Quiz 5 - Squarespace
advertisement

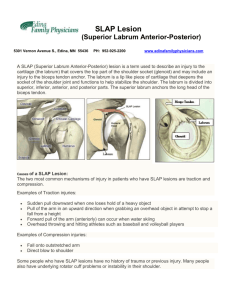
MS Study Guide #5: Shoulder Shoulder pathologies are a common and disabling condition Chronic shoulder impingement results in significant functional disability and reduction in the QOL Shoulder Complex o GH joint o AC joint o SC joint o Scapulo-thoracic ROM o Flexion: 0-180 o Abduction: 0-180 o IR: 0-70 o ER: 0-90 o Extension: 0-60 Capsular pattern: most limited in ER, less of abduction, least of IR Anatomy o Humerus is larger than glenoid fossa o SLAP lesion: biceps involvement and superior labrum o Codman’s paradox: cardinal plane movements cause external rotation (conjunct rotation) Why? can work in more confortable range (ER) to address flexion o Inferior adhesion: stiffness of the inferior capsule (the hammock) o Scapula: many force couples at the GH joint Importance of the rotator cuff because it keeps the humeral head in the socket o Clavicle and SC joint: Elevation: inferior glide at the SC joint Retraction: posterior glide at SC joint Protraction: anterior glide at the SC joint SC: frees up 10 degrees of motion in the GH joint Do not forget about it Subacromial space: 7 to 12 mm of space with arm at side Lose 50% when get to 90 degrees of abduction AC joint Posterior medial superior Posterior superior Posterior lateral superior Subacromial bursa: communicates with capsule through gap in the capsule Significance: weak points can cause laxity o Chronic bursitis: collagen due to chronic inflammatory response can get into capsule and cause adhesive capsulitis Need to look at capsule with recurrent bursitis Instability Instability: excessive displacement of humeral head in relationship to the glenoid Two types: names on the mechanism, directionality, and preferred method of treatment o TUBS: traumatic unilateral (anterior) bankart surgery Younger the patient the higher the likelihood Will require surgery to stabilize Bankart 3-6 o’ clock This lesion is seen in over 85% of cases after a traumatic anterior dislocation Bankart lesion: avulsion of the labraligamentous complex from the anteroinferior aspect of the glenoid, with complete disruption of the scapular periosteum The presences of an associated glenoid rim fracture is termed an osseous bankart lesion Hill Sach Lesion: a radiological finding a osteochondral compression defect/fracture of posterior humeral head o It is caused by a traumatic translation of the posterior humeral head over the sharp anterior lip of the glenoid rim Special Test Apprehension test Clunk test I, II Crank test o o Recurrence Rate Dislocation of the GH joint is notorious for its high rate of recurrence Recurrence rates have range from 47% to 100% Not as active once older so recurrence rate is lower Immobilization following dislocation For over 2000 years since the era Hippocrates, physician have immobilized the arm to the trunk (position of adduction and internal rotation) hoping to prevent recurrence Land mark paper: immobilization will not change the rate of recurrence o Immobilization of the arm in ER better approximates the bankart lesion to the glenoid neck than does conventional position of IR Treatment o Acute PRICE, Codman’s, NSAIDs, referral to rule out bony lesion, o Subacute: pain free ROM, strengthening-isometrics, PNF, scapular stabilizers, weight bearing for dynamic stabilization Surgery: Bankart Surgery; 3 o clock to 6 o clock AMBRII: atraumatic multidirectional bilateral rehab inferior capsular shift and rotator interval closure Patients will usually have secondary impingement like symptoms; usually due to laxity but will come to clinic with pain Rotator interval A gap exists between the anterior edge of the supraspinatus tendon and the superior edge of subscapularis tendon; this gap is the rotator interval Through this gap run the long head of the biceps tendon, from its origin on the supraglenoid tubercle of the scapula and the coracohumeral and superior GH ligaments Primary Impingement Compressive cuff problem Need to look a inferior capsule: usually limited which keeps humeral head elevated and decreases subacromial space Could have pain with contraction or lengthening MSTT/MMT: pain with abduction, ER, IR, flexion ST: empty can, Hawkins/kennedy, Neers P4T: pain along biceps or subacromial space Supraspinatus: has poor blood flow along the MTJ; not set up to heal well Excessive add during sleeping; place pillow under arm to avoid stretching the tendon (loose pack) Neers Classification of impingement Stage I o Edema and hemorrhage o Less than age 25 Stage II o Fibrosis and tendonitis o Age 25-40 Stage III o Bone spurs and tendon rupture o Greater than age 40 Acromial Morphology Requires an Outlet view x-ray to confirm o Type I- flat o Type II- smooth curve o Type III- anterior hook Special Tests Impingement Neer test Hawkins-kennedy Cross over test Yocum Test Rehabilitation of primary impingement Treat the cause of the problem o o o Treat hypomobility Therex NM dynamic stability Functional exercise Conservative management of impingement and prognosis (study) Type I acromian- 91% success rate Type II and III- 66% success rate Physical therapy successful in the first six weeks If physical therapy is unsuccessful: SAD Secondary Impingement Secondary to instability or hypermobility Abnormal GH translation usually anterior occurs This abnormal motion causes irritation to the anterior capsule, subscap, and supraspinatus tendon Additional ST should be performed to differentiate between primary and secondary impingement by assessing capsular mobility ST instability Sulcus sign at 0 degrees Sulcus sign at 90 degrees Anterior load and shift Posterior load and shift Jobe relocation