DHYG 311 Principles of Instrumentation Area Specific Curettes
advertisement

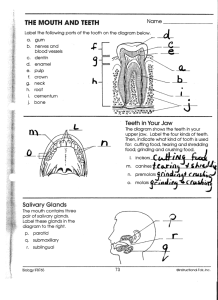
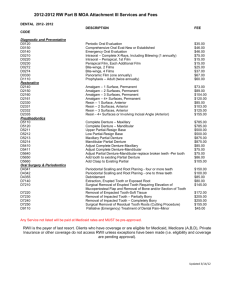
DHYG 311 Principles of Instrumentation Area Specific Curets Deborah L. Cartee, RDH, MS Objectives –Discuss the rationale for removing hard deposits from the teeth –Determine the different methods for removing hard deposits from the teeth –Discuss the procedures that should proceed calculus removal –Determine which hand instruments are used for calculus removal –Determine the parts of area specific curets (Gracey Curets) Objectives –Evaluate the distinct characteristics of area specific curets –Identify which Gracey curets are in the UMSOD scaling cassette –Determine the correct cutting edge of the area specific curet –Understand the proper adaptation, insertion, angulation, and activation of the area specific curets –Evaluate successful instrumentation Why Remove Calculus? Calculus removal is critical to periodontal health because: • The porous surface provides a mechanism for plaque attachment. • It holds inflammatory toxic byproducts of plaque in contact with gingival tissues. How is calculus removed? Scaling - the removal of calculus from all tooth surfaces coronal to the junctional epithelium • supragingival scaling - removal of calculus coronal to the free gingival margin • subgingival scaling - removal of calculus apical to the free gingival margin but coronal to the junctional epithelium Root Planning The removal of remaining specks of calculus, plaque, endotoxins/lipopolysaccharides, etc. The division between scaling and root planning is arbitrary. The ultimate goal is to create a smooth tooth surface. Periodontal Debridement The treatment of gingival and periodontal inflammation through mechanical removal of tooth and root surface irritants to the extent that the adjacent soft tissues maintain or return to a healthy, noninflammed state. –Supragingival debridement –Subgingival debridement –Deplaquing The goal of periodontal debridement is return of tissue health. When can I start Scaling? • After: Medical history/vital signs - to determine contraindications to treatment and identify factors to be considered when developing the treatment plan Extraoral/intraoral exam - to determine contraindications to treatment and identify factors to be considered when developing the treatment plan Periodontal probing - to determine the location, distribution, shape, and depth of pockets Exploring - to determine the location, distribution, and amount of calculus Which hand instruments can be used for calculus REMOVAL? –curets • Area Specific (Gracey) • Universal –Scalers • Sickle • Hoe • Chisel • File Area Specific curets • Cross section The top row of instruments are instruments found in your cassette: Where each instrument is used: Area Specific curets • Parts of the Area Specific curets –Handle –Shank –Working end (blade) • back • lateral surface • face • cutting edge Area Specific curets • Characteristics Set of instruments; each designed for specific areas and surfaces Only one cutting edge is used for each working end Curved in two planes (up and to the side) Offset blade (70 to 80 degrees to the shank) Gracey Instruments: Site Specific: Types: – 1/2 – Regular – 7/8 – Rigids – 11/12 – Minis – 13/14 – After- Fives Types: Regular Rigid Area Specific curets • Determining the correct cutting edge • Lower shank should be parallel to the long axis of the tooth • The face will be close to the tooth and only partially seen if the correct end is selected. The entire shiny face will be seen and a sharp cutting edge will be towards the gingiva if the incorrect end is selected. Area Specific curets –Posterior teeth • Gracey 11/12 for buccal, lingual, and mesial surfaces of molars and premolars - insert at distal line angle and use into mesial col area • Gracey 13/14 for posterior distals - it has a very angulated shank which allows for adaptation to molar and premolar distals. Insert at the distal line angle and use into the distal col area. –Anterior teeth • Gracey 1/2 for anterior teeth - one end is designed for use on the surface toward the operator, the other end is designed for use on the surfaces away from the operator. Area Specific curets: Adaptation – Objective: to keep the cutting edge on the tooth. This will decrease trauma and increase effectiveness of calculus removal. – Keep the lower 1/3 of the cutting edge in contact with varying tooth contours. – Maintain adaptation by rolling the handle. – More than the lower 1/3 of the cutting edge can be adapted on the buccal and lingual surfaces. – Once you reach the line angles only the lower 1/3 should contact the tooth. If the middle 1/3 is contacting the tooth then the lower 1/3 will be into soft tissue. Area Specific curets Do not overcompensate by only using the toe of the instrument. You will not be able to remove calculus with the toe. When working subgingivally you will not be able to see the blade. The handle position will provide a cue to blade position. The handle should be parallel or close to parallel with the long axis of the tooth. If the handle is perpendicular to the long axis, the toe will be directed toward the junctional epithelium. Area Specific curets • Insertion – Face needs to be flat against the tooth (0º) – Insert to the base of the pocket. (0o ) (45o – 90o) Area Specific curets: Angulation Refers to the angle between the face of the blade and the tooth surface Insert at 0º; reach base of sulcus; establish working angulation of 45º -90º To decrease or close angulation - move the lower shank towards the tooth. To increase or open angulation - move the lower shank away from the tooth For heavy deposits the angulation should be close to 90º. For finishing strokes of root planning the angulation should be close to 45º. Area Specific curets • Lateral Pressure –The pressure of the instrument against the tooth surface during activation. –Light, Moderate or Heavy pressure Area Specific curets: Activation Exploratory stroke is used to detect and evaluate. A light grasp is needed for maximum tactile sensitivity with the exploratory stroke. If calculus or roughness is detected then a working stroke should be activated. The working stroke requires a short, powerful pull stroke. Must have a good fulcrum and firm grasp. Engage the apical portion of the deposit with a vertical or oblique stroke. Use wrist (not finger) motion. Working strokes should begin short and powerful. They should become longer and lighter as deposits are removed. Area Specific curets • Evaluation – Use mirror, air, and explorer to evaluate effectiveness. – Tissue response should also be used to determine effectiveness (10-14 days). Sequence: Determine how many teeth you can complete in the time allotted ALWAYS start with the most posterior tooth in the quadrant- Distal surface – Begin with the 13/14 and complete distobuccal area of the molars – Then complete the buccal to mesial surfaces with the 11/12 – NOW: with the same sequence (13/14, 11/12) complete lingual surfaces When you have completed the teeth originally planned, move onto the remaining teeth in that quadrant. Keep in mind that you must keep an eye on the clock so that all the surfaces of a tooth are completed BEFORE you dismiss your patient. Sometimes that means you can only complete one tooth in the given time, or you might be able to complete all the teeth in the quadrant. Consider the following when planning: – Tenacity of the deposit (How difficult to remove?) – Patient management (Are they a talker? Sensitive?)