chemistry - Austin Community College
advertisement

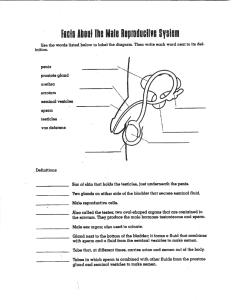
Urinalysis and Body Fluids Unit 5 Seminal Fluid CRg Seminal Fluids - objectives 1. 2. 3. 4. 5. 6. 7. Discuss the major components of seminal fluid with regard to source, function, normal and abnormal appearance. List three (3) reasons for semen analysis. Outline instructions to give to a patient for the correct method for collecting a semen specimen for laboratory analysis. List two (2) methods for identifying a questionable fluid as semen. State the significance of finding increased acid phosphatase in a suspicious fluid. Calculate a sperm count when provided with the number of sperm counted, the dilution factor and the area of the counting chamber used. List the normal values for: semen volume, viscosity, pH, sperm count, motility and morphology. Seminal Fluids • Composition of Semen • Spermatozoa • Fluids to provide nutritional support and media % of total forDescription or mechanism delivery / Purpose Spermatozoa 2-5% Formed in testes, stored in epididymis and vasa differentia Seminal Fluid 60-75% Alkaline fluid,; primarily responsible for nutritional support through: amino acids, enzymes, fructose. Also to suppress possible immune response by female Prostate Fluid 25-30% Acid phosphatase, citric acid, proteolytic enzymes and zinc Bulbourethral glands 1 – 5% Galactose, mucous Seminal Fluids • Anatomy, composition and formation. • Testes – source of sperm (2-5%) • Seminal vesicles – provides fructose & nutrients and is primary provider of fluid (@ 60-75%) • Prostate gland – Provides enzyme, acid phosphatase, citric acid, zinc, and proteolytic enzymes (for coagulation and liquification). 2nd source of fluid(25-30%) • Bulbourethral glands - @ 5%. Thick alkaline mucous-like fluid that neutralizes acids. Seminal Fluids • Spermatozoa - produced in the testes, mature in the epididymis. Seminal Fluids • Reasons for Testing • Infertility issues – more often a problem with the woman, but easy to rule-out the male. • With assisted reproductive technology, greater emphasis placed on sperm quality and quantity. • Post- vasectomy – frequent reason for testing • Test at one month intervals until 2 consecutive months are negative for sperm. Seminal Fluids • Reasons for Testing • Forensic analysis of fluid as being semen • as in alleged rape. • Vaginal swab, washings, or scrapings microscopically evaluated for sperm • chemical test for enzyme: acid phosphatase o Contributed by prostate gland o Present even in the absence of sperm cells • Sperm donors - artificial insemination programs Seminal Fluids • Specimen Collection • Sterile container • Direct deposit preferred • no lubricants, spermacides, condoms, etc. • Complete specimen • Majority of sperm are in first part of ejaculate • 3 day sexual abstinence required • But not more than 5 days. • Best if collected at laboratory site. • If other, specimen must be kept warm and delivered to lab within 1 hour • Time of collection important. • Must be recorded! Seminal Fluids • Physical characteristics • Liquefaction – fresh specimen will clot, then liquefy within 30 – 60 minutes • Persistence of clot is abnormal • All further evaluation must wait until liquefaction is complete. Seminal Fluids Semen: Appearance Opaque Normal Gray, white, light yellow Shades of yellow Correlate with flavin concentration Deep yellow Could also indicate contamination with urine. Associated with certain drugs Brown or red May contain blood Highly turbid Usually contains leukocytes indicating infection or inflammation Seminal Fluids Semen: Appearance, cont. Volume 2.0 – 5.0 mL Measured in serological pipet pH Recorded to 1 decimal place 7.2 – 8.0 Measured with pH paper Alkaline to off-set acid vaginal environment Acid may indicate increased prostatic fluids pH > 8 may indicate infection Seminal Fluids Semen: Appearance, cont. Viscosity Pours in droplets (as shown in picture) Rating: 0 = water-like 4 = gel-like Semen: Microscopic Analysis • • • • • • Motility Concentration / cell count Morphology Agglutination Viability Penetration of cervical mucous Semen: Microscopic Analysis • Microscopic examination • Generally performed 30 - 60 min after collection • Must be after liquidification has occurred • Motility • Motility is a very necessary quality of sperm. Must propel through uterus & fallopian tubes which is quite a long distance. • Must be evaluated within the 1st hour following collection • Will decrease over time Semen: Sperm Motility • • • • • • • Analysis to begin within 1 hour of specimen collection Evaluation times may vary between labs, but usually at set intervals Consistency in technique and procedure important Using hemocytometer & coverslip, examine a drop of undiluted specimen using high dry objective. Brightfield microscopy with light level reduced Some labs use phase microscopy Alternate method: High-resolution video photography / CASA (computer assisted semen analysis) Semen: Sperm Motility • Manual Subjective evaluation • Observe immediately following liquidfication; and within 1st hour. • Place well mixed undiluted drop on pre-warmed hemacytometer slide • Observe under high-dry objective; with reduced light. • Rated from “0” to 4.0” • • • • • 4.0 – rapid and straight line movement 3.0 – slower, and some lateral movement 2.0 – slow forward progression, noticeable lateral movement 1.0 – no forward progression 0 – no movement • Other types of rating scales may be used • Normal (authors vary greatly) but > 50-60% show 2.0 or greater at 1 hour. Semen: