Family Medicine Boston Health Net Inpatient
advertisement

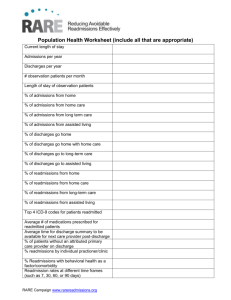
Family Medicine HealthNet Inpatient Service QUALITY REPORT AND UNIT DASHBOARD: BMC E6W QUEST: (QUALITY, EFFICIENCY, SATISFACTION AND TOTAL REVENUE) October 03, 2014 Leadership Team Christopher Manasseh, MD Assistant Professor Vice Chair for Inpatient and Hospital Services Aram Kaligian, MD Assistant Professor Assistant Inpatient Director Jonathan Bunker, BSN, RN Nurse Manager Eileen Mullaney, RN RN Care Manager Charlotte Cuneo, MSN, RN, CCAP Clinical Nurse Educator _______________________________________ Toyin Ajayi, MD Hospitalist Medical Director Director of Transitional Medicine Commonwealth Care Alliance Ted Constan Chief Administrative Officer, Department of Family Medicine Erica Cuevas, MPH Administrative Coordinator Gwyneth Jones, MBA Administrative Manager Brian Jack, MD Professor Chair, Boston University Department of Family Medicine Chief, Boston Medical Center Department of Family Medicine Jessica Martin, MA, MPH Program Director Introduction This is a Quality Report describing the activity of the Family Medicine - Boston Health Net (FM-HN) Inpatient Service located on 6W of BMC’s East Newton Campus. The purpose for this Dashboard is to document and share the quality of the service with senior leaders and other constituents FM-HN service accepts admissions from the family medicine practices at BMC and the CHCs and from the Boston Community Health Group (BCMG) which cares for high risk frail elders and disabled/homebound patients in our communities. As we continue with rapid PDSA (Plan-Do- Study- Act) cycles of improvement, and show improvement -- some graphic elements are dropped and are replaced by other priorities. Introduction These reports show areas in which we are doing well – and not so well – but that through this process we hope to continuously improve. The idea for collecting these data metrics emanated from the concepts of teamwork and the desire to provide high quality services among the partners. To begin, we organized a weekly meeting among the stakeholders designed to define the mission and the members of the team and to identify clear objectives that we would try to achieve. The principles of collaboration and objectives for the inpatient team are listed on a poster that hangs in the entry of the unit (shown on the next slide). The metrics developed that are shown in this report are an attempt to quantify each of these principles. The data are organized according to the BMC QUEST pneumonic (Quality, Efficiency, Satisfaction, Total Revenue). Principles of Collaboration for E6W Family Medicine, Boston HealthNet Inpatient Service Principles of Collaboration for 6 West Inpatient Unit Partners: Patients, Physicians, Nurses, Community Health Center Administration and Staff, Boston Community Medical Group, Physician Assistants, Consulting Services, Students, Nursing Education, Pharmacists, Physical and Occupational Therapists Environmental Services, Nutrition and Dietary and Community-based 1 providers including rehab units and SNFs Our Mission: To provide safe, high quality, evidence based, efficient, patient centered care at all times in an environment of collaboration and team work. Team Focused • Responsibility for care rests with a team of professionals rather than a single provider. • Patient Care is a shared responsibility • Team includes outpatient partners • Implement Teams training Clarity of Responsibility • The identity of the provider and the team responsible for each case will be clear to all staff at all times. Citizenship • Interactions among team members are respectful and collaborative at all times • Frequent