Using modeling to predict the optimal
advertisement

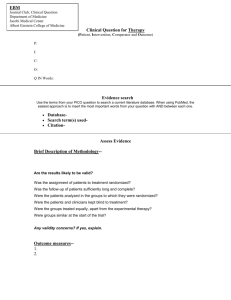
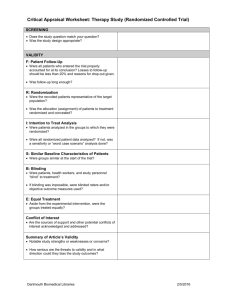
Comparative Effectiveness Research Shalini Kulasingam, PhD University of Minnesota Overview Learning objectives Background: why do we need a “special type” of research agenda? Definition: comparative effectiveness research What areas/conditions have been prioritized for study? Role of nursing? Methods for conducting comparative effectiveness research Examples RCTs Observational studies Simulation modeling Funding Learning Objectives Why there is a need for CER? Priority CER topics Study designs for conducting CER Examples of CER studies Background Health care expenditures were $2.4 trillion in 2008 and are projected to grow by an average of 6.2 percent per year for the next 10 years, more than triple the projected rate of overall gross domestic product (GDP) growth (Sisko et al., 2009) The Congressional Budget Office (CBO) projects that under current law, health care will consume more than 30 percent of GDP by 2035 (CBO, 2008). IOM report, 2009 Background Regional variations in treatment patterns and cost growth provide deeper insight into the need for more informed medical decision making. Patients in the highest-spending regions of the country receive 60 percent more health services than those in the lowest-spending regions, yet this additional care is not associated with improved outcomes (Fisher et al., 2003). Background Research suggests that physicians in higher-spending areas are more likely than physicians in other regions to recommend costly interventions that have not been definitively shown to be effective (Fisher et al., 2009). Nationwide, the Institute of Medicine (IOM) has estimated that less than half of all treatments delivered today are supported by evidence (IOM, 2007). Background A recent review of practice guidelines developed by the American College of Cardiology and the American Heart Association found that relatively few recommendations were based on high-quality evidence—randomized controlled trials, for instance—and many were based solely on expert opinion, individual case studies, or standard of care (Tricoci et al., 2009). What is comparative effectiveness research? Comparative effectiveness research (CER) is the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat, and monitor a clinical condition or to improve the delivery of care. The purpose of CER is to assist consumers, clinicians, purchasers, and policy makers to make informed decisions that will improve health care at both the individual and population levels. CER Summary and Investment in Research How good is the intervention/treatment/test? In what patients? Under what circumstances? American Recovery and Reinvestment Act of 2009 $1.1 billion “down payment” to support CER $400 million given to the NIH $300 million given to the AHRQ $400 million to Health and Human Services What are the priority areas for research? The American Recovery and Reinvestment Act of 2009 called on the Institute of Medicine to recommend a list of priority topics to be the initial focus of a new national investment in comparative effectiveness research. The IOM’s recommendations are contained in the report, Initial National Priorities for Comparative Effectiveness Research. What are the priority areas for research? Treatment strategies for atrial fibrillation Treatment for hearing loss Primary prevention versus clinical treatments in preventing falls in older adults Biologics for inflammatory diseases Upper endoscopy for patients with gastroesophageal reflux disease Dissemination and translation of techniques for use of CER by clinicians IOM, 2009 What are the priority areas for research? Comprehensive care programs for people with chronic disease Interventions for MRSA Strategies to reduce health care associated infections Management of prostate cancer Registry for lower back pain Detection and management of dementia in a community setting IOM, 2009 What are the priority areas for research? Management of behavioral disorders associated with dementia School-based interventions for treating obesity in children Interventions to reduce hypertension, obesity etc. in urban poor and Native American populations Management strategies for ductal carcinoma in-situ Use of imaging technologies for cancer Genetic and biomarkers for cancer IOM, 2009 What are the priority areas for research? Prevention of dental caries in children Treatment strategies for children with ADHD Management of serious emotional conditions in children and adults Interventions to reduce health disparities Literacy sensitive disease management Interventions to reduce adverse birth outcomes in women especially African American women Prevention of unintended pregnancies IOM, 2009 Role of Nursing Statement by MaryJean Schumann, Chief Program Officer, ANA, 2009 Perspective is based on two types of nurses the registered nurse providing direct care the advanced practice registered nurse Certified Registered Nurse-Anesthetists (CRNAs) who provide critical anesthesia services; Clinical Nurse Specialists (CNSs) who provide acute care expertise for complex patients; Certified Nurse-Midwives (CNMs) who provide health care to women across the lifespan; Nurse Practitioners (NPs) who deliver a wide range of primary care services. Role of Nursing “Nursing’s holistic view – attention to the whole person – makes nurses particularly effective in advancing these priorities. Nurses, with their expertise in health promotion, disease prevention, and health literacy, can contribute to changing the current sickness care system into a true health care system.” MaryJean Schumann,, ANA,. 