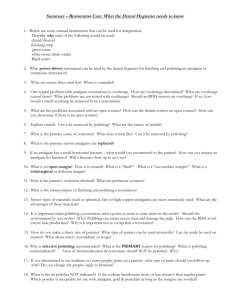
Care of Dental Restorations
advertisement

Care of Dental Restorations Chapter 43 Dental Amalgam Restorations • Margination- Process of removing excess restorative material and applying finishing techniques to re-establish a smooth, welladapted cavosurface margin. The resultant junction should conform in shape and normal anatomic characteristics. • Finishing-process that involves removing marginal irregularities, defining anatomic contours, and smoothing away surface roughness of a restoration. Dental Amalgam Restorations • Polishing- process carried out after placement of a restoration to remove minute scratches from the surface of a restoration and obtain a smooth, shiny luster. Also applied after other refinishing techniques to produce an unscratched homogeneous surface. Uses abrasive agents to remove roughness, eliminate pits or grooves, and make the surface more resistant to bacterial accumulation. Characteristics of an acceptable finished and polished restoration. • • • • • • • • • Smooth anatomic contours Contact areas intact with normal form Embrasures spaced correctly Refined margins Smooth resistant surfaces Functional effectiveness Acceptable appearance No biofilm-retaining irregularities Restored health of the gingival tissues Indications for use of Margination • Excess interproximal material (i.e., overhang, such as a Class II amalgam restoration) which could cause: – Gingival tissues appearing inflamed in the area – Localized vertical bone loss radiographically or when probing – Dental floss often fraying Benefits of Margination • • • • Removes excess amalgam Facilitates plaque control Promotes healthier periodontal tissues Recreates functional anatomy to the restored tooth surface Instruments that could be used for Margination • • • • • • • Finishing knives Files Scalers, curettes, spoon excavators Cleoid-discoid carvers Ultrasonic scaler Finishing discs Finishing polishing strips Finishing strips • Description: thin, flexible strip of metal (lightening strip), linen abrasive strip or plastic impregnated with abrasive particles on one side. • Available in varying grits, – Extra fine to course Technique to remove a large overhang • Assess the overhang – Use an explorer – Assess the condition of the adjacent gingival tissue to determine ease of access to overhang. – Select instruments based on size of overhang and ease of subgingival access. Technique to remove a large overhang • Initial margination – Use a sharp amalgam or appropriate ultrasonic scaler insert – Secure fulcrum – Angulate the blade/insert so only a small portion of the amalgam will be removed – Use short, overlapping, shaving strokes – Avoid removing too much of the overhang – Smooth with a curette – Finish with an abrasive strip Polishing an amalgam restoration • Use wet polishing agents • Use low speed hand-piece with light intermittent strokes • Avoid cementum • Do not over-polish Rubber cups and points • Amalgam polishing kit – Brown and green rubber cups and points have abraisve incorporated in them – Points are used for occlusal – Cups are used for proximal surfaces – Use in this order: • Brown • Green Sterilize after each use Mounted brushes • • • • • • Soften brushes in warm water Use a fine pumice Apply agent over the area Use a slow to moderate speed Use dental tape to apply to proximal surfaces Use course to fine abrasive to acquire finish desired • Rinse well Tin oxide • Use as final polish -apply with light intermittent strokes Rinse and evaluate Esthetic restorations • Composite resins – Class I and II posterior direct restorations – Class III, IV, and V anterior direct restorations – Veneeri for teeth that have been intrinsically stained – Filling of diastemas – Improve size or contour of small or misshaped teeth – Pit and fissure sealants Characteristics of a composite restoration • Softer to an explorer than enamel or porcelain • Esthetic, tooth colored, but may stain • Highly polishable • Must individualize which polishing agent to use. Polishing a composite restoration • Indications for polishing: – Surface roughness – Surface discoloration – Flash or overhang – Over-filled restorations Polishing a composite restoration • Contraindications include: – Open margins – Fractured restorations – Under-contoured proximal contacts – Large overhangs – Recurrent caries ****** • FYI – The use of a plastic matrix strip before polymerization minimizes the amount of finishing required to produce a smooth, regular contoured surface. Contraindications for composite restorations • Use of acidulated phosphate or stannous fluoride • –may cause alteration of the filler particles • -Discoloration of the resin • -avoid mouthrinses containing alcohol – Alcohol may act as a soolvent for the BISGMA resin resulting in softening of the material—making it rougher and stain easier. Polishing a composite restoration • Use rubber points (containing abrasives) on a slow-speed handpiece. • Also, can use with aluminum oxide or diamond pastes that contain particles as small as 1 um in diameter to create smooth, reflective surfaces. Microfilled composite resins • • • • Composed of very fine silica filler Polish very smooth Possess excellent polishing qualities Higher luster than hybrid composite resins Microfilled composite resins • Areas used: – Anterior esthetic restorations – Diastema closures – Hand-sculpted composite veneers – Class III and V restorations Microfilled composite resins • Easy to regain surface luster • High surface shine using rubber polishing cups, wheels, and points • Easy to ditch or scratch upon margination • Chips can be modified and stains can be removed with a sequence of finishing discs and strips. Hybrid Composite resins • A mixture of a mix of glass and silica with large, different-sized filler particles. • They can be used where strength and wear resistance are more important than surface luster. Hybrid Composite resins • Class IV anterior restorations • Incisal edges of anterior teeth • Class