ENDOCRINE SYSTEM
advertisement
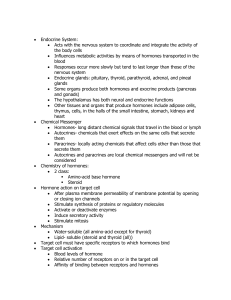
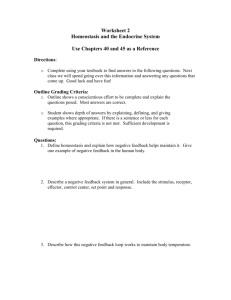
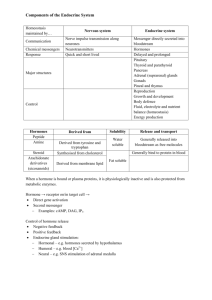
Physiology ENDOCRINE SYSTEM Edited by: Dr. Gholamreza Komeili Comparison of Nervous and Endocrine Systems Nervous Endocrine messenger electrochemical hormone (chemical) response milliseconds seconds to days duration short-lived long-lived one system (several distribution subsystems) widely scattered NOTE: Nervous and endocrine systems work together to coordinate and integrate activities of body (homeostasis) Functions of Endocrine System 1. Reproduction 2. Growth and development 3. Response to stress 4. Maintenance of fluid (water), electrolyte and nutrient balance 5. Regulation of cellular metabolism and energy Organs of the Endocrine System 1. Pituitary gland 2. Hypothalamus (neuroendocrine) 3. Pineal gland 4. Thyroid gland 5. Parathyroid gland 6. Thymus gland 7. Adrenal gland 8. Pancreas (also has exocrine function) 9. Gonads (testes or ovaries - also have exocrine functions) Topics • Hormone – Types – Modes of Action – Target cell activation – Control • Specific glands, their hormones, and disorders – Pituitary – Thyroid – Parathyroid – Adrenal – Pancreas – Thymus – Gonads (testes and ovaries) • General Adaptation Syndrome • chemicals Hormones • secreted by endocrine gland cells into blood (by way of interstitial fluid) • regulate metabolic functions of other cells (called target cells) • carried to all cells, but action is specific to cells that have receptors for the hormone – specificity of body’s response to hormone depends on how many cells have the receptor (highly specific if few cells respond [e.g., ACTH]; diffuse action if many respond [e.g., thyroxin]) Chemical Types of Hormones • Amino-acid based (amino acids, short or long peptides, proteins) – e.g., insulin, growth hormone, prolactin • Steroids - lipid derivatives of cholesterol – e.g., hormones from gonads (testosterone, estrogen) – e.g., hormones from adrenal cortex (adrenocortical hormones) • Eicosanoids - locally-secreted, locally-acting hormones secreted by all cell membranes (e.g., prostaglandins, which increase blood pressure and contribute to uterine contraction) Types of Changes in Target Cells • plasma membrane permeability changes (opening of protein channels; may change membrane potential) • activation of genes for increased protein synthesis, including enzymes • activation or deactivation of enzymes already present • secretion of cellular products • stimulation of cell division (mitosis) Mechanisms of Action • action in target cell depends on receptor • receptor may be: – in plasma membrane • second messenger mechanisms • used by most amino acid-based hormones (water soluble) – intracellular (in cytoplasm or nucleus) • direct gene activation • used by steroids and thyroid hormones (lipid soluble) Mechanisms of Action: Steroids • bind to intracellular receptors • hormone diffuses through plasma membrane and makes its way to nucleus – > where it binds with intracellular receptor to form hormone-receptor complex – > hormone-receptor complex interacts with chromatin (DNA) to affect gene activity (turn genes on or off) – > synthesis of mRNA – > synthesis of protein Steroid Signaling Mechanism of Action: Thyroid Hormone • similar to mechanism for steroid hormones • diffuses across plasma membrane – diffuses into nucleus where it interacts with intracellular receptors to activate genes for proteins (enzymes) involved in cellular respiration (glycolysis) – also, binds to receptors at mitochondria to activate genes for proteins involved in cellular respiration (Krebs cycle and electron transport chain) Mechanisms of Action: Other Hormones * plasma membrane receptor • used by most amino acid-based hormones • interaction of hormone with plasma membrane receptor results in activation of second messenger systems (cyclic AMP or PIP-calcium) • activation of second messenger has cascade effect resulting in: – enzyme activation, or – membrane permeability changes or secretion Membrane Receptor Mechanisms: 1. Cyclic AMP (cAMP) Signaling • interaction of hormone with receptor – > activates G protein (cleaves phosphate from GTP)-> excitation – > G protein activates adenylate cyclase – > adenylate