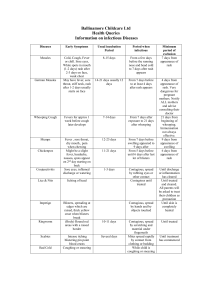
Dr(Mrs) M.S.Panapitiya Consultant Paediatrician why • Viral exanthum • Serious illness Main features • Well child / ill child • Erythematous / haemorrhagic rash Diagnostic clues • Association with fever • Distribution • Morphology Classfication of rashes • Mobiliform rashes • Scarlantiform rashes Rash that looks like measles Patients with Kawasaki disease drug reactions The rash consists macular lesions red 2-10 mm in diameter may be confluent papular lesions solid elevated above the rest of the skin • Has the pattern of scarlet fever • has innumerable small red papules • Patients with other conditions such as Kawasaki disease viral infections drug reaction • VIRAL INFECTIONS • BACTERIAL INFECTIONS • NONINFECTIVE Chicken pox Hand foot mouth disease Measles Rubella Fifth disease Sixth disease Dengue fever Erythema infectiousum Parvovirus B19 The preceding four exanthems were 1. Measles 2. Scarlet fever 3. Rubella 4. Atypical Scarlet fever ( Filatov-Dukes disease) 6. Roseola infantum (sixth disease) Benign, self-limited exanthematous illness of childhood. The prodromal phase • low-grade fever • headache • mild upper respiratory tract infection Characteristic rash occurs in three stages 1.erythematous facial flushing "slapped-cheek" appearance. 2. Spreads rapidly to the trunk and proximal extremities as a diffuse macular erythema 3. Central clearing of macular lesions occurs giving the rash a lacy, reticulated appearance. Palms and soles are spared, more prominent on extensor surfaces rash resolves spontaneously without desquamation Exanthem subitum Sixth disease Human herpes virus 6 (HHV-6) Primary HHV-6 infection occurs early in life. Peak acquisition of primary HHV-6 infection, from 6-15 m of age By 3-5 yr, 80-100% of children are seropositive The prodromal period • usually asymptomatic but may include • mild upper respiratory tract signs • mild conjunctival redness • cervical or, less frequently, occipital lymphadenopathy • mild palpebral edema. Clinical illness 101-106°F with an average of 103°F irritable and anorexic Seizures may occur in 5-10% of children Infrequently abdominal pain, vomiting, and diarrhea. Fever persists for 3-5 days, and then typically resolves rather abruptly (crisis) A rash appears within 12-24 hr of fever resolution Begins as discrete, small (2-5 mm), slightly raised pink lesions on the trunk and spreads to the neck, face, and proximal extremities Not pruritic, and no vesicles or pustules remain discrete but occasionally may become almost confluent. After 1-3 days, the rash fades. (rubeola) Measles has three clinical stages Incubation stage 10-12 days Prodromal stage 2- 4 days Disease stage 6-10 days prodromal phase characterized by • low-grade to moderate fever • conjunctivitis • coryza • dry cough • red mottling on the hard & soft palate • Koplik spots Koplik spots The pathognomonic sign of measles, appear by 2-3 days Grayish white dots, usually as small as grains of sand Opposite the lower molars They appear and disappear rapidly, usually within 12-18 hr. EXANTHEMATOUS PHASE The temperature rises abruptly as the rash appears neck, behind the ears, along the hairline, and on the posterior parts of the cheek Lesions macular, maculopapular confluent,haemorrhagic Spreads rapidly over the entire face, neck, upper arms, and upper part of the chest within the first 24 hr • Mx • • • • • admit iv fluids vit A antiotics NUTRITION • Complictions pneumonia diarrhoea malnutrition blindness encephalitis death (German or three-day measles) The incubation period is 1421 days The prodromal phase of mild catarrhal symptoms is shorter than that of measles and may go unnoticed Two thirds of infections are subclinical. RUBELLA Lymphadenopathy. most characteristic sign retroauricular, posterior cervical, and occipital An enanthem appears in 20% of patients just before the onset of the skin rash. discrete rose-colored spots on the soft palate (Forchheimer spots) Exanthem •It begins on the face and spreads quickly. •Discrete maculopapules are present in large numbers •Spread rapidly over the entire body, usually within 24 hr. •May be confluent •The eruption