phlebotomy
advertisement

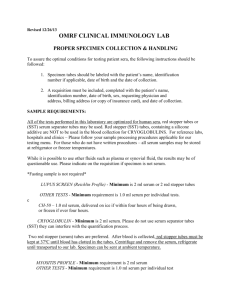
PHLEBOTOMY Created By: Michelle Huffman Introduction to Blood Collection Objectives • • • • • • • • • Recognize the Importance of Correct Blood Collection Factors That Influence Integrity of Blood Specimen Safety Precautions Related to Blood Collection Differentiate Between Whole Blood, Plasma and Serum Actions of Anticoagulants, to Prevent Blood Coagulation Describe the Appearance of Hemolyzed, Icteric, and Lipemic Specimen Differentiate Between Arterial, Venous and Capillary Blood Special Specimen Handling Procedures Purpose of Quality Assurance in Blood Collection SAFETY PRECAUTIONS In addition to safety precautions specifically associated with blood collection. Personnel must observe all STANDARD precautions required in Patient Care . • Wearing appropriate personnel protective equipment • Observation of Isolation Practices • Hand Washing (15-20 secs.) and BETWEEN Patients • Using ONLY Needles with Safety Devices in the Intended Manner • Using only the recommended transfer devices to transfer blood from syringes to evacuated tubes • Disposal of Entire Assembled Tube Holder and Needle After Use • Recording All Accidental Needlesticks and Exposures as Required • Disposal of Contaminated Materials in Designated Biohazard Containers • Decontamination of Surfaces Using an Approved Disinfectant. NOTE: Blood Collection poses a serious risk for exposure to blood borne pathogens (ex. HIV, hepatitis B, hepatitis C, Most blood-borne pathogen exposures associated with blood collection occur as a result of accidental puncture with a contaminated needle. Types of Patient Isolation • Strict Isolation – required for a patient with highly contagious diseases that can be spread by direct contact and through the air. (ex. Chicken pox, diphtheria) GLOVES, GOWN and MASK • Contact Isolation - indicated for highly transmissible disease that is spread primarily by direct contact, such as influenza and infections with antibiotic-resistant bacteria. GLOVES, GOWN and MASK • Respiratory Isolation – Patient with infection that can be spread via droplets or through the air, such as whooping cough (pertussis), meningicoccal meningitis and Haemophilus influenza. GLOVES and MASK • AFB-TB Isolation – (acid-fast bacillus) Patient with active tuberculosis. N95 Respirator Mask, GOWN and GLOVES What Does Being A Phlebotomist Mean?? Factors that are the responsibility of the collector and include: • • • • • • • • • • Monitoring of Specimen Ordering Correct Patient Identification Patient Communication and Patient Safety Patient Preparation Timing of Collections Phlebotomy Equipment Collection Techniques Specimen Labeling Specimen Transportation to the Laboratory Specimen Processing Importance of correct specimen collection • Laboratory testing of blood specimens is VITAL to the correct DIAGNOSIS, TREATMENT and MONITORING of a patient’s condition. • Although the primary concern of personnel collecting blood specimens is understandably to obtain the specimen, failure to adhere to the collection procedure can compromise the integrity of a successfully collected specimen. Note: approximately 56% of laboratory errors occurs during the preanalytical phase (process that occurs before testing) Types of Specimens The laboratory refers to blood specimens in terms of WHOLE BLOOD, PLASMA and SERUM. WHOLE BLOOD - A whole blood specimen contains erythrocytes (red blood cells), leukocytes (white blood cells), and thrombocytes (platelets) suspended in plasma and essentially represents blood as it circulates through the body. (CBC, blood typing) Note: Majority of laboratory tests are performed on the liquid portion of blood (plasma or serum) which contain substances, such as proteins, enzymes, organic and inorganic chemicals and antibodies. PLASMA – Plasma is the liquid portion of blood that has not clotted. Plasma is often defined as the liquid portion of blood that contains fibrinogen and other clotting factors. Plasma is obtained by centrifugation of unclotted specimens. SERUM - Serum is the liquid portion remaining after clotting has occurred. Serum does not contain fibrinogen and other clotting factors. Serum is obtained by centrifugation of clotted specimens. NOTE: • The presence or absence of anticoagulants in the tubes into which blood specimens are placed determines the type of specimen available for testing. • WHOLE BLOOD and PLASMA – require an anticoagulant to prevent clot formation • SERUM – is obtained from tubes that DO NOT contain and anticoagulant. EVACUATED TUBES AND ORDER OF DRAW • Evacuated tubes come in a variety of sizes, volumes and colors. The tubes are labeled with the type of anticoagulant or additive, the draw volume, and the expiration date. • Evacuated tubes have color coded rubber stoppers or plastic shields covering the stoppers. • Evacuated tubes fill automatically