2009 Setting priorities based on ANArelated work and data National Quality Forum National Priorities and Goals Six Priority areas: What are the most effective tools and systems to engage patients in their care? What are the most effective models for care coordination? How do we reduce 30-day readmission rates? How is palliative care best provided? “How do we eliminate unnecessary or risky care? “Improve health by ensuring that patients receive the most effective preventive services recommended by the U.S. Preventive Services Task Force. “ MaryJean Schumann,, ANA,. 2009 Setting priorities based on ANA related work and data CER priorities based on quality indicators developed by ANA 1998, ANA established the National Database of Nursing Quality Indicators® (NDNQI®), the only national database that provides nursing data and patient outcomes at the unit level where care occurs. Data are collected on structure, process and outcome measures in approximately 1400 hospitals of all sizes, in all 50 states and the District of Columbia. Data is collected on 17 measures, 11 of which have been endorsed by the National Quality Forum. MaryJean Schumann,, ANA,. 2009 Area NOT recommended for further research A Cochrane review concluded that “appropriately trained nurses can produce as high quality care as primary care doctors and achieve as good health outcomes for patients.” It was noted that the research available is limited and some may call for further comparative studies. There are, however, no other professionals who have been subjected to the depth of study that NPs and CNMs have, and we question the need to expend limited resources on additional studies comparing professional groups, though we stand ready to play a role in the design and conduct of such studies should they be deemed necessary. MaryJean Schumann, ANA. 2009 Study Designs for CER Synthesis of existing data Analysis of observational data Randomized controlled trials Study Design Synthesis of existing data Systematic review Meta-analysis Decision modeling Study Design Observational data Administrative claims Electronic medical records Registries Case control or cohort studies Study Design Randomized controlled trial Luce et al. Annals Internal Medicine, 2009 How to change RCTs for comparative effectiveness research Analytic and operational efficiency Reduce costs of running a trial, and be able to up date trials on an ongoing basis, dropping tests/drugs/interventions that are not promising Accomplish this using Bayesian approaches Pragmatic clinical trial Study Design Pragmatic RCT CER objective is to provide information to help patients, consumers, clinicians, and payers make informed decisions. Trials tend to exclude relevant patient populations, commonly used comparators, long term outcomes, and non-expert providers Clinically effective comparators Study patients with common co-morbid conditions Diverse study patients Providers from community settings Provider and patient chosen outcomes Potential Sequence for Identifying and Proposing CER IOM list of priority topics lists those that are most likely to get funded IOM report notes that systematic reviews and meta-analyses provide information on areas for further study. Question: can you use take a topic from the IOM priority list and identify a study for grant purposes? Examples of CER Studies Detection of dementia in a community setting Systematic review Decision modeling Pragmatic trial Patient falls Systematic review Patient record review Randomized controlled trial – with pragmatic aspects Detection of dementia in a community setting The original CMS-sponsored TA Aim: Assess the benefits of FDG-PET scanning in patients with dementia, with mild cognitive impairment (MCI) and in asymptomatic patients with a family history of AD, subsequent to the standard evaluation as described in the American Academy of Neurology (AAN) guidelines. CMS requested that the AHRQ identify an Evidence Practice Center to perform a Technology Assessment (TA) Duke EPC assigned the TA in 2001 Methods of the original TA Literature review Decision model to provide an understanding of the decisional context http://www.cms.hhs.gov/coverage/download/id64.pdf Direct inference Delayed progression Test Decreased mortality Indirect inference: causal pathway True - Test False - True + Treat False + Adverse