physical presence on the floor will promote communication and collaboration High Efficiency • Promote early discharge • Team will work to minimize redundancy • The provider with the highest level of training should be caring for those patients who need the highest level of care. Evidence-Based Care Care provided will be: -- Based on the current best practices -- Be standardized among all providers -- Be informed by a rigorous CQI process Safe Transitions • Good communication at admission + discharge • All pts know how to care for themselves at dc • Implement ReEngineered Discharge Timely, High Quality Communication • Frequent communication is needed for safe provision of care • Board rounds each AM+PM • Nursing input at board + bedside rounds • Communication with primary care team • A dialogue among providers for each change in plan or patient transfer • Use of a standardized tool for handoffs • Use language that patients understand Maximize Continuity • Communicating with PCP is a priority • Information will flow smoothly from the ambulatory providers to the unit and from the unit to site of post hospital care. Acceptable Case Load • Safe patient care is possible only if there are well rested providers responsible for a reasonable number of patients • Acceptable daily work load Patient satisfaction • Is a responsibility of all team members • Is a key metric for quality • Family members are our customers Excellence in Education • All team members have responsibility for the education of residents, students and other trainees. • Nursing education is valued • All providers are responsible for orienting and teaching new members of the team about the appropriate management and flow on the floor. Good Documentation • There will be clear and consistent documentation of all care delivered • Will reconcile medications and care at all times • Health proxy and end of life care to be documented at all times QuEST The Family Medicine HealthNet Inpatient service uses QuEST, the BMC framework to measure outcomes QuEST stands for: Quality Efficiency Satisfaction Total Revenue QUALITY: Mortality Analysis For Family Medicine Attending Note Compliance for Non- Surgical Departments All-Cause 30-Day Readmission Rate 7 EFFICIENCY: Daily Workload by Care Team (Census Counted at 8am) Weekly Average Discharge Time Average Length of Stay Of Inpatient Discharges by Care Team Average Length of Stay Of All BMC Admissions Average Length of Stay Of Observation Discharges by Care Team Monthly Length of Stay (Observed/Expected Ratio) Average Length of Stay (Observed and Expected) Percentage of Patients Admitted to E6W Satisfaction: HCAHPS Quarterly Patient Experience Trends: E6W Communication Standards Total Revenue: Total Number of Patients Admitted and Discharged by Care Team Monthly Total Number of Patients Admitted by Care Team Average Total Admissions and Discharges by Day of Week Percent of Admissions and Discharges in Observation Status by Care Team Percent of All Admissions by Patient Class Patients Lost ◦ HealtHNet Patients’ Admissions For All Services ◦ Monthly Percentage of HealthNet Patients’ Admissions to FM-HN ◦ HealthNet Patients’ Admissions by Health Center ◦ CCA Patients Lost ◦ HealthNet Patients Lost to Cardiology Mortality Analysis for Family Medicine Medical MS-DRG Mortality Analysis for Family Medicine 2.50 Mortality Rate (%) 2.00 1.50 FM-HN continues to have Om < Em 1.00 0.50 0.00 Q1 2013 (N= 625) Q2 2013 (N=583) Q3 2013 (N= 575) Q4 2013 (N=609) Q1 2014 (N=576) Q2 2014 (N=581) Q3 2014 (N=596) Observed Expected Note: Discharges with non-viable neonates, or point of origin is hospice are excluded. Discharges from MICU to floor transfers are included. Q1 