Microscopic Analysis • Morphology • May be performed in cytology, pathology, or hematology • Oval/egg shaped head (3x5um) • While oval from the front, appears flattened when viewed from the side appears flattened • @ ½ covered with an enzyme laden acrosomal cap, which contains • Middle piece • provides energy • Tail piece of @ 45 – 55 um long Semen: Microscopic Analysis • Morphology • At least 200 cells evaluated on smear (Wright’s, Giemsa or Papanicolaou) stained. • Usually evaluated by pathologist, or cytologist • Looking for double heads, pin heads, giant heads, or amorphous heads, double, coiled, or missing tails, etc. • Many sources of good pictures available Semen: Microscopic Analysis • Morphology • Normal = < 30% abnormal forms (NV varies considerably based on strictness of criteria. • WBC, RBC, bacteria presence should be noted & may indicate infection • Round cells (neutrophils and immature sperm) should be noted as well. Semen: Abnormal forms • 2 headed sperm • Sternheimer – Malbin stain • X 320 • Flat-headed sperm Semen: Microscopic Analysis • Sperm count • NV= 20 – 160 million/mL • Make 1 to 20 dilution with sodium bicarbonate and formalin, count 5 small squares (within the center large square) of the Neubauer hemacytometer. Semen: Microscopic Analysis • Sperm cell count • standard method to begin calculation of # cells (mature sperm) per microliter: ave. # cells counted x dilution # squares counted x volume of each square Semen: Microscopic Analysis • Microscopic examination • Example: 52 cells (mature sperm) x 20 • 5 (squares) x 0.004 This provides results as ___ cells / uL; Normal values are reported as ___ cells / mL • Must multiply X 1000 to convert uL to mL • = 52.0 x 106 / mL Semen: Microscopic Analysis • Metric • Internationalized system using decimals • Common system of measuring units • Length (M) , volume (L) , mass (G) , time (s), temperature (˚C) • Prefixes allow for mL, uL, etc. • International System of Units (SI) • Modified / modern form of metric system • Has 7 base units (but, unlike the original metric system does not include volume) • Other units, such as volume are ‘derived’ • Basic unit for volume is m3 • mL = cubic centimeter (cumm), uL = cubic millimeter (mm3 ) Semen: Sperm Agglutination • Observed while performing motility evaluation. • Few clumps are normal. • Distinctly head-to-head or tail-to-tail clumping may indicate the presence of antisperm antibodies. • IgG • IgA Semen: Sperm Viability • Eosin – Nigrosin stain supravital stain Add to drop of fresh sample Smear is made and allowed to dry Evaluated on oil immersion (1000x) Viable / live sperm do not take up the stain and remain colorless or blue-white • Non-viable / dead sperm stain orange-red • • • • • • Reported as % viable • Normal >75% Semen: Analysis • Other tests • Sperm penetration • Evaluates ability of sperm to make progressive movement through the cervical mucous. • Microbial testing • Increased WBC (>1 million/ mL) suggestive of infection • Aerobic and anaerobic cultures Semen: Chemical Analysis • pH • Measure within 1 hour of collection • Normal 7.2 8.0 • Acid Phosphatase • Used to evaluate the secretory function of the prostate • Also used in forensic analysis – as prostatic fluid acid phosphatase is higher than other fluids. (>200 units) • Fructose • Provides energy / nutrition to sperm • Indication of viability • Presence of fructose – screen using resorcinol test • Hormones • Testosterone, LH, FSH Post- Vasectomy Analysis • Post-vasectomy semen analysis • Specimens tested at monthly intervals starting 2 months post-vas. • 2 consecutive months of negative microscopic for sperm • Wet prep with phase microscopy • Examination of centrifuged specimen as well Semen: Forensic Analysis • Examination of fluid as to being semen (forensic) • Acid phosphatase – highly sensitive, as no other body fluid contains as high level (2500 units compared to @ 5 units) • ABO, HLA typing • DNA analysis • UV light scan, semen fluoresces green/white Semen: Analysis QC • Quality control • Previously little or no QC materials available • Commercial products now becoming available • Proficiency testing now available • CAP • American Association of Bioanalysts (AAB) Reference Listing Please credit those whose work and pictures I have used throughout these prsentations. Lillian Mundt & Kristy Shanahan, Graff’s Textbook of Urinalysis and Body Fluids, 2nd Ed. Susan Strassinger & Marjorie Di Lorenzo, Urinalysis and Body Fluids, 5th Ed. Wikipedia, the free encyclopedia www.wikibedia.org Urinalysis and Body Fluids CRg Unit 5 2 Pregnancy & Amniotic Fluid Testing Pregnancy Testing & Amniotic Fluid - objectives 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Describe HCG, explain its role in pregnancy testing, and identify causes for false negative and false positive results. Analyze the formation, composition, and physiology of amniotic fluid. State three (3) reasons for amniotic fluid analysis. Describe tests performed on amniotic fluid to determine risk of Hemoyltic Disease of the Fetus and Newborn (HDFN) and fetal maturity. Define amniocentesis and list special precautions needed for this procedure. Describe the handling and processing procedures for testing amniotic fluid. Explain the principle of spectrophotometric analysis of amniotic fluid for bilirubin and the interpretation of results as to level of risk to the fetus. Evaluate the L/S ratio including its significance and normal value in a mature fetus. Identify the significance of phosphatidylglycerol and the “foam” or “shake” test. Explain