usually clears by the third day. •Rubella without a rash has been described. Coxsackievirus A Coxsackie B viruses Enterovirus 71 It is usually a mild illness, with or without low-grade fever. The oropharynx is inflamed and contains scattered vesicles on the tongue, buccal mucosa, posterior pharynx, palate, gingiva, and/or lips. These may ulcerate, leaving 4-8 mm shallow lesions with surrounding erythema. Develop the rash on the palms of the hands, soles of the feet, maybe on buttocks. Rash is not itchy, Starts out as small, flat, red dots turn into bumps or blisters(3-7mm) They are generally more common on the extensor surfaces Vesicles resolve in about 1 week Mx Symptomatic No specific therapy Vricella-Zoster Virus Patients are contagious 24-48 hr before the rash appears and until vesicles are crusted, usually 3-7 days after onset of rash Prodromal phase 24- 48 hr before the rash malaise, headache, anorexia fever - variable - resolves 2-4 days after the onset of the rash •The rash often appears first on the scalp, face, or trunk. •It can then spread over the entire body. Ulcerative lesions involving the oropharynx are common Vricella-Zoster Virus The initial exanthem The initial exanthem • Intensely pruritic • Erythematous macules • Papular stage • • Blisters on a pink base Dry brown crusts • New waves of blisters often spring up as the illness progresses Vricella-Zoster Virus Varicella is a more serious disease with higher rates of complications and deaths among infants, adults, and immunocompromised patients. Newborn with varicella Newborns have particularly high mortality around the time of delivery. Maternal varicella one week before or 2 days after birth frequently results in the newborn developing severe varicella The initial infection is intrauterine, although the newborn often develops clinical chickenpox postpartum. Newborn with varicella Rx : ZSIG IV Acyclovir CONGENITAL VARICELLA SYNDROME Up to 2% of fetuses whose mothers had varicella in the first 20 weeks of pregnancy may demonstrate VZV embryopathy Fetuses infected at 6-12 wk of gestation appear to have maximal interruption with limb development at 12-20 wk may have eye and brain involvement Stigmata of Varicella-Zoster Virus Fetopathy Cicatricial skin lesions Hypopigmentation Microphthalmia Cataracts Chorioretinitis Optic atrophy Microcephaly Hydrocephaly Calcifications Aplasia of brain Hypoplasia of an extremity Motor and sensory deficits Absent deep tendon reflexes Skin Eye Brain Limbs Varicella vaccine • • • • Live virus vaccine Recommended for children at 12-18 mo Can be given at any age Children 12 mo to 12 yr receive a single vaccine dose • Adolescents and adults require 2 vaccine doses, a minimum of 4 wks apart Breakthrough varicella 2-6 weeks after vaccination Could be due to either the wild or vaccine strains Usually very mild Potentially infectious Upper respiratory tract infection associated with a characteristic rash Infection with pyrogenic exotoxin producing group A streptococcus The rash appears within 24-48 hr after onset of upper respiratory symptoms begins around the neck and spreads over the trunk and extremities Diffuse, finely papular, erythematous eruption producing a bright red discoloration Blanches on pressure More intense along the creases of the elbows, axillae, and groin P Cheeks may be erythematous with pallor around the mouth. Pharynx is red The tongue is usually coated and the papillae are swollen After desquamation, the reddened papillae are prominent, giving the tongue a strawberry appearance. After 3-4 days, the rash begins to fade and is followed by desquamation Sheetlike desquamation may occur around the free margins of the fingernails, the palms, and the soles. Treatment •Group A streptococcus is sensitive to penicillin, and resistant strains have never been encountered. •Penicillin is, therefore, the drug of choice (except in patients who are allergic to penicillin) •Treatment with oral penicillin V for 10 days is recommended •It must be taken for a full 10 days even though there is symptomatic improvement in 3-4 days Toxic shock syndrome is caused by a toxin produced by certain types of Staphylococcus