2013 (N= 625) % ICU Cases Source: UHC, Patient Outcomes Report 9.28 Q2 2013 (N=583) Q3 2013 (N= 575) 10.46 12.17 Q4 2013 (N=609) Q1 2014 (N=576) 11.82 Q2 2014 (N=581) 11.11 Q3 2014 (N=596) 10.15 9.06 Inpatient Mortality Index Mortality Index for Family Medicine 1.00 0.90 0.80 BMC wants to achieve a score of .77 or lower. FM has always been significantly lower than that. 0.70 0.60 0.50 0.40 0.30 0.20 0.10 0.00 Q1 2013 (N= 625) Q2 2013 (N=583) Q3 2013 (N= 575) Q4 2013 (N=609) Q1 2014 (N=576) Q2 2014 (N=581) Q3 2014 (N=596) Mortality O/E Source: UHC, Patient Outcomes Report Goal Case Mix Index Case Mix Index 1.45 CMI 1.35 1.25 1.15 1.05 0.95 Q1 2013 Q2 2013 Q3 2013 Q4 2013 Q1 2014 Quarter FM CMI FM Medicare CMI Note: Discharges with non-viable neonates, or point of origin is hospice are excluded. GIM CMI GIM Medicare CMI Q2 2014 Q3 2014 Attending Note Compliance for Non- Surgical Departments FM-HN attending continue to sign charts according to standard Source: BMC Administration All-Cause 30-Day Readmission Rate 30 Day All-Cause Readmission Rate for All Medical Services (May 2013-April 2014) Readmission Rate 35% 30% 25% 20% 18% 13.70% 15% 10% FM-HN has the lowest readmission rate among all the medical services. 5% 0% Medical Service Note: The attribution is based on the mortality analysis logic Source: BMC Administration- distributed at July 2014 Readmission meeting Readmissions All-Cause 30 Day Readmission 21.5 Readmission Rate (%) 19.5 17.5 15.5 13.5 11.5 9.5 Q1 2013 Q2 2013 Q3 2013 Q4 2013 Q1 2014 Quarter FM BMC GIM Q2 2014 Q3 2014 Daily Workload by Care Team (Census Counted At 8AM) Daily Workload by Care Team in November Average Daily Workload by are Team (at 8 am) 16 30 14 • 25 Number of Patients Number of Patients 12 10 8 6 4 20 15 7 5 5 10 5 6 4 11 11 10 9 10 10 5 9 10 9 9 June July August September 11 10 October November 2 0 0 11/1 11/3 11/5 11/7 11/9 11/11 11/13 11/15 11/17 11/19 11/21 11/23 11/25 11/27 11/29 Month Date FM 1 8 AM Census FM 2 (PA) 8 AM Census CCA 8 AM Census Source (both graphs): SDK Combined Census Report and confirmed with EPIC census on weekdays FM 1 FM 2 (PA) CCA • CCA volume peaked for a day, but then went back to average PA and FM team have the same average number of patients Weekly Average Discharge Time Weekly Average Discharge Time 16:48 Discharge Time 16:19 FM-HN continues to lead hospital in average discharge time. 15:50 15:21 14:52 14:24 13:55 13:26 Date FM-HN Entire Hospital Source: Weekly hospital reports (From Jonathan Bunker) Avg of H6E & H6W Total Number of Patients Admitted and Discharged in November by Care Team Total Number of Patients Admitted and Discharged in November by Care Team 120 110 112 100 Number of Patients 88 85 For FM team #admissions < # discharges 80 60 45 45 For PA team #admissions < # discharges 40 For CCA team #admissions= #discharges 20 0 FM 1 FM 2 (PA) Care Team Admissions Discharges Source: EPIC, Department of Medicine Admissions and DOM Discharges by Month report CCA Monthly Total Number of Patients Discharged by Care Team • Monthly Total Number of Patients Discharged by Care Team in November Number of Patients 300 45 250 47 200 50 45 36 3,500 128 150 106 89 94 112 100 50 FM-HN continues to maintain a constant volume about 8 admissions per day. 93 97 109 95 85 0 July August September October Month FM 1 FM 2 (PA) CCA November Observations Discharges Nox Eve 2694 2094 1494 3,000 1119 2,500 2,000 1162 1161 1,500 1,000 500 Source: EPIC, DOM Discharges by Month report Annual Volume 0 967 800 2028 300 222 206 387 AY12 AY13 260 198 0 AY14 Average Total Admissions and Discharges in November by Day of Week Average Total Admissions and Discharges in November by Day of Week 50 45 45 42 40 