because of the premeasured vacuum present in the tube. Why Does It Matter!?!?!? • The order in which the tubes are drawn is one of the MOST IMPORTANT considerations when collecting blood specimens. • Tubes MUST be collected in a specific order to prevent invalid test results caused by contamination of the specimen by microorganisms, tissue thromboplastin, or carryover of additives or anticoagulants between tubes. • The order of draw changes when collecting a capillary specimen due to how quickly the blood can clot. In order to achieve maximum quality for a specimen the microtainer tubes need to be collected purple then green. Most Common Tubes Drawn Color of Tube Main Tests Run Serum/Plasma Blood Cultures Microbiology Red Send out serum No Clot activator No gel Blue Coagulation plasma Sodium Citrate Gold chemistry serum Clot activator Green chemistry plasma Lithium heparin Pink Blood bank plasma K2 EDTA Purple hematology plasma K2 EDTA Gray chemistry plasma PotassiumOxalate/ Sodium Fluoride NA Anticoagulant medium ADDITIVES Gels are found in green and gold top evacuated and microtainer tubes. Most commonly used for separating Plasma and serum from the red blood cells. SODIUM CITRATE BINDS CALCIUM MOST COMMONLY USED FOR COAGULATION STUDIES GOLD CLOT ACTIVATORS – INITIATES OR ENHANCES COAGULATION LITHIUM HEPARIN INHIBITS THROMBIN MOST COMMONLY USED FOR CHEMISTRY DETERMINATIONS K2 EDTA (ETHYLENEDIAMINETETRAACETIC ACID) BINDS CALCIUM MOST COMMONLY USED FOR HEMATOLOGY STUDIES POTASSIUM OXALATE/ SODIUM FLUORIDE BINDS GLUCOSE OFTEN USED FOR GLUCOSE TESTING Special Requirements • • • • • Drug Levels – Usually ordered as a timed study (should be treated as a STAT) and required to be drawn as close to the time requested as possible due to the peak and trough levels of medication that has been given to the patient. Cold Agglutinins – Because cold agglutinins in serum attach to the RBC’s when the blood cools below body temperature, the specimen must be kept warm until the serum can be separated from the cells. Specimens Sensitive to Light – Exposure to light will decrease the concentration of bilirubin, beta-carotene, folate, vitamins A, B12, and B6 and Porphyrins. Chilled Specimens – Specimens for tests such as lactic acid and ammonia as well as many others need to be placed on ice (chilled) immediately after collection to prevent deterioration. Cortisol Stimulation – These tests are ordered by Chemistry after the nurse has dosed the patient. These tests MUST be done on time with NO EXCEPTIONS. If a patient receiving cortisol is not drawn on time the patient must wait 3 days before being able to repeat the test. Appearances of Blood • Normal serum and plasma appear clear and pale yellow. • Variations in the normal appearance can indicate that certain tests results may be adversely affected. (ex. results can be severely decreased or increased.) • Hemolyzed – Pink to red color, indicating red blood cell destruction • Icteric – Dark yellow color indicating the presence of increased bilirubin • Lipemic – Cloudy, milky appearance indicating the presence of increased lipids. Hemolysis Hemolysis – is the breakage of red blood cell’s membrane, causing the release of the hemoglobin and other internal components into the surrounding fluid. Which can be caused by a variety of factors including but not limited to: • • • • • • • • • • Rapidly pulling back on the plunger of a syringe Forcing blood from syringe into tubes Capillary draws that are not free flowing Improper choice in venipuncture site Prolonged tourniquet time Cleansing the venipuncture site with alcohol and not allowing the site to dry Improper venipuncture indicated by slow blood flow The use of a small bore needle resulting in a large vacuum force applied to the blood, causing stress on the red blood cells which may cause them to rupture Vigorous mixing or shaking of a specimen Prolonged contact of serum or plasma with cells Test results from all laboratory disciplines can be affected by hemolysis. The only corrective action is to………………… Must invert tubes 8-10 times: • to prevent hemolysis • to ensure adequate mixing of blood with anticoagulant Tests Affected By Hemolysis • • • • • • • • • • • • • • • • • Acetone Alcohol Ammonia AST C-Peptide CK CEA Cortisol Direct Bilirubin Free T4 Folate FSH Glucose Iron Lactic Acid LDH LH • • • • • • • • • • • • • • • • • Lipase Magnesium Phosphorus POTASSIUM Protein Electrophoresis PSA Testosterone Total Protein Total T4 TSH Vitamin B12 D-Dimer ESR Fibrinogen Hemoglobin Hematocrit PT PTT Redraw The Specimen Which Way do I Collect the Blood?? • Venipuncture can be performed using an evacuated tube system, a syringe system, or a winged blood collection (butterfly) set. Each of these systems requires its own unique equipment. • The system that is chosen for venipuncture is ALWAYS based on the assessment of the patient’s veins. NOTE: Each and every person has different veins (ex. Shape, size, and stability) VENIPUNCTURE EQUIPMENT • Differentiate between evacuated tube, syringe, winged blood collection set for collection of blood by venipuncture. • Differentiate various needle sizes, length, guage and purpose. • Safely disposing of contaminated needles. • Identify types of evacuated tubes by color, types of anticoagulants, additives present, mechanism of action, special characteristics, and purpose of each. • List correct order of draw for various types of blood collection tubes. • Purpose of tourniquet • Substances used to clean skin prior to venipuncture. • Quality Control of Venipunture. Evacuated Tube System (Vacutainer) • The evacuated tube system is the most frequently used method for performing venipuncture. • Blood is collected directly into the evacuated tube. • This system allows for the collection of numerous tubes from a single venipunture. • This system is usually chosen when a patient has a large median cubital vein, or other large veins in the antecubital area that are easily palpated. (15 to 30 degree angle) SYRINGES • Syringes – may be preferred over an evacuated tube system at times when drawing blood from patients with poorly anchored, rolling veins that will NOT support a vacuum. (10 to 15 degree angle) • The advantage of this system is that the amount of suction pressure on the vein can be controlled by slowly pulling back on the syringe plunger. NOTE: blood drawn in a syringe must be immediately transferred to appropriate evacuated tubes to prevent the formation of clots. WINGED BLOOD COLLECTION SETS (BUTTERFLY) • WINGED BLOOD COLLECTION SETS – or butterflies as they are routinely called are used for: • Performing venipuncture from very small veins (10-15 degree angle) • Obtaining specimens from children and elderly. WHAT SIZE NEEDLE WOULD YOU USE? • Needle sizes are determined by the number on the package. The BIGGER the number the SMALLER the (gauge) needle. • Therefore the SMALLER the number the BIGGER the (gauge) needle. Ex: 23’ gauge 22’ gauge 21’ gauge Where Are the Veins? • Proper positioning is important for succesful Venipuncture. Patients should not stand or sit on High stools because of possiblity of fainting • Slight rotation of the patient’s arm is necessary or vein exposure. • As a rule of thumb, the tourniquet should not be left On the patient for more than 1 minute at a time Because of discomfort, However the tourniquet is left on During the blood draw. • Tourniquets – are used to allow the veins to fill to Capacity Hand Veins & Nerve Damage • The Posterior surface of the wrist Should be used for hand venipunctures. • The hand is full of nerves and the venous Network. EXTREME caution needs to be used when selecting a vein in the hand or wrist for venipuncture. • Nerve Damage can also occur with Excessive needle punctures. • Never draw blood from a FOOT!!!!!! PERIOD!!!! Capillary Specimens • Capillary specimens are to be drawn only when necessary. • When a patient has no discernable veins in hands or arm and you need a CBC. • Always be sure that the test required can be done from a capillary specimen before drawing the patient if there is no other way to obtain the specimen. Phlebotomy Tips • Bevel on Upper Wall – rotate bevel slightly • Needle slipped beside vein – withdraw needle until The bevel is just under the skin and redirect needle into Vein. • Needle Position cannot be determined – withdraw Needle until bevel is just under the skin, relocate vein, and redirect into vein. • Needle too deep and penetrated through vein – Withdraw needle slightly • Needle Not Deep Enough – push needle gently into vein • Collapsed Vein – Vein disappears when entered due to vacuum, or pressure caused by pulling on syringe plunger. (try again using smaller tube Or pull more slowly on syringe plunger.) NOTE: If unable to obtain specimen discontinue Phlebotomy and try again using appropriate actions. Is it Venous, capillary or arterial? • VENOUS blood is the specimen of choice for clinical laboratory testing. • ARTERIAL blood is the required specimen for arterial blood gas determinations. • CAPILLARY blood is a mixture of arterial and venous blood and is • collected by dermal puncture. (ex. fingerstick, heelstick) When properly collected capillary blood is suitable for some lab tests Therefore it should always be indicated on the label whether a specimen is venous or capillary. This information must accompany the results for interpretation by the physician. QUALITY ASSURANCE • As you can see many factors related to blood collection can affect laboratory Quality Assurance. Remember that Laboratory Personnel are available to answer questions and should be consulted whenever NEEDED. Pre-analytical Errors https://www.youtube.com/watch?v=Ph4H1AuvOH0 Blood Culture Collection • Watch blood collection video QUESTIONS?????