the significance of alpha fetal protein and cytogenetic analysis of amniotic fluid. Urine Pregnancy Testing • Pregnancy tests detect the hormone produced in pregnancy, beta-human chorionic gonadotropin hormone (β-hCG). • A natural hormone produced in very small quantities in all persons, male / female. • Following fertilization of an ovum, the special cells in the chorionic layer of the developing placenta produce increased amounts. • Levels essentially double daily, until a peak level is normally reached near the end of the first trimester. • The hormone begins showing up in the urine @ 8-10 days after fertilization (2-3 days after implantation of the embryo) Urine Pregnancy Testing • Pregnancy tests detect the increased amount of, betahuman chorionic gonadotropin hormone (β-hCG). • Pregnancy testing can be done on blood or urine. • Blood levels detected earlier and are more constant • Urine levels vary depending upon the state of hydration (first morning specimen or one that has SpGr > 1.015) Urine Pregnancy Testing (cont.) • Enzyme immunoassays (EIAs) are most popular methodology. • Can show a positive in as little as 10 days after conception. • Example of how results are reported: hCG negative or hCG positive • False results can occur • False negatives – generally due to testing too early • False positives • Misinterpretation of results , not following directions • Contamination with large amounts of blood, protein, bacterial contamination • True positive, but patient NOT pregnant • Trophoblastic tumors, choriocarcinoma, germ cell tumors, etc. Amniotic Fluid Physiology, Composition and Formation • Contained within the amnion surrounding the fetus). (The membranous sac • Function • Provides protective cushion • Allows exchange of water, nutrients, biochemical products • Formed by • • • • Maternal circulation/plasma (early) Transfer of water across placental membrane Metabolism of fetal cells Fetal urine • (after @ 36 weeks) Amniotic Fluid Physiology, Composition and Formation • Volume • 700-1200 mL @ 34 weeks. • Composition • Similar to maternal plasma with sloughed fetal cells. • Fetal urine increases creatinine, urea & uric acid • Rise in creatinine levels after 36th week can be used to evaluate fetal age o < 36 weeks = 1.5 – 2.0 mg/dL o > 36 weeks = > 2.0 mg/dL • Fetal lung secretions • Lecithin & sphingomyelin surfactants. Amniotic Fluid • Indications for analysis • Abnormal screening blood tests: maternal alpha fetal protein, human chorionic gonadotropin, unconjugated estriol • Metabolic disorders, such as Tay Sachs • Neural tube defects – such as spinal bifida or an encephalic • • • Abnormal chromosome analysis and history of genetic disorders - such as Down’s syndrome Abnormal ultrasound In later pregnancy for possible early delivery • Fetal lung maturity, hemolytic disease of the newborn (HDN), infection, confirmation of gestational age, fetal maturity, etc. Amniotic Fluid • Specimen collection • Amniocentesis (using ultrasound) • 16-42 weeks gestation • @ 20-30 mL through fine needle collected in sterile syringes • Immediately transfer into sterile tubes (brown colored for protection from light) • Puncture heals and liquid replenished within 48 hrs. Amniotic Fluid • General Handling and processing • Special precautions • Cytogenic study specimens at RT or 37 degrees • Fetal lung maturity testing specimens must be kept cold until tested • Specimens for bilirubin testing must be protected from light exposure and process immediately • Other chemistry tests require separation of cells, etc. from the fluid to preserve constituents. Amniotic Fluid • Color & Appearance • Normally colorless – pale yellow • Some turbidity is normal cellular debris, especially late in fetal development period. Amniotic Fluid • Color & Appearance cont. • Blood streaked - traumatic tap, abdominal hemorrage, intraamniotic hemorrhage • Fetal blood vs maternal blood: use Kleihauer-Betke • Yellow – bilirubin • Dark green- meconium • Dark red-brown – • probable fetal death has occurred. Amniotic Fluid testing • Cytogenic analysis • Determination of chromosomal abnormalities and certain metabolic defects • Picture by Clare O’Connor, PhD, Biology Dept., Boston College. • Prenatal Screens Detects Fetal Abnormalities., Nature Education. Amniotic Fluid testing • Cytogenic analysis • Determination of chromosomal abnormalities and certain metabolic defects • Cells cultured • Chromosomess evaluated for appropriate number and completeness • Some cells lysed and contents analyzed for enzymes to evaluate for metabolic defects, such as Tay Sachs. • Not done on all patients • Patient is >35yrs. or has history of problems • Increased AFP • Known carriers. Amniotic Fluid testing in HDN • Hemolytic Disease of the Newborn (HDN) • Also called Hemolytic Disease of the Fetus and Newborn (HDFN) or erythroblastosis fetalis. • “classical” case: Rh-negative mothers with Rh+ infants • Other red blood group discrepancies between Mom and Baby can also produce HDN • Fetal cells with antigen foreign to the Mom enter her circulation and stimulate the production of antibodies. • Danger increases with each exposure. Amniotic Fluid testing for Fetal Distress • Hemolytic Disease of the Newborn (HDN) • Maternal antibodies cross the placenta and destroy fetal cells with the corresponding antigen • Bilirubin from RBC destruction appears in the amniotic fluid • Some level occurs naturally from normal RBC catabolism • The amount of unconjugated bilirubin present correlates with the amount of RBC destruction Amniotic Fluid