38 40 Number of Patients 35 35 37 • 42 36 32 32 28 30 • 25 23 25 30 20 • 15 10 5 0 Friday Saturday Sunday Monday Tuesday Wednesday Day of Week Admissions Discharges Source: EPIC, Department of Medicine Admissions and DOM Discharges by Month Report Thursday Monday and Tuesday had the highest number of admissions Monday and Tuesday had the highest number of discharges Monday and Tuesday were the busiest days in November Percent of November Admissions and Discharges in Observation Status by Care Team Monthly Percentage of Discharges in Observation Status by Care Team Percent of Admissions and Discharges In Observation Status in November 40% 50% 37.6% 35.2% 35% 26.7% 25% 22.2% Percentage 40% 30% Percentage The FM 1 team admitted < patients in obs status than it d/c 45% 35.5% 34.8% 35% 30% 25% 20% 15% 20% 10% 15% July August September October Month 10% FM 1 5% 0% FM 1 FM 2 (PA) CCA Care Team Admissions Discharges Source: EPIC, Department of Medicine Admissions and DOM Discharges by Month Report FM 2 (PA) CCA November The FM 9 (PA) and the CCA teams admitted > patients in obs status than it d/c Admissions in November by Patient Class Admissions in November by Patient Class 70% 66.3% 60% Percentage 50% 40% 33.7% 30% 20% 10% 0% Inpatient Observation Patient Class Source: EPIC, Department of Medicine Admissions 64.9% of all admissions were in inpatient status. Average Length of Stay of Inpatient Discharges in by Care Team (In Days) 4.95 5 4.05 3.85 4 3 3.28 2.62 5.2 4.9 4.6 4.3 4 3.7 3.4 3.1 2.8 2.5 June July August September October November Month 2.17 FM 1 2 1 0 FM (n=53) FM 2 (PA) (n=73) CCA (n=35) Care Team Mean Median Source: EPIC (From DOM Discharges by Month report) Average Length of Stay (In Days) Average Length of Stay (In Days) 6 Average Length of Stay (In Days) Average Length of Stay of Inpatient Discharges in November by Care Team (In Days) Monthly Length of Stay of Inpatient Discharges by Care Team Based on the Mean (In Days) FM 2 (PA) CCA Monthly Length of Stay of Inpatient Discharges by Care Team Based on Median (In Days) 4.5 3.5 2.5 1.5 June July August September October Month FM 1 FM 2 (PA) CCA November Based on Mean- CCA has always had a longer ALOS and the ALOS for CCA, and FM 1 increased since October Based on Median- CCA usually has a higher ALOS but was similar to FM1 and FM 1 in August and September ALOS for FM 1 increased since October Average Length of Stay of Inpatient admissions in October by Day of The Week (In Days) FROM DATE OF ADMISSION FROM DATE OF DISCHARGE Average Length of Stay of Inpatient Admissions in November for FM-HN Service (In Days) Average Length of Stay of Inpatient Discharges in November for FM-HN Service (In Days) 5 5 6 5.5 4.5 3.5 3 3.4 2.9 2.9 2.8 2.5 2.6 3.4 3.3 2.9 2.4 3.3 2.6 2.1 2 1.5 4 3.8 4 3 5 4.7 5 3.6 ALOS (In Days) ALOS (In Days) 4 People admitted on Wednesday, Thursday and Saturday have a longer LOS and people admitted on Sunday and Monday have a shorter LOS 2.4 2.8 4.2 2.6 2.1 2 3 2.8 1.8 2 1 1 0.5 0 Friday 0 Friday Saturday Sunday Monday Saturday Tuesday Wednesday Thursday Sunday Monday Day of Week Day of Week Mean Mean Median Source: EPIC (From Department of Medicine Admissions and DOM Discharges by Month report) Median Tuesday Wednesday Thursday People discharged on Friday, Sunday, and Monday longer LOS & people discharged on Saturday and Tuesday have a shorter LOS Average Length Of Stay by Day of Discharge in September ALOS by Day of Discharge in September 8.5 ALOS (In Days) 7.5 FM-HN ALOS is always lower than the ALOS for BMC and 6.5 5.5 4.5 3.5 2.5 Sunday Monday Tuesday BMC Source: UHC, Patient Outcomes by Discharge Day Wednesday Day of Week FM-HN Thursday GIM Friday Saturday Average