Case Management: Thyroid
advertisement

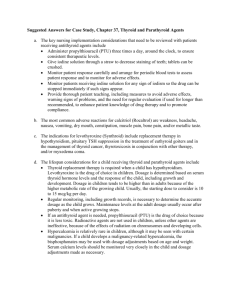
Case Management: Thyroid Joey Tabula Mayou Martin Tampo Korina Ada Tanyu General Information MJA, 35/F, married, right-handed, Roman Catholic, housewife from Infanta, Quezon Chief complaint: ABDOMINAL ENLARGEMENT Patient Profile • No DM, HPN, BA • No vices DIFFUSE TOXIC GOITER (2007) anterior neck mass with associated palpitations, dysphagia, dyspnea, tremors and heat intolerance PTU and Propanolol taken for ~ 6 months with resolution of symptoms. Discontinued. Lost to follow-up. 6 mo PTC 3 mo PTC 2 wk PTC RECURRENCE palpitations tremors heat intolerance Now with... Exertional dyspnea Gradual abdominal enlargement Progressive bipedal edema. 1 wk PTC 1 day PTC Consulted Admitted in Lucena and allegedly given IV antibiotics. Discharged improved after 10 days PTU and propanolol on fair compliance 6 mo PTC 3 mo PTC 4 wk PTC 1 wk PTC 1 day PTC Readmitted for dyspnea and abdominal enlargement. Given unrecalled meds probably diuretics which decreased the edema Discharged after 2 days with relief of symptoms. 6 mo PTC 3 mo PTC 4 wk PTC 1 wk PTC 1 day PTC Persistence of exertional dyspnea, abdominal enlargement, and bipedal edema. Now with 2-pillow orthopnea and jaundice. No consult 6 mo PTC 2 mo PTC 2 wk PTC 1 wk PTC 1 day PTC • 1 week prior to consult ▫ Increase in the severity of the exertional dyspnea on mild activity, abdominal enlargement, and bipedal edema ▫ Now with paroxysmal nocturnal dyspnea ▫ Consulted at a local hospital in Quezon ▫ “may tubig sa tiyan” ▫ Advised transfer to PGH for evaluation and management 6 mo PTC 2 mo PTC 2 wk PTC Persistence of symptoms 2 episodes of vomiting Consult at PGH 1 wk PTC 1 day PTC Review of systems • • • • • • • (+) weight loss ~50% (-) loss of consciousness (-) blurring of vision (-) dizziness (-) headache (-) chest pain (-) melena/hematochezia Past and Family History • Past Medical History ▫ As above ▫ (-) PTB ▫ No known allergies • Family Medical History ▫ (+) hypertension – mother ▫ (+) goiter – sister and brother ▫ (-) DM, PTB, asthma, heart disease Personal Social History • Housewife • With 4 children • No vices OB-Gyne History • • • • G5P5 (5005) LMP: December 15, 2009 PMP: November 2009 Irregular, lasting for ½ month sometimes, consumes 6 cloths per day • IUD since 2000 Physical Examination at the ER • BP = 140/90, HR = 160s, RR = 24, T = 37.2 • Awake, coherent, oriented • Icteric sclerae, pink conjunctivae, (+) exophthalmos, neck vein engorgement, ANM 10 x 10 cm, nontender, moves with deglutition • Equal chest expansion, subcostal and intercostal retractions, bibasal crackles, and rhonchi • Adynamic precordium, DHS, tachycardic, irregularly irregular rate • Globular, NABS, soft, nontender, (+) fluid wave • bipedal pitting edema, anasarca, DTR ++ Differentials for Hyperthyroidism Differentials Points for Points against Graves’ Disease With the above mentioned SSx, especially the ophthalmopathy Cannot be ruled out Thyroiditis With the above mentioned SSx Nontender goiter Struma ovarii With the abovementioned SSx, abdominal enlargement No masses palpable on