test Rehabilitation of secondary impingement Should focus on o Dynamic stability o Proprioceptive/kinesthetic training o NM reactive training o Functional rehabilitation Rotator Cuff Tears Special tests rotator cuff tears ER lag signs IR lag sign Internal impingement-Posterior Posterior internal impingement has been purposed as the likely cause of pain when the shoulder is in an abducted and ER Injuries to the undersurface of the RC and the posterior superior labrum are thought to occur as these areas make contact First described in 1992 Pain is typically felt in the posterior aspect of the shoulder at the end of the cocking phase of throwing mechanics Contributing factors include posterior capsular tightness and GIRD The total arc motion from end range ER to end range IR is 180 degrees For every degree of ER that is gained, a degree of IR can be lost without affecting the function of the throwing shoulder Lecture #3 7/15/15 AC Joint Description: disruption of the ligamentous integrity of the AC joint o The AC ligament may be damage with excessive posteriorly directed translatory or rotary force o The coracoclavicular ligaments (conoid and trapezoid) may be damaged with excessive superiorly or anteriorly directed forces Etiology: the cause is generally traumatic such as a fall directly on the shoulder with the arm adducted or a fall on an outstretched hand Classification o Type I: Type I AC separations occur secondary to a mild force to the point of the shoulder, which produced a minor strain to the fibers of the AC ligaments The AC joint remains stable, and the ligaments are intact On physical examination, AC joint tenderness is minimal to moderate without palpable deformity o Type II: AC separations result from a moderate force to the point of the shoulder, severe enough to rupture the AC ligaments the distal end of the clavicle is unstable, but the coracoclavicular ligaments are intact o the scapula may rotate medially, widening the AC joint if the coracoclavicular ligament is mildly stretched, slight downward displacement of the scapula from the distal end of the clavicle may be apparent on physical examination, pain at the AC joint can be moderate to severe. The outer end of the clavicle may be slightly superior to the acromion shoulder motion produces pain in the joint and the coracoclavicular space is tender manipulation of the clavicle in the horizontal plane may result in subtle motion detectable with palpation of the AC joint Type III Disruption of the AC and CC ligaments occurs after a severe force is applied to the point of the shoulder The deltoid and trapezius muscles are disrupted from the distal end of the clavicle, or the periosteal sleeve with muscle attachments may be separated from the outer end of the clavicle On physical examination, this may be less painful but unstable Patient will present with a depressed UE compared with the normal shoulder, and the distal end of the clavicle may be prominent enough to tent the skin o Treatment Physical Agents External devices Taping, splinting, orthotics Sling Supervised neglect Therapeutic exercises Re-injury prevention instruction Surgery if IV, V, VI Subacromial bursitis Best exam steps: P4T, MLT, MSTT Etiology: inflammation of this bursa is most commonly the result of repetitive strain, or overuse, injury to other structures like the rotator cuff o Rarely occurs alone and is usually associated with supraspinatus tendinitis, or tenosynovitis of the rotator cuff, bicipital muscles, or GH arthritis Historical findings o Diffuse shoulder pain o Pain at rest o Recent unaccustomed repetitive use of UE Common presentation o Pain with all shoulder movements o Symptoms are reproduced/increased with palpation of subacromial bursa Adhesive capsulitis Common presentation o Lateral shoulder pain: worsens with positions or activities which put stretch on the GH joint o Progresses to stiffness o Gradual, usually insidious, onset of symptoms o Patients with DM, thyroid, middle age women, non dominant, o Many times when a patient presents to the MD with shoulder stiffness the patient is automatically labeled with a frozen shoulder o If the patient improves quickly, the patient does not have a true frozen shoulder o The true frozen shoulder is difficult to treat and slow to recover o Self limiting disorder lasting approximately 30 months o Supervised neglect had a better outcome measure than aggressive PT Epidemiology o Primary (idiopathic) Higher frequency in women vs. men More common in non-dominant arm Age range 40-60 12% bilateral o Secondary DM Trauma CNS involvement Upper limb immobilization Three stages o Freezing (Painful)- average duration 6 months Contraindications: US o Frozen (stiff)- average duration 8 months o Thawing (resolution)- average duration 14 months o The length of the painful period corresponds to the length of the recovery period Lecture #4 7/17/15 S.L.A.P Superior, labral, anterior, posterior Anatomy o The biceps tendon inserts directly into the most superior position of the labrum o The labrum configuration and histology resembles that of the meniscus in the knee o The superior and middle GH ligaments usually attach to the anterior superior labrum, which in turn attaches to the glenoid rim o The superior and anterosuperior portions of the labrum are less vascular than the remainder of the labrum o 10-2 o’clock two mechanisms of injury o traumatic superior compression fall or direct blow to the shoulder the shoulder is typically positioned in an abducted and slightly forward-flexed position during the fall Inferior traction Dislocation/subluxation Lifting heavy object o repetitive overhead activities eccentric deceleration