bacteria. A similar syndrome, called toxic shock-like syndrome (TSLS), can be caused by Streptococcal bacteria. The onset is abrupt high fever vomiting diarrhea sore throat headache myalgia Very ill Alteration in the level of consciousness Oliguria, hypotension progress to shock Disseminated intravascular coagulation • Exanthum A diffuse erythematous macular rash (scarlatiniform) appears within 24 hr Hyperemia of pharyngeal& conjunctival, mucous membranes Strawberry tongue is common Diagnostic criterias Fever lasting for at least 5 days Fever lasting for at least 5 days Presence of at least four of the following five signs: 1. Bilateral bulbar conjunctival injection, generally nonpurulent 2. Changes in the mucosa of the oropharynx, injected pharynx red, dry & fissured lips strawberry tongue 3.Changes of the peripheral extremities Edema and/or erythema of the hands or feet in the acute phase Periungual desquamation in the subacute phase 4.Rash, primarily truncal polymorphous but nonvesicular Rash of various forms (maculopapular, erythema multiforme, or scarlatiniform) with accentuation in the groin area 5.Cervical adenopathy, ≥1.5 cm usually unilateral nonpurulent Mycoplasma pneumoniae • Skin lesions include a variety of exanthems, most notably Maculopapular rashes Erythema multiforme Stevens-Johnson syndrome Dengue fever rash A transient, macular, generalized rash that blanches under pressure may be seen during the first 24-48 hr of fever. A generalized, morbilliform, maculopapular rash appears that spares the palms and soles. Rarely there is edema of the palms and soles. Petecial rash - Usually found on the limbs this rash is as a result of bleeding under the skin surface. Bright red rash - skin becomes florid and bright red in appearance. there will be some 'normal' areas of skin which are unaffected. ?TRANSIENT APLASTIC CRISIS •The incubation period for is shorter than for erythema infectiosum because it occurs coincident with the viremia. •B19-induced aplastic crises occur in TRANSIENT APLASTIC CRISIS. patients with all types of chronic hemolysis •These patients are ill with fever, malaise, and lethargy and have signs and symptoms of profound anemia •Rash is rarely present. C0NGENITAL INFECTION (PARVOVIRUS B19) Primary maternal infection is associated with nonimmune fetal hydrops and intrauterine fetal demise The mechanism of fetal disease appears to be a viral-induced red cell aplasia at a time when the fetal erythroid fraction is rapidly expanding. The second trimester seems to be the most sensitive period, but fetal losses are reported at every stage of gestation • probably the most common cause of stomatitis in children 1-3 yr of age, • The symptoms may appear abruptly, with pain in the mouth, salivation, fetor oris, refusal to eat, and fever, often as high as 4040.6°C • Fever and irritability may precede the oral lesions by 1-2 days. • The initial lesion is a vesicle which is seldom seen because of its early rupture. • The residual lesion is 2-10 mm in diameter and is covered with a yellow-gray membrane. • the tongue and cheeks are most commonly involved, no part of the oral lining is • Submaxillary lymphadenitis is common. • The acute phase lasts 4-9 days and is self-limited reatment Any foreign materials, such as tampons, vaginal sponges, or nasal packing, will be removed. Sites of infection (such as a surgical wound) will be drained. The goal of treatment is to maintain important body functions. This may include: Antibiotics for any infection (may be given through an IV) Dialysis (if severe kidney problems are present) Fluids through a vein (IV) Methods to control blood pressure Intravenous gamma globulin may help in severe cases Dukes' disease or fourth disease An exanthem-producing infectious disease of childhood of unknown aetiology. Synonym: Filatov's disease, fourth disease, Signs and tests No single test can diagnose toxic shock syndrome. The diagnosis is based on several criteria: fever, low blood pressure, a rash that peels after 1-2 weeks, and problems with the function of at least three organs. In some cases, blood cultures may be positive for growth of S. aureus. Treatment