PE Drug induced hyperthyroidism With the abovementioned SSx No history of intake Other Problems Differential Points for Points against Congestive Heart Failure NVE, ascites, crackles prob sec to TTHD Cannot be ruled out Community-acquired pneumonia Cannot be ruled out Crackles, cough, fever, tachypnea Working Impression Diffuse Toxic Goiter probabaly Graves’ Disease, in storm Thyrotoxic Heart Disease in CHF FC III r/o CAP-MR s/p IUD insertion (2000) AF in Course at the ER Diffuse nodular toxic goiter, in storm CHF FC II-III with AF in RVR, t/c CAP-MR Course at the ER • Burch and Wartofsky Score (85) ▫ ▫ ▫ ▫ ▫ ▫ Temperature – 5 CNS – 0 GI – 20 Precipitant history - 10 Cardiac (> 140) – 25 CHF Edema 5 Bibasal rales 10 AF 10 • Labs done: CBC, RBS, Crea, Na, K, Ca, Mg, Albumin, ALT/AST, PT/PTT, urinalysis, 12 L ECG, xray (chest and abdomen) • Medications given ▫ ▫ ▫ ▫ ▫ ▫ PTU 50 mg tab 12 tabs now then 1 tab TID Propanolol 40 mg 1 tab now, then 40 mg tab Digoxin 0.25 mg IV now Furosemide 40 mg IV SSKI 5 drops q6 h, 1 hour post PTU Dexamethasone 2 mg IV q6 h • Referred to POD Physical Exam at Med-ER • Awake, conscious, coherent • BP = 90/60, HR = 115, RR = 22, T = 37.2 • Icteric sclerae, pink palpebral conjuctivae, (+) anterior neck mass 10 x 10 cm • Equal chest expansion, no retractions, (+) bibasal crackles • Adynamic precordium, distict heart sound, tachycardia, irregular rhythm, no murmur • Globular, normoactive bowel sounds, soft, (+) ascites, no tenderness • Full and equal pulses, pink nailbeds, (+) grade 2 bipedal edema Course at the Med-ER • Assessment: DTG in storm, thyrotoxic heart disease, in CHF FC III, AF in VR, t/c CPC of the liver, s/p IUD insertion • Plan ▫ ▫ ▫ ▫ NPO except medications Keep on moderate high back rest IVF: 1 liter D5NSS x 16 hours Side drip: furosemide 100 mg in 100 cc PNSS in soluset at 4 cc/hr ▫ Diagnostics: FT4, TSH, add FBS, lipid profile, holoabdominal UTZ, fecalysis ▫ Tx: add paracetamol 500 mg tab 1 tab OD q4 prn for T ≥ 38.5 Albumin 22 low Alkaline phosphatase 94 AST 61 high ALT 42 Ca 1.86 low Mg 0.82 Glucose 5.6 Crea 131 high Na 133 low K 3.2 low Cl 104 PT 11.3/22.4/0.35/2.15 APTT 35.8/52.8 U/A dark yellow hazy 1.015 pH 6 trace sug neg prot 0-1 RBC 1-3 WBC 0-1 hyaline casts 0-1 waxy cast occ epith cells neg crystals 1+ bact occ mt Bilirubin 3+ trace ketone CBC WBC 10.1 3, RBC 6 , Hgb 101, Hct 0.302, MCV 83.7, MCH 28.1, MCHC336, RDW 15.9, PC 201, N 0.7, L 0.15, M 0.14, E 0.01, B 0 CXR: Cardiomegaly LV form 7AM MICU DTG, instorm With TTHD in CHF FC III with AF in RVR With TTLD 10 AM Day MHAPOD DTG Grave’s Disease in thyroid storm With TTHD in CHF FC III with AF in RVR With TTLD 10:45AM Endo Maintained r/o CAP 11 AM Day MHAPOD 8:30 PM RIC Maintained Decreased PTU 2 tabs q6 Decreased Propanolol 1 tab TID defer if BP <90/60 O2 prn Same Increased PTU 4 tabs q4 Increased SSKI 5 drops q4 Increased Propanolol 40 mg q8 Started oral KCl 15 cc TID x 2 cycles Started NaCl tab 1 tab BID x 2 days Same 3/12/10 Endo 3/13/10 RIC 5 PM Grave’s disease, storm resolving With TTHD in CHF FC III with AF in RVR With TTLD Azotemia probably prerenal from poor intake and 