Length of Stay of Observation Discharges in November by Care Team (In Hours) 30 25 29.5 28.47 27.04 24.5 22.6 21.9 20 15 Monthly Average Length of Stay of Observation Discharges by Care Team Based on the Mean (In Hours) 50 45 40 35 30 25 20 Based on the Mean- the ALOS for all three teams decreased since October June July August September October November Month FM 1 FM 2 (PA) CCA 10 Average Length of Stay of Observation Discharges by Care Team Based on the Median (In Hours) 5 0 FM (n=32) FM 2 (PA) (n=39) CCA (n=10) Care Team Mean Median Source: EPIC , DOM Discharges by Month report Average Length of Stay (In Hours) Average Length of Stay (In Hours) 35 Average Length of Stay (In Hours) Average Length of Stay of Observation Discharges in October by Care Team (In Hours) 45 35 25 15 June July August September October Month FM 1 FM 2 (PA) CCA November Based on the Median- the ALOS for CCA and FM 2 decreased but slightly increased for FM 1 Average Length of Stay of Observation Admissions in October by Day of The Week (In Hours) ALOS FROM ADMISSION DATE ALOS FROM DISCHARGE DATE Average Length of Stay of Observation Admissions in November for FM-HN Service (In Hours) Average Length of Stay of Observation Discharges in November for FM-HN Service (In Hours) 60.7 40 60 35 30 40 30 26.8 26.3 37.9 34.4 29.6 36.4 25.9 22.2 19.3 20 23.5 29 21 21.4 ALOS (In Hours) ALOS (In Hours) 50 34.7 31.9 31.2 25 27.1 23.7 23.922.7 25.1 22.2 23.7 26.9 24 28.2 18.6 20 15 10 10 5 0 Friday Saturday Sunday Monday Day of Week Mean Tuesday Wednesday Thursday Admissions on Friday and Sunday have a longer LOS and admissions on Thursday and Monday have a shorter LOS 0 Friday Saturday Median Source: EPIC (From Department of Medicine Admissions and DOM Discharges by Month report) Sunday Monday Day of Week Mean Median Tuesday Wednesday Thursday Discharges on Monday and Tuesday have a longer LOS and discharges on Sunday, Saturday and Wednesday have a shorter LOS Comparing ALOS for Inpatient and Observation Admissions in October: With and Without the CCA team OBSERVATION ADMISSIONS INPATIENT ADMISSIONS Average Length of Stay (In Days) 4 3.9 3.9 3.8 3.7 3.6 3.6 3.5 3.4 3.3 3.2 3.1 Comparison of Average Length of Stay of Observation Admissions in November Average Length of Stay (In Hours) Comparison of Average Length of Stay of Inpatient Admissions in November 28.20 28.19 28.18 28.15 28.16 28.14 Obs ALOS is .04 hours less when CCA is excluded 28.12 28.10 28.08 28.06 28.04 28.02 28.00 3 FM 1, FM 2 (PA), CCA FM 1 & FM 2 (PA) Care Teams Note: ALOS is based on mean Inpt ALOS is .3 hours less when CCA is excluded FM 1, FM 2 (PA), CCA Care Team FM 1 & FM 2 (PA) Percentage of Patients Admitted to E6W Percentage of Patients Admitted by FM-HN in November by Floor Percentage of Patients Admitted to E6W 100.0% E6W 90.0% 88.7% 89.6% 84.0% 87.7% 83.0% 80.0% E7E E7N 70.0% 60.0% 50.0% E7W E8E 40.0% 30.0% 20.0% E8W 87.7% 10.0% 0.0% July August September % admitted to E6W Source: EPIC, Department of Medicine Admissions October Goal November In November FM-HN admitted about 88% of patients to E6W. The percentage of Admissions to E6W has increased since October Percentage of Patients Discharged from E6W Percentage of Patients Discharged From E6W Percentage of Patients Discharged From FM-HN by Floor 100% 90% E6W 80% 70% E7N E7W E8E Percentage E7E 60% 50% 40% 30% 20% 88.0% E8W 10% 0% November December Month HCAHPS: Quarterly Patient Experience Trends: BMC & E6W Recommended Hospital 100 90 80 70 Rate (%) 60 E6W had a higher percentage for recommending the hospital 50 40 30 20 10 0 2012 Q4 2013 Q1 2013 Q2 (n=159, 13) 2013 Q3 (n=158, 7) 2013 Q4 (n=291, 20) 2014 Q1 (n=431, 39) 2014 Q2 (n=422,44) 2014 Q3 (n=411, 