I or II posterior restorations where there is a moderate stress chewing load. Hybrid Composite resins • More difficult to achieve and maintain a high luster polish • Best strength of all resin categories • Poishable using a diamond-impregnated polisher • Does not polish as smoothly or with as much shine as the microfill composite resins. Compomer • Is a direct esthetic restorative material that is a combination of glass ionomer and composite. Compomer • Used in Class I, II, III, and V restorations in low stress-bearing areas of patients with moderate risk for dental caries. • Buildups or cores for cast crowns • Esthetic repair for fractured or chipped porcelain restorations. Compomer • Characteristics – Smoother surface than glass ionomer, but not as smooth as composite resin materials – Best translucency an any of the direct esthetic restorative materials – Releases fluoride similar to glass ionomers – Less wear resistant than composites – Good handling characteristics. Glass ionomer resins • Composed of a polyacrlic matrix filled with aluminosilicate particles. • **The benefit of using glass ionomer restorative material is the release of fluoride to reduce dental caries. Glass ionomer resins • Uses: – Cements – Low stress-bearing restorations – Limited use as Class I and II restorations in the primary dentition – Class I, II, and V restorations on a high caries risk patient where esthetics are not critical Glass ionomer resins • Characteristics – Cannot be polishned to the same smoothness as composite resin – Minimal shine – Brittle – Higher incidence of fracture and wear – More opaque—less desirable than other composite resin materials Porcelain • Mostly are completed in the laboratory prior to cementation. • Cerec • Longest lasting cosmetic restoration material • When maintained the porcelain restoration can last for many years---if it is not—the restoration can become rough. Porcelain • If the porcelain restorative material becomes rough: – Can increase wear of the opposing dentition – Increase the susceptibility to stain and dental caries. – Periodontal inflammation can occur is the gingival margins are not adequately polished. Porcelain • High fusing material is used for detnure teeth • Medium fusing material is used for anterior porcelain jacket crowns, ceramic restorations, inlays, onlays and crowns. • Low fusing material is used in porcelainfused- to- metal crowns. Porcelain • Characteristics – Mimics tooth color – More esthetic appearance than composite resins – Retains luster – Subject to fracture – Staining Dental hygiene care for porcelain • Gently debride deposits with curets • Avoid the use of a sickle, ultrasonic, or sonic scaler, air polisher, or air abrasive unit. • Consider the use of a plastic instrument instead. Dental hygiene care for porcelain • Use a low-speed handpiece • Special paste for porcelain use • Moisten a soft, flexible rubber cup or felt disc or wheel • Polish for 15-30 seconds • Dilute the paste with water as the polishing progresses How can the DH identify the restorative material? • • • • Review patient record Gather patient information Use tactile detection with a dental explorer Use air—esthetic restorations may reveal a dry, chalky appearance. Finishing and Polishing Materials • The intent of polishing is to: – create a restorations that fit and maintain occlusal harmony – to produce a smooth surface – Less plaque and calculus adherence – Decrease the potential for the corrosion of metal restoration material. Abrasive procedure • Abrasion is the wearing away or removal of material by rubbing, cutting, or scraping. Finishing • process that involves removing marginal irregularities, defining anatomic contours, and smoothing away surface roughness of a restoration. Factors that affect finishing a. Hardness refers to the abrasive’s ability to cut b. Size influences the speed of the cut a. Larger particles abrade a surface more rapidly. b. Particles are classified by size in micrometers(um) a. Course = 100 um b. Medium = 10 to 100 um c. Fine = 0 to 10 um Pressure applied during finishing and polishing 1. Of the force, when greater, results in more rapid removal of the material. 2. When greater, creates increased temperature and heat. 3. Under higher temperatures can lead to distortion or physical changes within the appliance/restoration. 4. With high temperatures may cause discomfort for the patient because of the transmission of heat to the pulpal tissues. Speed of cup/point/brush during finishing and polishing procedure. • 1. When faster, results in faster cutting rates. • When faster, creates greater temperatures. • When faster, creates greater danger of over-cutting the appliance/restoration. Types and composition of abrasives • Diamond – Composed of carbon – Is the hardest substance; is an efficient abrasive because it does not wear down or lose sharpness easily Types and composition of abrasives • Carbides – Include silicon carbide, boron carbide and tungsten carbide – Silicon and boron for finishing instruments typically are supplied as particles pressed with a binder into disks or wheels for use on a hand-piece. Aluminum oxide • Typically is produced as particles bonded to paper disks and strips or impregnated into rubber wheels and points. • Is the abrasive used for white stones—used for polishing of porcelain. • Has fine particles of aluminum oxide and diamond that can be mixed into a paste to produce smooth, polished surfaces on many types of restorations, including acrylics and composites. Zirconium silicate • Is a natural mineral • Is used as a polishing agent in strips and disks. • Often is used in prophylactic pastes. Tin oxide • Is used as a polishing agent for metallic restorations, especially amalgams • Produces excellent polish of enamel. Pumice • Is a natural glass that is rich in silica • Polishes acrylics and enamel. Rouge • Is iron oxide • Is a powder that can be formed into a block or cake and used on a rag wheel in a dental lathe/handpiece to polish gold alloys.