in the deceleration phase of pitching, the biceps muscle fires to stop the elbow from hyperextending, which causes a force to be placed across the labrum peel back mechanism when the shoulder is placed in a position of abduction and maximal ER, the rotation produces a twist at the base of the biceps, transmitting a torsional force to the anchor Type I o Characterized by degenerative fraying of the superior labrum with the edge still firmly attached to the glenoid o Intact biceps anchor Type II- the most common o Detachment of the superior labrum and biceps tendon from the glenoid o Destabilization of the biceps anchor Type III o Bucket-handle tear of the superior labrum o The central portion of the tear is displaced into the joint o The remaining labrum and biceps anchor are stable Type IV o Bucket-handle tear of the superior labrum with extension into the biceps tendon Clinical presentation o History- the patient may or may not relate a specific event to the onset of symptoms Patient complained can range from instability to a vague ache in the shoulder The most common complaint is deep shoulder pain localized to the anterosuperior shoulder associated with overhead use of the extremity In addition to deep shoulder pain, symptoms of clicking, catching, or popping are commonly described The problem with diagnosing a SLAP lesion is that it is usually found in combination with either impingement or instability What do these special tests tell us o The problem with diagnosing a SLAP lesion is that is usually found in combination with either impingement or instability o Current research is looking to increase sensitivity and specificity of these tests by SLAP classifications Imaging o X-ray- will not help disclose possible intraarticular pathology o CT Arthrograpy: better for detecting bone abnormalities o MRI- labral lesions Good study for identifying labral lesions with decreased sensitivity in identifying superior lesions when compared to middle and inferior labral lesions MRI with contrast dye was developed to improve the ability to detect superior lesions Treatment o Overall, non-operative management has proven unsuccessful for a large number of patients with unstable SLAP lesions o Surgical intervention: the 2 major ways the SLAP lesions can be treated are by debridement and repair SLAP I/III- debridement SLAP II/IV- repair Outcomes o Early studies demonstrated only short-term improvement after isolated arthroscopic labral debridement of unstable SLAP lesions with deteriorating outcomes over time o This failure is probably because the underlying instability was not addressed Surgical intervention o The surgical treatment of a SLAP lesions has undergone a considerable evolution because of advanced in arthroscopic techniques and instrumentation o The current approach to address unstable SLAP lesions favors surgical repair Rehabilitation o Following all SLAP surgeries, the rehabilitation plays an integral part in the patients outcome o While protocols with differ among surgeons, we must appreciate postoperative precautions for repairs Postoperative precautions SLAP II/IV repair o Typical protective phase is 6 weeks Protected biceps contraction No active shoulder flexion No resistance to elbow flexion or supination Protected biceps stretch Avoid shoulder extension/hand behind back movements Caution with ER Week 0-2: 0-10 /15 degrees ER at 0 degrees of abduction 3-4- 0-25/30 degrees ER at 35 degrees of abduction 5-6: 0-45/50 degrees ER at 45 degrees of abduction at week 6: begin light and gradual progression of ER at 90 degrees of abduction general goals SLAP II/IV o full ROM by 10-12 weeks postoperatively o return to interval throwing program by 20-24 weeks provided adequate strength base and MD approval Postoperative guidelines SLAP I/III debridement o The debridement procedures do not require the same lengthy protection phase associated with a repair o Precaution-no biceps strengthening including isometrics for one week postoperatively o Gradual progression beginning with ROM and progressing to strengthening over the first month with expected return to activity within 2-3 months Suprascapular neuropathy Diagnosis o Vague posterior shoulder pain, weakness and fatigability Weakness/atrophy without pain often suggests compression at spinoglenoid notch (nerve purely motor beyond this) o Symptoms may mimic rotator cuff pathology or instability o Exam reveals rotator cuff weakness (supra-infraspinatus) o MRI may exclude RTC, demonstrate atrophy and or reveal a ganglion or space-occupying lesion- if present, strongly consider surgical excision o NCS/EMG may assist with the diagnosis Treatment o Typically begin with non-operative management o Rest/rehab depending on the suspected etiology o o o o Rest from repetitive hyperabduction NSAIDs and corticosteroid injections considered Symptoms often resolve, allowing full return to athletics, but atrophy may persist Non-responders may benefit from a spinoglenoid notchplasty, transverse scapular ligament release, nerve decompression or surgical exploration Erb’s Palsy Brachial plexus injury Involved the segments innervated by C5 and C6 nerve roots Approximately 1-2 babies in 1,000 suffer brachial plexus injuries at birth and 1 in 10 will require treatment Presentation o The limb is extended at the elbow Loss of biceps, brachialis, and brachioradialis o The limb is adducted Loss of deltoid and supraspinatus o The limb is internally rotated Loss of infraspinatus and teres minor Klumpke’s Paralysis Brachial plexus injury Involved the segments innervated by C7, C8, T1 Usually manifests in the newborn period as weakness restricted to or mainly involving the hand