testing for Fetal Distress • Purpose of bilirubin testing on amniotic fluid: • Measurement of bilirubin is an indication of degree of hemolysis occurring in utero, therefore an indication of danger of anemia in the fetus. Amniotic Fluid testing for Fetal Distress • Bilirubin by spectrophotometric analysis • Scan fluid at increasing wavelengths • Plot readings against a baseline • Measure difference between baseline and peak bilirubin at 450 nn Plot difference on Liley graph, against gestational age Amniotic Fluid Testing for Neural Tube Defects • Neural Tube Defects • Anencephaly • Spinal bifida • Tests (these are usually tested together) • Alpha fetal protein (AFP) • Peaks at 16 weeks gestation • Acetylcholinesterase • **Test affected by presence of blood or hemolysis Amniotic Fluid Testing for Fetal Lung Maturity -To determine whether fetus is capable of surviving an early delivery. • Hyaline membrane disease • Also called neonatal respiratory distress syndrome • Major complication of early delivery & Most common cause for death of premature newborn. • Immature lungs lack of lung surfactants, which allow lung alveoli to be able to open during when breathing. • Surfactants decrease surface tension, permitting alveoli inflation. • Fetal lung surfactants include three phospholipids: • lecithin (also known as phosphatidylcholine), **major lung surfactant. • sphingomyelin, • phosphatidyl glycerol. • Many tests developed to assess for fetal lung maturity. Amniotic Fluid Testing for Fetal Lung Maturity • Shake test & Foam stability • Both tests utilize dilutions of amniotic fluid in 95% ethanol and look for formation of a persistent ring of foam / bubbles, an indication of total surfactant concentration. • Shake test – crude, fast, cheap and can be performed at bedside. Physician can make an immediate decision regarding safety of early delivery of infant. • 1:2 dilution (amniotic fluid : 95% ethyl alcohol), shake 15 seconds, If a complete ring of foam persists 15 minutes = positive test. • Foam stability index – places fixed amount of amniotic fluid in series of tubes with increasing amounts of 95% ethanol (from 0.43 to 0.55) • Dilutions are shaken vigorously and the higher concentration of 95% alcohol that is able to suppress a foam ring is known as the foam stability index • Foam stability index >0.47 indicates fetal lung maturity Amniotic Fluid Testing for Fetal Lung Maturity • Lamellar bodies • “packets” of surfactant lipids produced by pneumocytes • Size 1-5 um (slightly smaller than platelets) • Can run on automated cell counters (platelet mode) • Lamellar body count > 30,000 / uL is highly predictive of pulmonary maturity • Count < 10,000 suggest risk for RDS – respiratory distress syndrome • Test not affected by hemolyzed blood or meconium Amniotic Fluid Testing for Fetal Lung Maturity • Lecithin / Sphingomyelin ratio • Lecithin is the major lung surfactant • The role of sphingomyelin is not established • Levels equal until 33 weeks of gestation • @ 1/1 ratio • After 34 the week of gestation, lecithin production greatly increases as compared to the sphingomyelin • L/S ratio 2.0 or greater indicates lung maturity • 2X as much lecithin / spingomyelin Amniotic Fluid Testing for Fetal Lung Maturity • Phosphatidyl glycerol • Not detected until 35 week of gestation • Delayed in cases of maternal diabetes • Amniostat FLM - PG • Immunological test for phosphatidyl glycerol • Uses antibodies for detection, thereby not affected by the presence of hemolysis or blood Amniotic Fluid Testing for Fetal Lung Maturity • Microviscosity • Fluoresent dye binds with surfactants and albumin. • Test run on Abbot TDx and results correlate well with L / S ratio Amniotic Fluid Testing • Creatinine • Fetal age determination (at 36 weeks, fetal kidneys excrete >2.0 mg/dL creatinine) • • This test has been replaced by ultrasound measurements. Creatinine still used as: • Measurement as means of determining a fluid to be amniotic or urine. • Creatinine level up to 3.5 mg/dL & urea level @ 30 mg/dL can be found in amniotic fluid • Urine levels of creatinine @10 mg/dL and @ 300 mg/dL for urea. Urinalysis and Body Fluids CRg Unit 5 3 Sweat Fluid Analysis Sweat Fluid Analysis - objectives 1. Define cystic fibrosis (CF). 2. Describe the methodology of the sweat chloride test. 3. Analyze the sweat chloride values seen in patients suspected of having CF Cystic Fibrosis (CF) • Cystic fibrosis • 1/25 white Americans are carrier of CF gene • Autosomal recessive, affects @ 1/1500 – 1/2000 Caucasian births. • Most common fatal inherited disease of Americans • 1000 new cases diagnosed / year • Most patients diagnosed before 2 years of age • If diagnosed early, many will live to adulthood; but @ ½ die before age of 30. • Affects mucous secreting glands • Very thick mucous produced • Lungs, pancreas, GI tract, sweat glands CF – Symptoms vary: • CF Symptoms • Coughing due to respiratory distress & frequent lung infections • Viscous stools cause GI obstructions • Pancreatic insufficiencies • Leads to frequent greasy, bulky stools • Failure to thrive • Salty –tasting skin CF – Treatments vary: • CF Treatments: • Mycolytic agent • Bronchodilator to liquefy and expedite removal of mucous from lungs • Antibiotics • Anti-inflammatory medications such as ibuphrofen • Physical therapy – breathing exercises Sweat test - Laboratory Procedure • (Pilocarpine iontophoresis) • Pilocarpine – chemical that will induce sweating • Iontophoresis – mild electrical current • http://www.cff.org/AboutCF/Testing/SweatTest/ Sweat test - Laboratory Procedure • (Pilocarpine iontophoresis) • Pilocarpine – chemical that will induce sweating • Iontophoresis – mild electrical current Clean area Induce new sweat formation Collection on filter paper OR Collection in tube OR Directly measure on skin with chloride ion selective electrodes / ISEs • Test sweat for chloride concentration • • • • • http://www.cff.org/AboutCF/Testing/SweatTest/ Sweat Testing • Results: • Normal Sweat chloride levels < 30 mEq/L (mmol/L) • Sweat chloride levels of 40-70 mEq/L are borderline and must be repeated. • Sweat chloride (or sodium) levels greater than 50 mEq/L are consistently seen in 98% of CF patients. Reference Listing Please credit those whose work and pictures I have used throughout these prsentations. Lillian Mundt & Kristy Shanahan, Graff’s Textbook of Urinalysis and Body Fluids, 2nd Ed. Susan Strassinger & Marjorie Di Lorenzo, Urinalysis and Body Fluids, 5th Ed. Wikipedia, the free encyclopedia www.wikibedia.org Cystic Fibrosis Foundation www.cff.org/About CF/ Urinalysis and Body Fluids CRg Unit 5 4 Gastric Fluids Gastric Fluid Analysis - objectives 1. Describe the physiology and composition of gastric fluid; including the role of gastrin in its production. 2. List two (2) reasons for gastric fluid analysis. 3. Explain the special patient preparation that should occur before gastric fluid is analyzed. 4. Define or describe the Zollinger-Ellison Syndrome, anacidity, hypochloryhydia, and achlorhydria. 5. Describe the procedure for gastric acidity and state the clinical significance. 6. Describe gastric fluid drug screening and its clinical significance. Gastric Fluid - production • Physiology • Full stomach, presence of amino acids, stimulation by vagus nerve, other factors • Release of hormone Gastrin from stomach G cells • Gastrin stimulates release of digestive gastric fluids from the stomach parietal cells. • Inhibition / shut-down • Negative feed-back system • Presence of secreted HCl in stomach will inhibit gastrin release • Hormones somatostatin, glucagon, calcitonin and others Gastric Fluid - composition • Composition and formation • Produced by the parietal cells in the stomach under the hormonal influence of gastrin. • Normal makeup of gastric fluid: • • • • • * HCl, saliva, mucous, neutralizing chemicals, secretions from the intestines, bile & pancreas Gastric Fluid • Anacidity – lack of normal acidity • Sometimes called achlorhydria (hypochlorhydria) • Absence (decrease) of HCl in gastric secretions • Usually caused by • • • • Atrophy of gastric mucosa Gastric carcinoma Pernicious anemia Severe iron deficiency anemia Gastric Fluid testing • Indications for testing gastric fluids • Peptic ulcer evaluation • Gastritis – inflammation of stomach wall • Anacidity – inability to produce acid Gastric Fluid testing • Indications for testing gastric fluids • Zollinger-Ellison (Z-E) syndrome • Hypersecretion • Gastrin secreting neoplasm usually located within the pancreatic islets • Drug analysis • Suspicion of recent overdose • Examination of gastric fluid / aspirate for presence of pills, capsules, etc. generally performed by attending physician, or perhaps pathologist. • Literature provides some information regarding quantatitive testing, ie. HPLC, GLC/Mass Spectroscopy. Gastric Fluid testing • • • Specimen collection • Nasal or oral intubation • Fasting & avoid swallowing saliva Normal Specimen • ≤ 75 mL • Translucent, light gray • Slightly viscous Laboratory procedures • Gastric acidy (acid <4.0) pH paper • Drug screening Reference Listing Please credit those whose work and pictures I have used throughout these prsentations. Lillian Mundt & Kristy Shanahan, Graff’s Textbook of Urinalysis and Body Fluids, 2nd Ed. Susan Strassinger & Marjorie Di Lorenzo, Urinalysis and Body Fluids, 5th Ed. Wikipedia, the free encyclopedia www.wikibedia.org Mosby’s Medical Dictionary, 8th edition. @ 2009 Elsevier. Clinical Chemistry, Vol 22, 1906-1909. by American Association of Clinical Chemistry. Pub Med.gov. U.S. National Library of Medicine, National Institutes of Health. Urinalysis and Body Fluids CRg Unit 5 5 Feces & miscellaneous Feces • Feces • Composition • • • • • Bacteria, Cellulose & other undigested foodstuffs GI secretions, enzymes, bile pigments Cells Electrolytes and water Overview of Indications for Fecal Testing • GI bleeding • Occult blood • Suspicion of pathogenic bacterial or parasitic infections • Microscopic exam for leukocytes • O&P • Stool cultures • Diagnosis / confirmation of a malabsorption syndrome or liver and biliary duct disorder • Fecal fat & Fecal Carbohydrates • Meat fibers • Fetal hemoglobin Diarrhea • Diarrhea • • • • Common disorder of the GI tract Increased frequency (> 3x / day) Increased amount (>200 gm stool wt / day) Associated with infections, toxins, malabsorption issues, etc. Diarrhea • Diarrhea • Mechanisms of diarrhea: • 1. Secretory • Microbial infections o o o o o o o o Vibrio cholerae Some E. coli Clostridium Salmonella Shigella Staphylococcus Campylobacter Cryptosporidium • Drugs, laxatives • Inflammatory bowel disease / colitis • Endocrine disorders, malignancy, others Diarrhea • Diarrhea • Mechanisms of diarrhea: • 2. Osmotic imbalance • • • • Incomplete digestion / absorption Lactose intolerance Amebiasis, antibiotics, laxatives, antacids Irritable bowel syndrome, others Diarrhea • Diarrhea • Mechanisms of diarrhea: • 3. Altered motility • Hypermotility with decreased absorption • Irritable bowel syndrome, others • Ramifications – diarrhea can easily result in dehydration and critical