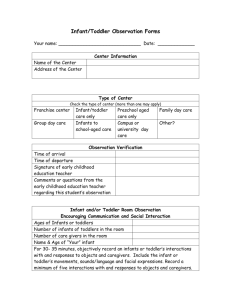
Physical Assessment of the child
advertisement

Physical Assessment of Children Depending of Age Physical Assessment of Infant Assessment is NOT in the head-to-toe manner When quiet, auscultate heart, lungs, abdomen Assess heart & respiratory rates before temperature Palpate and percuss same areas Perform traumatic procedures last Elicit reflexes as body part examined Elicit Moro reflex last Encourage caretaker to hold infant during exam Distract with soft voice, offer pacifier, music or toy Physical Assessment of Toddler Inspect body areas through play – “count fingers and toes” Allow toddler to handle equipment during assessment and distract with toys and bubbles Use minimal physical contact initially Perform traumatic procedures last Introduce equipment slowly Auscultate, percuss, palpate when quiet Give choices whenever possible Photo Source: Del Mar Image Library; Used with permission Physical Assessment of Preschooler If cooperative, proceed with head-to-toe If uncooperative, proceed as with toddler Request self undressing and allow to wear underpants Allow child to handle equipment used in assessment Don’t forget “magical thinking” Make up “story” about steps of the procedure Give choices when possible If proceed as game, will gain cooperation Photo Source: Del Mar Image Library; Used with permission Physical Assessment of School-Age Child Proceed in head-to-toe May examine genitalia last in older children Respect need for privacy – remember modesty! Explain purpose of equipment and significance Teach about body function and care of body Physical Assessment of the Adolescent Ask adolescent if he/she would like parent/caretaker present during interview/assessment Provide privacy Head-to-toe assessment appropriate Incorporate questions/assessment related to genitals/sexuality in middle of exam Answer questions in a straightforward, noncondescending manner Include the adolescent in planning their care Pain Assessment Pain • “Pain is whatever the experiencing person says it is, existing whenever the person says it does.” – McCaffery and Pasero, 1999 • This includes VERBAL and NONVERBAL expressions of pain Pain Facts and Fallacies • FACT: Children are under treated for pain • FACT: Analgesia is withheld for fear of the child becoming addicted • FALLACY: Analgesia should be withheld because it may cause respiratory depression in children • FALLACY: Infants do not feel pain Principles of Pain Assessment in Children: QUESTT • Question the child • Use a pain rating scale • Evaluate behavioral and physiologic changes • Secure parent’s involvement • Take the cause of pain into account • Take action and evaluate results Pain Rating Scales • Not all pain rating scales are reliable or appropriate for children • Should be age appropriate • Consistent use of same scale by all staff • Familiarize child with scale Pain Scales • FACES pain rating scale • Numeric scale • FLACC scale – Facial expression – Legs (normal relaxed, tense, kicking, drawn up) – Activity (quiet, squirming, arched, jerking, etc) – Cry (none, moaning, whimpering, scream, sob) – Consolability (content, easy or difficult to console) Nonpharmacologic Interventions • • • • • Based on age Swaddling, pacifier, holding, rocking Distraction Relaxation, guided imagery Cutaneous stimulation Anesthetics: Topical and Local • Major advancement for atraumatic care • EMLA • NUMBY stuff • Intradermal local anesthetics • Importance of timing Analgesics • • • • Opioids NSAIDs “Potentiators” Lytic cocktail (DPT)—Demerol, Phenergan, and Thorazine • Co-analgesics, amnesics, sedatives, etc. • Role of placebos Dosage of Analgesia • • • • • Based on body weight up to 50 kg Concept of “titration” Ceiling effect of non-opioids First pass effect PCA Fears of Bodily Injury and Pain • Common fears among children • May persist into adulthood and result in avoidance of needed care Pain Assessment: Infants Assessment of pain includes the use of pain scales that usually evaluate indicators of pain such as cry, breathing patterns, facial expressions, position of extremities, and state of alertness Examples: FLACC scale, NIPS scale Young Infant’s Response to Pain • Generalized response of rigidity, thrashing • Loud crying • Facial expressions of pain (grimace) • No understanding of relationship between stimuli and subsequent pain Older Infant’s Response to Pain • • • • Withdrawal from painful stimuli Loud crying Facial grimace Physical resistance Pain Assessment: Toddlers Toddlers may have a word that is used for pain (“owie,” “booboo,” “ouch” or “no”); be sure to use term that toddler is familiar with when assessing. Can also use FLACC scale, or Oucher scale (for older toddlers) Young Child’s Response to Pain • Loud crying, screaming • Verbalizations: “Ow”, “Ouch”, “It hurts” • Thrashing of limbs • Attempts to push away stimulus Pain Assessment: Preschoolers Think pain will magically go away May deny pain to avoid medicine/injections Able to describe location and intensity of pain FACES scale, poker chips and Oucher scale may be used Photo Source: Del Mar Image Library; Used with permission School-Age Child’s Response to Pain • Stalling behavior (“wait a minute”) • Muscle rigidity • May use all behaviors of young child Pain Assessment: Older Children Older children can describe pain with location and intensity Nonverbal cues important, may become quiet or withdrawn Can use scales like Wong’s FACES scale, poker chips, visual analog scales, and numeric rating scales Adolescent • Less vocal protest, less motor activity • Increased muscle tension and body control • More verbalizations (“it hurts”, “you’re hurting me”) Let’s Review The nurse begins a full assessment on a 10 yearold patient. To ensure full cooperation from this patient it is most important for the nurse to: A. Approach the assessment as a game to play. B. Provide privacy for the patient. C. Encourage the friend visiting to stay at the bedside to observe. D. Instruct the child to assist the nurse in the assessment. Let’s Review During a routine health care visit a parent asks the nurse why her 10 month-old infant is not walking as her older child did at the same age. Which response by the nurse best demonstrates an understanding of child development? A. “Babies progress at different rates. Your infant’s development is within normal limits.” B. “If she is pulling up, you can help her by holding her hand.” C. “She’s a little behind in her physical milestones.” D. “You can strengthen her leg muscles with special exercises to make her stronger.” Let’s Review When assessing a toddler identify the order in which you would complete the assessment: 1. 2. 3. 4. Ear exam with otoscope Vital signs Lung assessment Abdominal assessment Let’s Review When assessing pain in an infant it would be inappropriate to assess for: A. B. C. D. Facial expressions Localization of pain Crying Extremity movement