Event Delayed progression Decreased mortality Model: Part 1 Truepos AD sens prevAD PET Falseneg AD, treat # Falsepos NoAD # AD, no treat # Trueneg No AD, treat spec AD Mild dementia No PET/Rx Truepos No AD, no treat Falsepos AD, treat Falseneg No AD, treat Trueneg AD, no treat prevAD NoAD # AD No PET/NoRx prevAD NoAD # No AD, no treat Test performance No AD by clinical evaluation Test + AD by clinical evaluation True + Test - False - True - False + Sensitivity = True +/AD Specificity = True - /No AD ROC curve of PET test accuracy based on the literature review Tree results: mild dementia True + (%) False + (%) False – (%) True – (%) Correct (%) No PET/ Rx 56 44 0 0 56 PET/ Rx+ 49 6 7 38 87 No PET/ no Rx 0 0 56 44 44 Asymptomatic MCI Model: Part 2 Dead Mild Dementia Moderate Dementia Severe Dementia Illustrative patient history Year 1 Asy MCI MiD MoD SeD D 2 Asy MCI MiD MoD SeD D 3 Asy MCI MiD MoD SeD D 4 Asy MCI MiD MoD SeD D Markov results: mild dementia QALY LE SDFLE No PET/ Rx 4.10 7.89 4.02 PET/ Rx+ No PET/ no Rx 4.09 7.88 4.00 4.02 7.82 3.86 Primary conclusion PET could improve the overall accuracy compared to accuracy of an exam based on AAN guidelines. Treatment based on an AAN-recommended examination leads to better health outcomes than treatment based on PET results How can this make sense? While net accuracy with PET may be better, this is because there are many fewer false positives but a few more false negatives Incorrectly not treating (due to a false negative result a patient misses an opportunity for a Rx benefit) is worse than incorrectly treating (the patient unnecessarily receives medication, however the Rx is relatively benign, may be beneficial even if they don’t have AD, and the personal downside is that their cognitive impairment/disability is not correctly labeled) When testing is preferred 1. If a new treatment becomes available that is not only more effective than AChEIs but is also associated with a risk of severe adverse effects. When testing is preferred 2.If testing could be demonstrated to be a better reference standard than an examination based on AAN guidelines. (i.e., testing would need to better distinguish patients who respond to therapy than is possible with a standard examination.) When testing is preferred 3.If the results have demonstrable benefits beyond informing AChEI use. This “value of knowing” could have both positive and negative components. A research agenda in service to decision-making Designs: Minimize bias Maximize generalizability Why not a trial? In particular, why not a pragmatic clinical trial? Kulasingam et al. Am J Alzheimers Dis Other Demen. 2006 Design of a pragmatic clinical trial Matched Communities R PET reimbursed Patients identified, 1 page evaluation completed* PET not reimbursed Medicare claims (primary outcome = resource use from index date to 3 months) * Medicare claims at the community-level for individuals with relevant ICD codes will be examined (see Methods) Design of a pragmatic clinical trial Design: A demonstration project in which matched communities are randomly assigned to have FDG-PET reimbursed by Medicare or not. Allocation: Communities are allocated to intervention or control by concealed randomization. Blinding: Blinded outcome assessors/data collectors, biostatisticians. Follow-up period: 3 years Setting: Communities in which state-of-the-science FDG-PET is reasonably available for various Medicare-covered clinical applications. Patients: Patients will be enrolled based on (a) age ≥ 65, (b) free-living, (c) presenting without prior specific workup for a complaint of memory deficit, and (d) the physician specifies that some degree of workup is planned. Design of a pragmatic clinical trial Intervention: All participating communities will have a general education program regarding the diagnosis and evaluation of cognitive impairment, and will be informed how to enroll patients into the study. To ensure comparable patient identification in all communities, providers will be compensated on completion of a basic evaluation form for an eligible patient. Communities randomized to have FDG-PET reimbursed will have payment coordinated by the regional Medicare carrier. Communities randomized to not have FDG-PET reimbursed by Medicare will not have restrictions on FDG-PET if covered under other payment arrangements. Design of a pragmatic clinical trial Measures: Measures will consist of (a) a simple (i.e., 1 page) form completed on the date of presentation (index date) by the patient’s provider regarding basic demographic and clinical features, diagnosis/further diagnostic plan, treatment plan, and prognosis; and (b) resource utilization related to initial evaluation and management of individuals with CI, as assessed via linked Medicare claims files. Cumulative resource costs from the index date to three-months (short-term) will serve as the primary outcome measure for purposes of sample size calculation. Additional measures will include resource counts (e.g., imaging