electrolyte imbalances. Other Disorders of the GI Tract • Malabsorption • Abnormal digestion or absorption of one or more nutrients • May lead to malnutrition or anemia • Maldigestion • Impaired digestion due to lack of digestive enzymes Other Disorders of the GI Tract • Colorectal cancer • Relatively common cancer of GI tract • Associated with ‘occult’ / hidden blood loss • Pancreatic insufficiency and cystic fibrosis • Decreased pancreatic digestive enzymes • Trypsin • Chymotrypsin • Elastase I • Results in maldigestion Fecal Specimen Collection • • • • • • Patient needs detained instructions Clean container, avoid contamination with urine or toilet water Qualitative tests require only small amount of random sample Quantitative / timed specimens, may require collection over several days. May require entire sample during the time period (72 hr fecal fat) or small amounts taken over several days (O& P) In some tests, timing of collection is important Some tests require restrictions of diet (occult blood) Fecal Laboratory Procedures Color / Appearance Possible Cause(s) Brown (normal) Normal – presence of urobilin (from bacterial breakdown of urobilinogen / stercobilinogen Black *Upper GI bleeding, Iron therapy, or some medications Red *Lower GI bleeding. Beets, food coloring & some meds. Pale yellow, white, gray Giardia infection. Bile – duct obstruction. Barium sulfate Green Strongly green vegetables. Some oral antibiotics. Biliverdin Bulky / frothy Bile-duct obstruction. Pancreatic disorders Ribbon-like Intestinal constriction Colitis, dysentery, malignancy, constipation Mucous /blood streaked *Color varies shades of red to black depending upon where bleeding occurs in the GI tract. Fecal Laboratory Procedures • Microscopic Examination for WBC • Fecal leukocytes • Mucous with blood / pus often seen in dysentery and damage to intestinal wall. • Methylene blue, Wrights or Gram stain may be used to visualize WBCs. • Wrights best for cell differentiation • Can indicate pathogenic bacterial infection or ulcerative colitis • Neutrophils associated with bacterial infection • Eosinophils associated with amebic infestation. Fecal Laboratory Procedures • Microbiology tests • Gram stain – not much help. Stool full of gram negative rods (mostly E. coli.) • Cultures – must use selective media which restricts or prohibits the growth of normal flora, and allows pathogens to grow. • Salmonella, Shigella, Campylobacter, Yersinia, E. coli 0157, Clostridium difficile Fecal Laboratory Procedures • Microbiology tests • Ova & Parasites • • • • • • • Giardia Enterobius vermicularis (pinworm) Taenia sagenata Taenia solis D. latum H. nana .. Tapeworms Ascaris Fecal Laboratory Procedures • Blood in feces • Melana • A large amount of fecal blood • May be black, tarry stool • Lower GI tract bleeds usually bright red blood if not occult Fecal Laboratory Procedures • Fecal Occult Blood Testing (FOBT) • “Occult” = hidden • Detection of occult blood may indicate • Infection / inflammation / ulcers of GI tract • Intestinal Trauma / hemorrhoids / Bleeding gums • Colorectal cancer • The American Cancer society recommends testing on all those over age 50 years. Fecal Occult Blood Testing (FOBT) • Two samplings from 3 consecutive stools for a negative • Traditional screening tests based on detection of the *pseudoperoxidase activity of hemoglobin • Different chromagens have been used • Benzidine (most sensitive), ortho-toluidine, & *gum guaiac (least sensitive, but preferred as to limit false positives) • Hydrogen peroxide oxidizes a colorless compound to for a blue color. • View demonstration at: http://www.operationalmedicine.org/ed2/Video/Hemoccult.mpg Fecal Laboratory Procedures • Stool guaiac test / gFOBT • Diet restrictions • • • • No red meats, fish Turnips , Horseradish Melons, banannas, pears, plums Raw broccoli, & cauliflower • Other restrictions • No aspirin or other non-steroidal anti-inflammatory medications for @ 7 days prior to collections to prevent GI irritation • iron supplements avoided for 3 days • High Vitamin C levels will reduce (False negative Rx) peroxidase activity iFOBT • • Immunochemical fecal occult blood (iFOBT) Fecal Immunochemical Testing (FIT) • Hemoccult ICT(commercial product name) • • • • Specific for globin portion of human hemoglobin Uses anti-human hemoglobin antibodies No dietary or drug restrictions Most sensitive to lower GI bleeding (patients with upper GI bleeding, such as ulcer would not react as blood has been digested) • Although many studies are in progress comparing the iFOBT and the traditional guiac , this test is quickly replacing the traditional fecal occult blood test! Feces - fecal fat • Fecal Fat – steatorrhea • Notable characteristics • Floats in water • Pale and greasy oily appearance • Foul-smelling • Causes • Decreased production of pancreatic enzymes • Absence of bile salts • Malabsorption syndromes • • • • bacterial overgrowth, intestinal resection celiac disease, tropical sprue lymphoma, Crohn disease, Whipple disease, and giardiasis. Feces - fecal fat testing • Patient preparation • Normal diet with normal level of fats • No contamination by oils, suppositories, or creams (could cause false positives) • Qualitative method • 2 procedures • Neutral fats (triglycerides) • Soaps and fatty acids • Sudan III/IV or Oil red O stain • Examine microscopically for large orange - red fat droplets. Feces - fecal fat testing • Quantitative method • To follow up a positive quantatitive test • Dietary requirements • Requires adherence to a diet of 100g/ day fat intake before and during test collection. • Chemistry dept – usually sent to reference lab • 3day collection (72 hours) • Test methods • Van de Kamer – classical titration Use sodium hydroxide to chemically titrate the amount of fat. • Acid steatocrit • Near infra-red spectroscopy Feces • APT - fetal hemoglobin • To determine whether blood found in newborn’s vomitus or stool is their own, or from the Mom. • Testing makes use of fact that baby blood (Hgb F) cells are resistant to lysing with sodium hydroxide & remain pink, while mom adult (Hgb A) cells lyse changing from the pink to yellow - brown. Feces • Fecal enzymes • Pancreatic insufficiency & cystic fibrosis • Pancreatic – associated enzymes • Trypsin • Classic trypsin test – series of diluted stool specimens are placed on x-ray paper (has a gelatin coating). After incubation, the stool is rinsed off and the paper evaluated to determine the dilution at which no gelatin has been digested by the protease trypsin . TEST NOT SENSITIVE • Chymotrypsin – more sensitive and can be measured spectrophotometrically • Elastase I • pancreas specific enzyme not affected by motility or other mucosal issues • Immunoassay procedure provides higher degree of specificity Feces - Fecal Carbohydrates • Fecal carbohydrates. • Celiac disease – inability to absorb carbohydrates • Lactose intolerance – lack enzymes to digest • Inflammatory necrotizing entrocolitis – rare, but very serious condition, most often occurs in premature infants • Increased carbohydrates in stool results in osmotic diarrhea. • Disaccharides (lactose is example) in the large intestine and bowel are osmotically active and cause movement of a large amount of water into the intestine. • Clinitest to detect the carbohydrate • Fecal pH to determine increased acid level • Stool pH normally @ 7-8 • pH 5.5 – 6 indicates increased acid Bronchial Washings & Bronchoalveolar Lavage • Fiberoptic bronchoscope placed in airway can be used to obtain specimen. • Or sterile saline infused (lavage procedure) and retrieved for analysis. - Results may be as good as biopsy. • Specimens usually sent to cytology / pathology to be examined for malignancy. • Occasionally, they are examined for other cells: • macrophages (60-80%), • lymphs, up to 10% • neutrophils up to 21% • eosinophils < 1 % • bronchial epithelial cells, • squamous cells • OR, more often cultured for microorganisms. Other miscellaneous fluids. • Nasal smears • Hansel stain for eosinophils • Cyst fluids – cells, and organisms • Tears – eosinophils • Breast milk – eosinophils. • always can culture them. Reference Listing Please credit those whose work and pictures I have used throughout these prsentations. Lillian Mundt & Kristy Shanahan, Graff’s Textbook of Urinalysis and Body Fluids, 2nd Ed. Susan Strassinger & Marjorie Di Lorenzo, Urinalysis and Body Fluids, 5th Ed. Wikipedia, the free encyclopedia www.wikibedia.org Urinalysis and Body Fluids Unit 5 6 Vaginal Secretions CRg Vaginal Fluids - objectives 1. 2. 3. 4. 5. Define and list at least three (3) symptoms of vaginitis. Identify at least two (2) sources of error that can occur during the collection and processing of vaginal wet prep specimens. List three (3) common causes of infectious vaginitis. Describe "clue cells" and explain the significance of finding them in a vaginal wet prep. Evaluate the test for estrogenic activity including the appearance of positive and negative results. Vaginal Secretions • Normal secretions • Clear mucus • May turn slightly white or pale yellow when exposed to air • Healthy vagina - Lactobacillus species predominates • pH< 4.5 (3.8-4.5) • Amount / volume varies through menstrual cycle • Normal microscopic exam • Abnormal changes • Color • Consistency • Amount Normal Wet prep • No symptoms • Lactobacillus (normal) • Normal discharge 108 Vaginitis • Vaginitis • - inflammation or infection of the vulva and vagina • NOT a specific disease, but is a very common reason women seek medical attention • Estimated 1/3 to ½ outpatient visits by women • Can occur in all age groups, sexually active as well as sexually non-active. • Common symptoms • • • • • Vaginal discharge Foul smell Itching Spotting Pain 109 Vaginitis - evaluation • Patient history • Marital or relationship status • Timeline of when symptoms began, etc. • • • Symptoms / complaint(s) Physical examination Tests • • • • • Physical properties Vaginal pH Microscopic exam / Wet Prep Amine (Whiff) test Cultures, if warranted 110 Vaginitis • Two (major) types • Non- infectious • May be caused by soaps ( no bubble baths ladies !), chemicals, foreign objects, allergies to condoms / lubricants etc. • Infectious (makes up 90% of all cases) • Fungal / yeast • Parasitic – Trichomonas vaginalis • Bacterial 111 Vaginitis • Specimen – Vaginal Wet Prep • Sterile swab (moistened with normal saline) • Must process these immediately, ie within 5 minutes • Swab in tube with @ ½ mL normal saline, or Ringer’s lactate • Keeps organisms from drying out if delay is expected • Special collection procedures: Microbiology cultures for gonorrhea (GC) must be placed in special transport media immediately. • This microbiology testing being replaced by molecular diagnostics • Collection / processing errors • Insufficient specimen / poor collection • Swabs / slide drying out 112 Vaginitis - testing • vaginal pH • Most important preliminary test • Normal (childbearing age) < 4.5 • pH paper 113 Vaginitis - testing • Microscopic exam / Saline Wet Prep • Sample mixed with saline examined microscopically to look