36) BMC Note: The percentage presented in these graphs are the top box score percentages Source: BMC Administration (From Inpatient Dashboard) 6W Target HCAHPS: Quarterly Patient Experience Trends: BMC & E6W Communication with Nurses Communication with Doctors 100 100 90 90 80 80 70 60 Rate (%) Rate (%) 70 50 40 60 E6W had a lower score than BMC for communication with nurses and communication with doctors 50 40 30 30 20 20 10 10 0 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 (n=159, (n=158, 7) (n=291, 13) 20) BMC 6W 2014 Q1 2014 Q2 2014 Q3 (n=431, (n=422,44) (n=411, 39) 36) Target Note: The percentage presented in these graphs are the top box score percentages Source: BMC Administration (From Inpatient Dashboard) 0 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 2014 Q1 2014 Q2 2014 Q3 (n=159, 13) (n=158, 7) (n=291, 20) (n=431, 39) (n=422,44) (n=411, 36) BMC 6W Target HCAHPS: Quarterly Patient Experience Trends: BMC & E6W Response of Hospital Staff Pain Management 100 100 90 90 80 80 70 60 Rate (%) Rate (%) 70 50 40 60 E6W had a lower score than BMC at both responsible of hospital staff and pain management 50 40 30 30 20 20 10 10 0 0 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 2014 Q1 2014 Q2 2014 Q3 (n=159, 13) (n=158, 7) (n=291, 20) (n=431, 39) (n=422,44) (n=411, 36) BMC 6W Target Note: The percentage presented in these graphs are the top box score percentages Source: BMC Administration (From Inpatient Dashboard) 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 2014 Q1 2014 Q2 2014 Q3 (n=159, 13) (n=158, 7) (n=291, 20) (n=431, 39) (n=422,44) (n=411, 36) BMC 6W Target HCAHPS: Quarterly Patient Experience Trends: BMC & E6W Discharge Information 100 100 90 90 80 80 70 70 60 60 Rate (%) Rate (%) Communication about Medicines 50 40 50 40 30 30 20 20 10 10 0 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 2014 Q1 2014 Q2 2014 Q3 (n=159, 13) (n=158, 7) (n=291, 20) (n=431, 39) (n=422,44) (n=411, 36) BMC 6W Target Note: The percentage presented in these graphs are the top box score percentages Source: BMC Administration (From Inpatient Dashboard) E6W had a lower score than BMC for both communication about medicines and discharge information 0 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 2014 Q1 2014 Q2 2014 Q3 (n=159, 13) (n=158, 7) (n=291, 20) (n=431, 39) (n=422,44) (n=411, 36) BMC 6W Target HCAHPS: Quarterly Patient Experience Trends: BMC & E6W Quietness of Hospital Environment 100 100 90 90 80 80 70 70 60 60 Rate (%) Rate (%) Cleanliness of Hospital Environment 50 40 30 E6W had a slightly higher score than BMC for cleanliness but had a lower score for quietness 50 40 30 20 20 10 10 0 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 2014 Q1 2014 Q2 2014 Q3 (n=159, 13) (n=158, 7) (n=291, 20) (n=431, 39) (n=422,44) (n=411, 36) BMC 6W Target Note: The percentage presented in these graphs are the top box score percentages Source: BMC Administration (From Inpatient Dashboard) 0 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 2014 Q1 2014 Q2 2014 Q3 (n=159, 13) (n=158, 7) (n=291, 20) (n=431, 39) (n=422,44) (n=411, 36) BMC 6W Target Communication Standards Percent of Patient's PCPs Contacted Upon Admisison and Discharge 100% 95% 96% 90% 80% Percentage 70% 60% 50% About 91% of PCPs are contacted upon admission and 95% upon discharge 40% 30% 20% 10% 0% November '13 December '13 January '14 February '14 March '14 April '14 May '14 June '14 July '14 August '14 Month % of PCPs contacted at Admission Source: Communications Excel Tracking Sheet Percentage of PCPs Contacted at Discharge September '14 October '14 November '14 Patients Lost ◦ HealtHNet Patients’ Admissions For All Services ◦ Monthly Percentage