3rd spacing loses Anemia multifactorial, IDA Grave’s disease not in storm With TTHD in CHF FC III with AF in RVR With TTLD d/c dexa and SSKI Shifted PTU to Methimazole 20 mg q8 Continued Propanolol Started Furosemide 40 mg IV q12 or tab Defer for BP <90/60 ideally bumetanide Started oral KCl 10% 30 cc q8 Resume digoxin once electrolyte corrected Home meds: Furo 20 mg bid Spiro 25 mg po Propanolol 10 mg tid PTU 50 mg 2 tabs tid Vit D +CaCO3 1 tab bid Kalium durule 1 tab tid x 3 days Laboratories Prior to Discharge • BUN 21.69, Crea 138, TB 560.56, DB 401.83, IB 158.73, Mg 0.70, Na 137, K 2.7 Discharge Diagnosis • Graves’ Disease, not in storm • Thyrotoxic Heart Disease in CHF FC III with Atrial Fibrillation in RVR • t/c Chronic-Passive Congestion of the Liver • s/p IUD insertion (2000) Course in the Wards • Home medications • Furosemide 20 mg 1 tab bid • Spironolactone 25mg 1 tab od • Propanolol 10 mg tid • PTU 50 mg 2 tabs tid • Vitamin D + CaCO3 1 tab bid • Kalium durule TID x 3 d Management of Thyroid Storm Introduction • Thyrotoxicosis ▫ Elevated thyroid hormone ▫ Most common causes: Graves’ Disease (60-80%) Hyperthyroidism Thyroid storm (thyroid crisis) Introduction • Hyperthyroidism ≠ Thyrotoxicosis ▫ Conditions with increased thyroid hormone but normal thyroid function: Thyroiditis Thyrotoxicosis factitia Signs and Symptoms • Represent a hypermetabolic state with increased adrenergic activity • • • Tachycardia, atrial fibrillation in the elderly Hyperactivity, irritability, dysphoria • Tremor Heat intolerance and sweating • Goiter Palpitations • Warm, moist skin Fatigue and weakness • Muscle weakness, proximal Weight loss with increased myopathy appetite • Lid retraction or lag Diarrhea Polyuria • Gynecomastia • Oligomenorrhea, loss of libido • • • • • * in descending order of frequency Signs and Symptoms • Other Signs: ▫ ▫ ▫ ▫ ▫ Chest pain – often w/o cardiovascular disease Psychosis Disorientation Hyperdefacation Edema Signs and Symptoms • Other Symptoms ▫ ▫ ▫ ▫ ▫ Diaphoresis Dehydration Fever Widened Pulse Pressure Thyromegaly Graves = nontender, diffuse Thyroiditis = tender, diffuse Single nodule or MNG ▫ Thyroid bruit (Brief) Pathophysiology Etiologies • • • • • • Autoimmune Drug-Induced Infectious Idiopathic Iatrogenic Malignant Etiologies • Autoimmune ▫ ▫ ▫ ▫ Graves Chronic thyroiditis (Hashimoto) Subacute thyroiditis (de Quervain) Postpartum thyroiditis Etiologies • Infectious ▫ Suppurative thyroiditis ▫ Postviral thyroiditis • Idiopathic ▫ Toxic MNG 2nd most common cause of hyperthyroidism Etiologies • Iatrogenic ▫ Thyrotoxicosis factitia ▫ Surgery • Malignant ▫ Toxic adenoma ▫ TSH – secreting pituitary tumor ▫ Struma ovarii Etiologies • Thyroid storm (classically w/ underlying Graves or toxic MNG) can be triggered by: ▫ ▫ ▫ ▫ ▫ ▫ ▫ ▫ ▫ Infection General surgery Cardiovascular events Toxemia of pregnancy DKA, HHS, insulin-induced hypoglycemia Thyroidectomy Non-adherence to antithyroid medication RAI Vigorous palpation of the thyroid gland Differential Diagnosis • • • • • • Anxiety Panic Disorders Delirium Tremens Neuroleptic Malignant Syndrome CHF DM Differential