for • Budding yeast with elongated pseudohyphae • Motile trichomonads & increased segmented neutrophils • PMNs & Clue cells 114 Vaginitis - testing • Microscopic exam / Saline Wet Prep • Limitations • Skill of collection • Transport time • Trichomonas organisms die / become immotile • Skill of technician • New wave in laboratory testing • Immunologic • Molecular diagnostic / pcr 115 Vaginitis - testing • Amine (Whiff) test • Also called potassium hydroxide or KOH preparation • Vaginal fluid & 10% KOH placed on a slide • Fumes from the slide are smelled to detect presence of ‘fishy odor’ (trimethylamine) . • Presumptive for bacterial vaginosis, though can also be positive for trichomonal vaginosis 116 Vaginitis - suspect yeast (candidiasis) • Candida albicans • Commonly causes a majority of cases • Alteration of normal vaginal flora o antibiotic regimens o immunocompromised patients • Thick white, clumpy or “curd-like” discharge. • Laboratory findings • Normal vaginal pH • Identification of yeast cells and elongated pseudohyphae (mycelia forms) • saline wet mounts • 10% KOH wet preps • Gram stain 117 Vaginitis - suspect:Trichomonas vaginalis • Trichomonas vaginalis • Parasitic vaginitis Free- living organism • Swimming / bathing in contaminated water • Sexually transmitted • Symptomatic - Yellow-Green frothy discharge; or may be asymptomatic • Organism seen in urine or on wet-prep • In males – sexually transmitted urogenital infection • Usually asymptomatic • Organism may be detected in urine microscopic T. vaginalis - testing / detection • Laboratory findings • Wet-prep microscopic • Single celled flagellate demonstrating jerky movements • @ size of WBC, but no nucleus and actively motile - unless specimen is old, dry or cold. • May demonstrate WBCs • • • DNA and immunological tests Elevated vaginal pH Positive amine / “whiff” test Vaginosis – suspect bacteria • • • Healthy vagina - Lactobacillus species predominates Bacterial vaginosis • Gardnerella vaginalis • Mobiluncus species • Prevotella species (anaerobes) Characteristics (*Amsel criteria) • *Homogenous vaginal discharge • Amount & Color may vary, but often gray / off-white • Usually thin in consistency and malodorous. • Lack of WBCs, but increased epithelial cell exfoliation • *“Clue cells” (make up 20+%) – most reliable finding • *Vaginal pH > 4.5 • *Positive amine test in the KOH prep “Clue cells” Normal examples Clue cells 121 Vaginitis – testing summary Observation / test Candidia vaginatis yeast Trichomonas vaginalis Bacterial Appearance Thick white, clumpy / curdlike Green-yellow & frothy Thin, gray homogenous pH < 4.5 >4.5 > 4.5 Wet Prep microscopic Budding yeast and pseudohyphae Motile trichomonads & PMNs > 20% Clue cells identified Amine (Whiff) test with 10% KOH Negative Negative, or Positive Positive: fishy odor DNA & immunological tests available Amsel criteria: at least 3 of 4 must be positive. Miscellaneous 122 Summary • From the lab’s perspective – 3 main causes for vaginitis • Yeast infection / candidiasis • Candidia albicans / other species possible • Trichomonas vaginalis • Bacterial • From disturbance of normal flora (ie decreased lactobacillus) that allows overgrowth of mixed flora, ie Gardnerella vaginalis and others • Gardnerella – results in ‘clue cells’ • Known pathogens, ie gonorrhea 123 Fern test • Test for estrogenic activity • Cervical mucous smeared on glass slide and allowed to dry • Examine under the microscope – look for fern-like appearance / pattern • Seen during times of increased estrogen – as occurs at time of ovulation. • Also done to see if there has been premature leakage of amniotic fluid - as it will also make a fern pattern due to its protein and sodium chloride content. 124 Fern test – positive reactions 125 Fern test – negative reaction 126 Wet preps - 1 • No symptoms • Lactobacillus (normal) • Normal discharge 127 Wet preps - 2 • • • • • pH <4.5 (normal) KOH microscopic negative & Whiff test negative (no amine odor) Normal epithelial cells Predominately lactobacillus Rare WBC 128 Wet preps - 3 • • • • • Positive clue cells pH > 4.5 Whiff test positive KOH microscopic negative Normal lactobacilli have been overrun by Gardnerella vaginalis and other organisms 129 Wet preps - 4 • Positive KOH microscopy • Whiff test negative • No amine odor when mixed with the KOH • Vaginal pH <4.5 • Moderate – increased discharge • White to light yellow, • Etiology – Candida albicans / Candida species 130 Wet preps - 5 • • • • Microscopy – positive for motile ‘trich’ Whiff test often positive Vaginal pH >5.0 Discharge – greatly increased • Green / yellow purulent, may appear foamy • Etiology – Trichomonas vaginalis 131 Summary • Yeast - Candidiasis • Candida albicans / other species possible • Microscopic shows mycelia forms 132 Summary • Trichomoniasis • Trichomonas vaginallis • @ size of WBC (slide on Rt), but no nucleus and actively motile • Unless specimen is old, dry or cold 133 Reference Listing • • Lillian Mundt & Kristy Shanahan, Graff’s Textbook of Urinalysis and Body Fluids, 2nd Ed. Susan Strassinger & Marjorie Di Lorenzo, Urinalysis and Body Fluids, 5th Ed. Wikipedia, the free encyclopedia www.wikibedia.org eMedicine from Webb MD http://emedicine.medscape.com/article/257141-diagnosis Family Practice notebook.com Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med. 1983 Jan;74(1):14-22. [Medline] Seattle STD/HIV Prevention and Training Center, Washington State Dept. of Health • • http://depts.washington.edu/nnptc/online_training/std_handbook/gallery/pages/cluecel ls.html