studies, specialty referrals, laboratory testing, and so on), FDGPET diffusion (in terms of proportion of candidates who have had a FDG-PET), as well as trajectory of resource use over time. Review of Steps Priority topic Literature review/decision modeling to identify areas for further research Proposed pragmatic clinical trial Patient Falls Potential Areas of Research “Patient falls are one example of how our quality work informs a CER priority. As an outcome of interest, falls are of critical importance, highlighted by CMS’ decision to include falls on the list of Hospital Acquired Conditions for which they no longer pay. There are many validated fall assessment tools, but there has not, to date, been any comparative research on the tools to determine which is more effective in determining fall risk assessment and which interventions are most effective for preventing falls.” MaryJane Schumann, ANA, 2009 Falls Coussement J et al. American Geriatrics Society, 2008 Interventions for Preventing Falls in Acute- and Chronic-Care Hospitals: A Systematic Review and Meta-Analysis Goal: To determine the characteristics and the effectiveness of hospital fall prevention programs Results: Review showed that most studies were conducted on long-stay (mean length of stay (LOS) >1.5 years) and rehabilitation units (mean LOS 36.9 days). Results: For analysis of the number of falls, one unifactorial and two multifactorial studies showed a significant reduction of 30% to 49% in the intervention group, with the greatest effect obtained in the unifactorial study that assessed a pharmacological intervention. Falls Lakatos BE et al. Psychosomatics, 2009 Objective: to determine the prevalence of diagnosed and undiagnosed delirium in patients who fell during their hospital stay. Study design: Retrospective chart review Methods: Falls were categorized by their severity (i.e., minor, moderate, and major). Demographic information, patient outcomes, and diagnostic criteria for delirium (per DSM–IV) were collected on the day of admission, the day of the fall, and the 2 days preceding the patient’s fall Results: Falls in the general hospital were associated with delirium (both diagnosed and undiagnosed), advanced age, and specific surgical procedures Falls Vass et al. Reducing Falls in In-patient Elderly, Trials, 2009 Summary of an RCT that aims to reduce falls in an elderly inpatient population in an acute care setting. Background: More than half of all in-patient falls in elderly people in acute care settings occur at the bedside, during transfers or whilst getting up to go to the toilet. In the majority of cases these falls are un-witnessed. Background: New patient monitoring technologies have the potential to offer advances in fall prevention. Bedside sensor equipment can alert staff, not in the immediate vicinity, to a potential problem and avert a fall. However no studies utilizing this assistive technology have demonstrated a significant reduction in falls rates in a randomized controlled trial setting. RCT for fall prevention The research design is an individual patient randomized controlled trial of bedside chair and bed pressure sensors, incorporating a radio-paging alerting mode to alert staff to patients rising from their bed or chair, across five acute elderly care wards in Nottingham University Hospitals NHS Trust. Participants will be randomized to bedside chair and bed sensors or to usual care (without the use of sensors). The primary outcome is the number of bedside inpatient falls. RCT – proposed data collection Data collection Baseline Discharge Demographics X Previous falls/med. Hx. X Cognitive Ability X X Quality of Life X X Activities of Daily Living X X Discharge Destination X X Length of stay X X Fear of falling questionnaire X X Total # of in-patient falls X X Vass et al. Trials, 2009 Review of Steps Priority topic Meta-analysis and chart review study to identify gaps Proposed clinical trial Pragmatic aspects are community setting Range of outcomes Conclusions CER is new focus of funding at the NIH and AHRQ List of priority topics (IOM) Evidence reports and meta-analyses can provide information on gaps in knowledge base that require further study (AHRQ) Search grants.gov for RFAs or other announcements re: new funding opportunities Lots of potential colleagues/collaborators at the U MN School of Public Health School of Medicine School of Dentistry Funding and Acknowledgements Shalini Kulasingam is supported by NCI grant K07-CA113773 Previously funded by: Grants: Merck, CSL-Australia, SP-MSD, CDC, NIH, mtm Consultant: SP-MSD, CSL – New Zealand, Medtronic Collaborators Evan Myers, Duke University George Sawaya, University of California, San Francisco Joy Melnikow, University of California, Davis Mark Schiffman, Philip Castle, NCI Eduardo Franco, Raghu Rajan, McGill University Laura Koutsky and Akhila Balasubramanian, University of Washington Patti Gravitt, Johns Hopkins University Levi Downs, Rahel Ghebre, Ruby Nguyen, Karen Kuntz, University of Minnesota