Diagnosis • • • • • Septic Shock Heat Exhaustion/ Heat Stroke Munchausen Syndrome Withdrawal Syndromes Toxicity ▫ Anticholinergics (atropine) ▫ Selective Serotonin Reuptake Inhibitors (fluoxetine) ▫ Sympathomimetics (dopamine) The Burch-Wartofsky Score • assess of the probability of thyrotoxicosis independently from the level of thyroid hormones • temperature, central nervous effect, hepatogastrointestinal, cardiovascular dysfunctin, and history • > 25 points thyrotoxicosis is possible • > 45 points, probable Thermoregulatory Dysfunction Score Cardiovascular Dysfunction 99-99.9 F (37.2-37.7 C) 5 Tachycardia 100-100.9 F (37.8-38.2 C) 10 99-109 BPM 5 101-101.9 F (38.3-38.8 C) 15 110-119 BPM 10 102-102.9 F (38.9-39.3 C) 20 120-129 BPM 15 103-103.9 F (39.4-39.9 C) 25 130-139 BPM 20 ≥ 104 F (>40.0 C) 30 ≥ 140 BPM 25 Central Nervous System Score Congestive Heart Failure Score Agitation 10 Pedal Edema 5 Delirium/Psychosis/ Lethargy 20 Bibasal Rales 10 Seizure/Coma 30 Pulmonary Edema 15 GI – Hepatic Dysfunction Score Atrial fibrillation Present 10 Diarrhea, Nausea/Vomiting, Abdominal Pain 10 Precipitant History Present 10 Severe jaundice 20 Burch – Wartofsky Criteria Score Workup • In thyroid storm, the diagnosis must be made on the basis of the clinical examination. • Total T4 not measured ▫ variations in serum thyroid-binding proteins alter the ability to interpret results • TFT’s do not distinguish thyrotoxicosis from thyroid storm Workup • Some lab abnormalities in thyroid storm ▫ ▫ ▫ ▫ ▫ ▫ Hyperglycemia Hypercalcemia Hepatic function abnormalities Low serum cortisol Leukocytosis Hypokalemia (in HPP) Imaging • CXR ▫ May identify trigger for thyroid storm, ex. CHF or pneumonia ▫ Thyroid scan Diffuse uptake = Graves Focal uptake = toxic adenoma Other Diagnostics • 12-L ECG ▫ Sinus tachycardia (most common) ▫ AF (often in elderly) ▫ Complete heart block (rare) Critical Care • Prompt institution of treatment ▫ Hook to cardiac monitor Arrhythmia may convert to sinus only after antithyroid tx ▫ Intubate if profoundly altered sensorium ▫ Aggressive fluid resuscitation (3-5L/d) Profound GI and insensible losses ▫ Thermoregulation with aggressive TSB and antipyretics Avoid ASA decreased protein binding increased fT3, fT4 Critical Care • Antithyroid Treatment ▫ To prevent synthesis of new thyroid hormone: ▫ Load 600 mg PTU then 200-300 mg q6 (PO, per NGT, per rectum) PTU prevents peripheral conversion of T4T3 Clinical effects may be seen after 1 hour Critical Care • Antithyroid Treatment ▫ To prevent release of preformed hormone: ▫ 1 hour after loading PTU, give stable iodide Wolff-Chaikoff vs. Jod-Basedow 5 drops SSKI q6 0.5 mg iopodate or iopanoic acid q12 Iodine allergy? Use lithium Critical Care • Anti-adrenergic Treatment ▫ Anti-adrenergic activity to control symptoms and heart rate High output heart failure ▫ Propranolol 40-60 mg PO/NGT or 2 mg IV q4 High dose propranolol inhibits peripheral conversion of T4T3 Critical Care • Corticosteroids ▫ Dexamethasone 2 mg 6h Inhibits thyroid hormone synthesis Inhibits peripheral conversion of T4T3 ▫ Suspicion of Adrenal Insufficiency Inpatient Care • • • • Admit to ICU Confirm diagnosis with labs Clinical improvement a few hours after therapy Titrate medications to optimimize antithyroid and antiadrenergic effects • Aggressively treat infection, underlying precipitants Inpatient Care • • • • Admit to ICU Confirm diagnosis with labs Clinical improvement a few hours after therapy Titrate medications to optimimize antithyroid and antiadrenergic effects ▫ May take 4-8 weeks after discharge • Aggressively treat infection, underlying precipitants Prognosis • Thyroid storm is usually fatal unless treated ▫ Overall mortality 10-20%, some report 75% ▫ The precipitating factor is usually the underlying COD • With early diagnosis and prompt treatment, prognosis is good. Patient Education • Stress the importance of medication adherence. • Stress the importance of medication adherence. • Explain the possible side effects of treatment. ▫ Antithyroid – liver failure, agranulocytosis ▫ Anti-adrenergic – hypotension, dermatologic ▫ Corticosteroids – cushingoid disease, DM Medicolegalities • Because of variable presentation, thyroid storm may be missed in patients who present obtunded or comatose. • Apathetic thyrotoxicosis in the elderly ▫ ▫ ▫ ▫ Protracted duration of symptoms Weight loss Cardiovascular abnormalities (common) Ocular findings (less common) • Consider thyrotoxicosis in patients with acute behavioural changes referred for psych evaluation. Grave’s Disease •60–80% of thyrotoxicosis. •~2% of women but is 1/10 as frequent in men. • rarely begins before adolescence and typically occurs between 20 and 50 years of age, but it also occurs in the elderly. Pathogenesis • ENVIRONMENTAL and GENETIC ▫ polymorphisms in HLA-DR, CTLA-4, and PTPN22 (a T cell regulatory gene. • SMOKING is a minor risk factor for Graves' disease and a major risk factor for the development of ophthalmopathy. • Sudden increases in iodine disease, and there is a intake may precipitate Graves' 3x increase of Graves' disease in the postpartum in the occurrence period. • The hyperthyroidism of Graves' disease is caused by TSI that are synthesized in the thyroid gland as well as in bone marrow and lymph nodes. • Other thyroid autoimmune responses, similar to those in autoimmune hypothyroidism occur concurrently in patients with Graves' disease. TPO antibodies occur in up to 80% of cases and serve as a readily • In particular, measurable marker of autoimmunity. In the long term, spontaneous autoimmune hypothyroidism may develop in up to 15% of Graves' patients. • Cytokines appear to play a major role in thyroid-associated ophthalmopathy. • Infiltration of the extraocular muscles by activated T cells; the release of cytokines such as IFN-, TNF, and IL-1 results in fibroblast activation and increased synthesis of glycosaminoglycans that trap water, thereby leading to characteristic muscle swelling. • Late in the disease, there is IRREVERSIBLE FIBROSIS. • TSH-R MAY BE A SHARED AUTOANTIGEN that is expressed in the orbit. • INCREASED FAT is an additional cause of retrobulbar tissue expansion. The INCREASE IN INTRAORBITAL PRESSURE can lead to proptosis, diplopia, and optic