2013 Research Study
advertisement

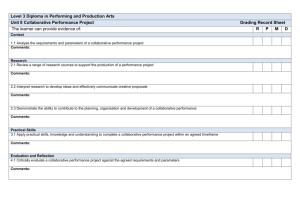
Session A2b October 11, 2013 Providing Care for Children and Adolescents with Complex Medical, Psychological, and Developmental Problems: A Collaborative Model Mary Rineer, Ph.D.; Kathleen Shepherd Koljack, MD; Michael J. Sannito, Ph.D.; and Danny W. Stout, Ph.D. www.capesinc.org Faculty Disclosure We have not had any relevant financial relationships during the past 12 months. Learning Assessment A learning assessment is required for CE credit. Attention Presenters and Attendees: Please incorporate audience interaction through a brief Question & Answer period during or at the conclusion of your presentation. This component MUST be done in lieu of a written pre- or post-test based on your learning objectives to satisfy accreditation requirements. Presentation Objectives Describe a model of collaborative multidisciplinary care appropriate for complex cases. Describe the development and implementation of the collaborative multidisciplinary model. Identify and discuss research models which can be utilized with collaborative care and approaches to measure and document benefits to patients. Describe both advantages and challenges of this model of care and discuss solutions utilized for common challenges when implementing the collaborative model. The Agenda for Today’s Presentation I. The Problem II. The Collaborative Process III. The Data IV. The Future I. The Problem • Children and adolescents who present to Health Care Providers with moderate to severe problems in two or more areas of development pose a significant problem for the Health Care Provider! • The problem which this creates for the Health Care Provider is created by a service delivery design which does not encourage or establish a format for collaboration among providers. I. The Problem • Half of “well-care” appointments in primary pediatrics involve behavioral concerns. (Cassidy & Jellinek, 1998) • Pediatricians may feel unprepared to accurately diagnose behavioral problems and treat complex problems that may necessitate both pharmacologic and behavioral interventions. ( Williams, Klinepeter, Palms, Pulley, & Foy, 2004) I. The Problem • Health care providers more readily identify and treat attentiondeficit/hyperactivity disorder than anxiety, depression and conduct disorder. ( Williams, Klinepeter, Palms, Pulley, & Foy, 2004) Essentials of the Problem Very complicated patients Problems are interwoven-no clear referral pattern-doesn’t fit the “medical model” No clear format for addressing the problem No common language-doctors don’t speak “Psychologist” or “Occupational Therapist” No “captain of the ship” for these patients No algorithm We need to build competency and comfort in our pediatricians around these diagnoses The Problem: An Ineffective Delivery System In the past parent driven or based on referral of an HCP (Health Care Provider)… • Fragmented • Variable outcomes • Limited by perspective of the service provider • Lack of awareness of available community resources • Limited financial resources • Limited communication between HCP in multiple fields • Limited interaction between psychiatric services, regarding outcomes of medication in a variety of settings Benefits of CAPES Program • Integrated • Coordinated • Consistent, evidenced-based outcomes • Dynamic perspective of multiple service providers • Awareness of available community resources • Maximizing utilization of limited financial resources • Consistent communication between HCP in multiple fields • Consistent interaction between multiple providers and outcomes observed in a variety of situations • Integrated assessment of family dynamics related to the child/adolescent The Collaborative Process • Recruiting Team Members to be part of the process: • Start with individuals with whom you already have a practice relationship. • Emphasize the efficiency of the process that designs a treatment plan and a way to implement it and follow progress. III. The Data • 10% to 20% of youths meet diagnostic criteria for a mental health disorder, and many more are at risk for escalating problems with long-term individual, family, community, and societal implications (Kataoka, Zhang, & Wells, 2002) • Estimates are that 25% of the 150 million child visits per year for primary health care (non-mental health and other specialties) have a psychological problem associated with the presenting problem (Woodwell, 2000) III. The Data from CAPES • It was hypothesized that the effectiveness of the CAPES program would be manifested in significant lower post-test scores on the Child Behavior Checklist. • Initial nonparametric analysis using the Wilcoxon SignRank test found significant differences in the domains of ADHD, OD and Conduct (p < 0.05), and marginal significance for Affective (p = 0.06). • This initial analysis did not account for the reason of referral and utilized non-parametric tests of significance. • Follow up tests accounting for referral reason and utilizing the Student’s t-test were planned. III. The Data from CAPES • Follow up tests accounting for referral reason and utilizing the Student’s t-test found significantly lower post-test scores in all domains with the exception of Somatic, meeting all statistical assumptions. • Affective, t(17) = 3.80, p = .001 • Anxiety, t(17) = 3.02, p < .001 • ADHD, t(15) = 5.14, p < .001 • Oppositional Defiant, t(22) = 2.50, p < .001 • Conduct, t(17) = 4.01, p < .001 • Somatic (t(8) = 1.94, p = .088 Box & Whisker Plot Pre_ADHD vs. Post_ADHD Include condition: v24 = "X" and v25 <> 999 and v26 <> 999 and v27 > -100 and v27 < 100 13 12 11 10 9 8 7 6 5 Pre_ADHD Post_ADHD Mean Mean±SE Mean±1.96*SE Box & Whisker Plot Pre_Conduct vs. Post_Conduct Include condition: v32 = "X" and v33 <> 999 and v34 <> 999 and v35 > -100 and v35 < 100 11 10 9 8 7 6 5 4 3 2 Pre_Conduct Post_Conduct Mean Mean±SE Mean±1.96*SE IV. The Future • Dynamic Long Term Results • Service delivery model that maximizes the utilization of available • • • • • • technology and expertise Develop a hierarchy of family needs in order to optimize treatment strategies which evolve as the child develops Provide informational exchange between participants Facilitate communication among parents and providers Develop understanding of the service delivery system Integrate decision making to enable a comprehensive and collaborative series of recommendations Develop standardized tools to communicate and document change including: intake, case history, release of information and progress updates and discharge reports IV. Charting the Future • CAPES Procedure Steps • Intake Form • Assessment Instruments • Secure Website • CAPES Team Notes and Care Recommendations • Care Plan Sample References Williams, J., Klinepeter, K., Palmes, G., Pulley, A., & Foy, J.M. (2004). Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics, 114, 601-606. doi: 10.1542/peds.2004-0090 Kataoka, S. H., Zhang, L., & Wells, K.B. (2002). Unmet need for mental health care among U.S children: Variation by ethnicity and insurance status. American Journal of Psychiatry, 159, 1548-1555. Woodwell, D.A., (2000). National Ambulatory Medical Care Survey: 1998 summary. Advance Data From Vital and Health Statistics No. 315. Hyattsville, MD: National Center for Health Statistics. Cassidy, L.J., & Jellinek, M.S. (1998). Approaches to recognition and management of childhood psychiatric disorders in pediatric primary care. Pediatric Clinics of North America, 45, 1037-1052. NAMI. Facts on Children’s Mental Health in America. (2005). www.nimh.nih.gov.