of HealthNet Patients’ Admissions to FM-HN ◦ HealthNet Patients’ Admissions by Health Center ◦ HealthNet Patients Lost to Cardiology HealthNet Patients’ Admissions for ALL Services In October HealthNet Patient's Admissions to FM-HN Service 70% HealthNet Patient's Admissions in November 23.60% 2.20% E Card Gen 9.60% E Card CHF Percentage 7.80% 60% 62% 57% 56% August September 57.1% 50% 40% 30% 20% 10% Medical Services 0% October November Month FM-HN ED Obs Unit 57.10% About 57% of HealthNet patients were admitted into the FM-HN Service in November Source: Individual SDK Inpatient and Observation admissions by Health Center report Note: This graph includes patients with a PCP in Family Medicine Yawkey Goal: ?? HealthNet Patients’ Admissions In October by Health Center South Boston (44) Greater Roslinale (1) Yawkey ACC (52) 0.6% 6.8% 7.7% 6.8% 9.1% 19.2% 67.8% 77.3% 100% Dorchester (36) Geiger/Neponset (6) Upham's Corner (39) 7.7% 11.1% 5.1% Medical Teams 8.3% 33.3% ER 20.5% 13.9% 66.7% FM-HN loses the least patients from Geiger/Neponset, Mattapan, South Boston,and East Boston (n>5) 66.7% Source: Individual SDK Inpatient and Observation admissions by Health Center report 66.7% FM-HN Cardiology HealthNet Patients’ Admissions In October by Health Center (Cont.) East Boston (88) Codman Square (39) Mattapan (26) 7.7% 11.4% 11.5% 12.8% 7.7% 10.2% 62.5% 50.0% 53.8% 15.9% 25.6% 30.8% Harvard St. (13) Whittier St. (23) 17.4% 23.1% 4.3% South End (1) Manet (3) 33.3% FM-HN loses the most patients from Whittier, Roslindale, and Harvard Medical Teams 33.3% ER 38.5% 47.8% FM-HN 15.4% Cardiology 30.4% 23.1% 33.3% 100.0% Source: Individual SDK Inpatient and Observation admissions by Health Center report APPENDIX Variability in staffing patterns, operations, and processes results in significant differences in discharge timing Service Cath Lab Family Medicine – PA EP Ambulatory Surgery Surgical Subspecialty Neurology Pediatric Surgery Maternity Family Medicine – Resident Newborn General Surgery Medicine – Hospitalist Gynecology ED OBS CHF ID Medicine – Resident Oncology General Neurology General Cardiology Renal General Pediatrics Geriatrics Average discharge time 1:22:41 PM 1:40:15 PM 1:41:27 PM 1:42:00 PM 2:20:02 PM 2:34:41 PM 2:40:00 PM 2:42:19 PM 2:46:47 PM 2:47:40 PM 2:48:13 PM 2:49:41 PM 3:05:39 PM 3:07:57 PM 3:15:15 PM 3:17:36 PM 3:22:59 PM 3:27:45 PM 3:31:36 PM 3:50:23 PM 4:01:25 PM 4:11:13 PM 4:12:30 PM Average daily discharges 1.2 4.9 0.5 2.0 10.1 0.4 0.6 8.0 3.7 5.7 8.7 6.4 1.7 4.9 1.9 2.9 11.0 2.1 2.4 3.1 2.8 5.2 3.3 Average discharge time: 2:58 PM Advancing all these teams to the current mean would save a total of 25.6 bedded patienthours each day. 30 Day All-Cause Readmission by Service Service ENP HEM/ONC ENP RENAL E PULMONARY IP E VASCULAR SURGERY E CARDIOLOGY CHF MP TEAM 3 MP TEAM 5 ENP 2 MP GERIATRIC IP MP TEAM 6 MP TEAM 4 E TRANSPLANT MP TEAM 2 MP TEAM 1 H MEDICU ENP 1 E INTERNAL MED IP H REHAB CENTER BMC ENP FM E CARDIOTHORACIC SURGERY ENP PA E CARDIOLOGY GENERAL E CCU Note: Services with less than 30 index cases are excluded. Den Num 712 224 711 210 52 12 256 59 576 127 774 161 449 89 230 45 824 149 372 66 796 138 76 13 738 126 742 125 132 22 264 43 388 61 80 12 735 103 437 60 1042 143 682 93 327 39 30 Day All-Cause Readmission Rate (%) 31.46% 29.54% 23.08% 23.05% 22.05% 20.80% 19.82% 19.57% 18.08% 17.74% 17.34% 17.11% 17.07% 16.85% 16.67% 16.29% 15.72% 15.00% 14.01% 13.73% 13.72% 13.64% 11.93% Lack of clinical practice standardization across services results in variable LOS for patients with similar DRGs … LOS for Observation admissions with primary diagnosis of non-specific chest pain Average hours Source: SDK dataset, 8/1/2013-1/31/2014.