cyclase forms cAMP from ATP – > cAMP activates protein kinases – > protein kinases activate (or inhibit) other proteins by phosphorylation – > cAMP degraded by enzyme • slightly different G protein inactivates adenylate cyclase associated with different hormone receptor • Link to animation: http://student.ccbc.cc.md.us/c_anatomy/animat/cAMP.htm cAMP Signaling Mechanism Membrane Receptor Mechanisms: 2. PIP-Calcium Signaling • interaction of hormone with receptor --> activates membrane-bound enzyme phospholipase – > phospholipase cleaves PIP2 (phosphatidyl inositol diphosphate) into diacylglycerol (DAG) and IP3 -- each of which acts as a second messenger • diacylglycerol (DAG) activates protein kinases • IP3 (inositol triphosphate) causes release of Ca2+ into cytoplasm (from endoplasmic reticulum or other storage areas) --> Ca2+ acts as third messenger PIP-Calcium Mechanism (con’t) -> Ca2+ (third messenger) – changes enzyme activity and plasma membrane channels, or – binds to calmodulin (intracellular regulatory protein) --> activates enzymes – see Fig. 17.2 for examples of proteins that act through membrane-receptors and 2nd messengers PIP-Calcium Signaling Mechanism Factors Affecting Target Cell Activation a. blood levels of hormone, which depend on: – rate of hormone release – rate of deactivation (by target cell or liver) b. affinity of hormone for receptor – greater affinity means greater association --> greater effect c. number of receptors available Factors Affecting Target Cell Activation (con’t) c. number of receptors available – up-regulation: increase in blood level of specific hormone (normally present at low levels) causes cells to make more receptors – down-regulation: prolonged exposure to high level of specific hormone --> cells remove some receptors -->return to normal response level – cross-regulation: influence of one hormone on number of receptors for another hormone; e.g., progesterone causes uterus to make fewer estrogen receptors; estrogen causes uterus to make more progesterone receptors Hormone Removal • hormones may be: – degraded by specific enzymes within target cells; – removed from blood by kidneys (excreted in urine) – degraded by liver (excreted in urine and feces) • half-life - time for 1/2 of hormone to be removed (from a fraction of a minute to 30 minutes) • onset - time from release to action (minutes [amino acidbased] to days [steroids]) • duration of action - how long the effects last (~20 minutes to several hours) Control of Hormone Release • Humoral control • Neural control • Hormonal control Control of Hormone Release: Humoral Hormone released in response to changing blood levels of ion or nutrient (negative feedback) parathyroid glands: detects low blood Ca2+ PTH raises blood Ca2 thyroid (Para follicular cells) detect high blood Ca2+->calcitonin -->decrease blood Ca2+ Control of Hormone Release: Humoral Other examples: • pancreas: – beta cells detect high blood glucose insulin decreases blood glucose – alpha cells detect low blood glucose glucagon raises blood glucose • zona glomerulosa (of adrenal cortex) detects low blood Na+ or high blood K+ aldosterone , K+ Control of Hormone Release: Neural Hormone released in response to nerve impulse preganglionic fibers of sympathetic division stimulate release of catecholamines (epinephrine, norepinephrine) from adrenal medulla impulses from hypothalamus result in release of oxytocin or ADH from posterior pituitary Control of Hormone Release: Hormonal Hormone produced by one endocrine gland (or hypothalamus) affects secretion of hormone by another endocrine gland • hypothalamus acts as overall coordinator releases regulatory hormones (releasing hormones or inhibitory hormones) affects anterior pituitary • anterior pituitary, when stimulated, secretes hormones that affect other glands (e.g., TSH [thyroid stimulating hormone] stimulates release of thyroid hormones from thyroid gland) Hormone Control - Misc. • nervous system can override normal endocrine control – e.g., in “fight-or-flight” response, sympathetic impulses result in release of epinephrine and norepinephrine from adrenal medulla --> increases blood glucose levels to maintain fuel supply during stress or exertion (overrules effect of insulin on blood glucose level)