neuropathy Clinical Manifestations • ophthalmopathy and dermopathy specific for Graves' disease Opthalmopathy Grading 0 = No signs or symptoms 1 = Only signs (lid retraction or lag), no symptoms 2 = Soft tissue involvement (periorbital edema) 3 = Proptosis (>22 mm) 4 = Extraocular muscle involvement (diplopia) 5 = Corneal involvement 6 = Sight loss In the elderly, features of thyrotoxicosis may be subtle or masked, and patients may present mainly with fatigue and weight loss, a condition known as APATHETIC THYROTOXICOSIS. • UNEXPLAINED WEIGHT LOSS • WEIGHT GAIN OCCURS IN 5% • HYPERACTIVITY, NERVOUSNESS, AND IRRITABILITY • SENSE OF EASY FATIGABILITY • INSOMNIA AND IMPAIRED CONCENTRATION • FINE TREMOR • HYPERREFLEXIA, MUSCLE WASTING, PROXIMAL MYOPATHY WITHOUT FASCICULATION • HYPOKALEMIC PERIODIC PARALYSIS (ASIAN MALES WITH THYROTOXICOSIS) • SINUS TACHYCARDIA, OFTEN ASSOCIATED WITH PALPITATIONS, OCCASIONALLY CAUSED BY SUPRAVENTRICULAR TACHYCARDIA • HIGH CARDIAC OUTPUT PRODUCES A BOUNDING PULSE, WIDENED PULSE PRESSURE, AND AN AORTIC SYSTOLIC MURMUR • ATRIAL FIBRILLATION IS MORE COMMON IN PATIENTS >50 YEARS • WARM AND MOIST SKIN • SWEATING AND HEAT INTOLERANCE, • PALMAR ERYTHEMA, ONYCHOLYSIS • PRURITUS, URTICARIA, AND DIFFUSE ALOPECIA IN 40% • HAIR TEXTURE MAY BECOME FINE, AND A DIFFUSE ALOPECIA OCCURS IN UP TO 40% • GI TRANSIT TIME IS DECREASEDINCREASED STOOL FREQUENCY, OFTEN WITH DIARRHEA AND OCCASIONALLY MILD STEATORRHEA • OLIGOMENORRHEA OR AMENORRHEA • IMPAIRED SEXUAL FUNCTION, RARELY, GYNECOMASTIA. • OSTEOPENIA IN LONG-STANDING THYROTOXICOSIS • MILD HYPERCALCEMIA OCCURS IN UP TO 20% OF PATIENTS, BUT HYPERCALCIURIA IS MORE COMMON SMALL INCREASE IN FRACTURE RATE IN PATIENTS WITH A PREVIOUS HISTORY OF THYROTOXICOSIS. • GOITER 2X ITS NORMAL SIZE, FIRM, THRILL OR BRUIT • LID RETRACTION • GRAVES' OPHTHALMOPATHY OR THYROID-ASSOCIATED OPHTHALMOPATHY ▫ occurs in the absence of Graves' disease in 10% of patients. • Onset occurs within THE YEAR BEFORE OR AFTER the diagnosis of thyrotoxicosis in 75% of patients. THYROID DERMOPATHY occurs in <5% of patients with Graves' disease most frequent over the anterior and lateral aspects of the lower leg (pretibial myxedema) THYROID ACROPACHY in <1% of patients with Graves' disease MANAGEMENT Treatment of Graves’ Disease Hegedus, L. 2009. Treatment of Graves’ Hyperthyroidism: Evidence-Based and Emerging Modalities. Endocrinol Metab Clin N Am 38: 355-371. Treatment Choices • Antithyroid Drugs • Radioactive Iodine • Surgery Antithyroid Drugs PTU Methimazole Carbimazole Antithyroid Drug Regimens The starting dose of antithyroid drugs can be gradually reduced (TITRATION REGIMEN) as thyrotoxicosis improves. High doses may be given combined with levothyroxine supplementation (BLOCK-REPLACE REGIMEN) to avoid drug-induced hypothyroidism. Other Drugs • • • • • • • Beta-adrenergic Antagonist Drugs Glucocorticoids Inorganic iodide Iodine-containing compounds Potassium perchlorate Lithium carbonate Novel Immunomodulatory agents (rituximab) Radioiodine Treatment • causes progressive destruction of thyroid cells • can be used as initial treatment or for relapses after a trial of antithyroid drugs • Small risk of thyrotoxic crisis, hence the need for antithyroid drugs prior to radioiodine treatment ▫ Carbimazole or methimazole - stopped at least 3 days before radioiodine administration ▫ Propylthiouracil - has a prolonged radioprotective effect Radioiodine Treatment • 131I dosage range between 185 MBq (5 mCi) to 555 MBq (15 mCi) • Tendency to relapse ▫ thyroid ablation vs. euthyroidism • Safety precautions ▫ Avoid contact with children and pregnant women • Risk of hypothyroidism • Contraindicated in pregnancy and breastfeeding mothers Radioiodine Treatment • Severe ophthalmopathy requires caution ▫ prednisone, 40 mg/d, at the time of radioiodine treatment, tapered over 2–3 months to prevent exacerbation of ophthalmopathy Surgical • option for patients who relapse after antithyroid drugs and prefer this treatment to radioiodine • careful control of thyrotoxicosis with antithyroid drugs, followed by potassium iodide (3 drops SSKI orally TID needed prior to surgery • complications ▫ bleeding, laryngeal edema, hypoparathyroidism, and damage to the recurrent laryngeal nerves • Thank you 3/11/10 DEMS 2AM DNTG in storm with CHF FC II-IIII with AF in RVR t/c CAP-MR 4:50 AM POD DTG in storm Thyrotoxic Heart Disease in CHF FC III with AF in RVR t/c CPC of the liver s/p IUD insertion (2000) 6 AM Gen Med DTG in storm Thyrotoxic Heart Disease in CHF FC III with AF in RVR t/c CPC of the liver s/p IUD insertion (2000) PTU 50 mg/tab 12 tabs now then 1 tab TID (2AM) Propanolol 40mg/tab now then40 mg tab OD Digoxin 0.25 mg IV now Furosemide 40 mg IV (2:30AM) SSKI 5 drops q6, 1 hr post PTU (3:30AM) Dexamethasone 2 mg IV q6 (4:30AM) Hooked 4 lpm PTU 50 mg/tab 2 tab q6 Propanolol 10mg/tab TID Digoxin 0.25 mg/tab OD SSKI 5 drops q6, 1 hr post PTU Dexamethasone 2 mg IV q6 Paracetamol 500mg/tab for T 38.5 O2 via NC at 2-4lpm, hook to CM Increased PTU to 4 tabs q6 Increased propanolol to 2 tabs TID • 3/11/10 Alb 22 low alk phos 94 AST 61 high ALT 42 Ca 1.86 low Mg 0.82 • Gluc 5.6 Crea 131 high Na 133 low K 3.2 low Cl 104 • PT 11.3/22.4/0.35/2.15 • APTT 35.8/52.8 • U/A dy h 1.015 6 trace sug neg prot 0-1 RBC 1-3 WBC 0-1 hyaline casts 0-1 waxy c occ epith cells neg crystals 1+ bact occ mt Bilirubin 3+ trace ketone CBC 10.1 3.6 101 0.302 83.7 28.1 336 15.9 201 0.7 0.15 0.14 0.01 0 3/13 BUN 21.69 Crea 138 BCR 38.82 (prerenal azotemia) Mg 0.70 Na 137 K 2.7 • • • • • • • Decrease in edema Decrease in resting dyspnea Decrease in abdominal distension No hyperdefecation No agitation No palpitations With easy fatigability • • • Awake afebrile not in distress Stable VS no pallor AP, irreg irreg no murmur Intact traubes (+) fluid wave, succusion splash, shifting dullness, bipedal edema • • • • A> Grave’s disease not in storm t/c TTHD with CHF FC II in AF in CVR t/c TTLD Home meds Furo 20 mg 1 tab bid Spiro 25mg 1 tab od Propanolol 10 mg tid PTU 50 mg 2 tabs tid Vit d + CaCO3 1 tab bid Kalium durule tid x 3 d 1. 2. 3. 4. 5. 6. Medication • • • • PTU 600 mg loading dose then 200-300 mg q6h SSKI 5 drops q6h 1hr after PTU Propanolol 40-60 mg PO q4h or 2 mg IV q4h Dexamethasone 2 mg q6h