Low-Risk - The Prostate Net
advertisement

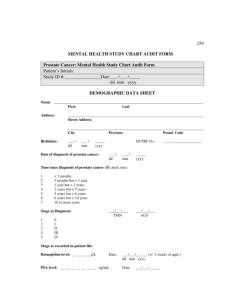
Newly-Diagnosed Prostate Cancer Mark Scholz MD Prostate Oncology Specialists The PSA Net Types of Things We Find in the PSA Net • BPH • Recent sexual activity • Lab errors • Prostate infections • High-Grade prostate cancer • Low-Grade prostate cancer 260 240 220 PSA Testing Started 1987 200 180 Prostate 160 140 120 100 80 60 Lung and Bronchus Colon and Rectum 40 Urinary Bladder Non-Hodgkin Lymphoma Melanoma of the Skin Year of Diagnosis Adapted from Jemal A, et al. CA Cancer J Clin. 2006;56:106-130. 2001 1999 1995 1997 1993 1989 1991 1987 1983 1985 1981 1979 0 1975 1977 20 2002 Rate per 100,000 Population Annual Age-Adjusted Cancer Incidence Rates Among Males for Selected Cancers, 1975-2002 Epidemic Prostate “Cancer” • Prior to PSA (1987) 1 of 41 men died of PC (2.4%) • In 2009, with screening and early treatment, the • risk of dying from PC is 1 of 53 (1.9%) However: – 200,000 diagnosed annually instead of 90,000 – 1.5 million men are biopsied annually – The lifetime risk of biopsy is 1 out of 2 “Six-Core” Biopsy of 3000 Men Age 55-75 with Normal PSA PSA Level Cancer Diagnosis Rate 1 – 2 17% 2 – 3 24% 3 – 4 27% radical prostatectomy specimen transition zone prostate cancer urethra peripheral zone Prostate Biopsy Points of needle entry Posterior View Prostate Tests to Detect Prostate Cancer –PSA blood test –PCA-3 urine test –Digital rectal examination –Ultrasound and MRI scans “Risk of Biopsy-Detectable Prostate Cancer” • • • • • • Age BMI (are you fat?) Race PSA Rectal exam PCA-3 55 22.5 Not African American 2.0 Risk of any prostate normal Cancer = 23% not done Risk of High-Grade prostate cancer = 2.5% Prostate Cancer Types • Growth rate • Ability to spread “Gleason” Grading of Prostate Cancer • Low grade (3) • Higher Grade (4) • Highest Grade (5) • Score = “Adding Up” two grades Staging Risk Gleason PSA Digital Low (all) <7 < 10 Normal 7 10-20 Nodule >7 > 20 Mass Intermediate (any) High (any) Risk Status • Low = Monitor • Intermediate = Seeds, Surgery or IMRT • High-Risk = IMRT with Hormone Blockade Treatment Selection Flow Chart Low-Risk Determine Disease Risk Intermediate High-Risk Active Surveillance Seeds or IMRT or Cryotherapy or Surgery or Hormones or Active Surveillance or IMRT plus Short-Term Hormones Long-Term Hormones plus IMRT plus Seeds 10-Year Survival by Risk Category Low More than 100% Brenner: Journal of Clinical Oncology 2005 Intermediate With treatment 98% Mayo Clinic Journal of Urology 2008 High Surgery 95% Mayo Clinic Journal of Urology 2008 Very High Early Hormone blockade: 87% Late Hormone blockade: 59% Messing: New England Journal Medicine 1999 Prostate Snatchers The Prostate is “Built In” Collateral Damage Loss of Sexual and Urinary Function Impotence Five Years after Surgery: 1288 Men David Penson Journal of Urology 2005 • Incapable of an erection adequate for intercourse with Viagra Age < 54 55-59 60-64 > 65 39% 51% 56% 82% Urinary Continence Surgeon 12 mo Pat Walsh (Open) 93% Ahlering (Robotic) 94% Shalhav (Robotic) 84% Lee (Robotic) 90% “Optimal Surgical Competency Requires a minimum of 250 Practice Cases” • In the New York during the whole of the years in 2005: – 25% of the urologists did a single radical prostectomy – 80% of the urologists did <10 cases Savage & Vickers, Memorial Sloan Kettering Journal of Urology December 2009 Radiation Implant Procedure Implant Procedure X-Ray of Seed Implant Robotic Prostatectomy Computer enhanced Surgeon operates at the console within a 3D view Bedside surgical assistant is next to the patient Instruments move like a human wrist (↑ dexterity and precision) The Surgeon Directs The Instruments The surgeon’s hands are placed in special devices that direct the instrument movement Robotic Prostatectomy: Difference Big, Ugly Scar Standard Surgery little, tiny scars Robotic Surgery Robotic vs. Standard Prostatectomy in 2700 Patients • Good: – Shorter hospital stays (1.4 vs. 4.4 days) – Slightly less complications (30 vs. 36%) • Not so Good: – Higher likelihood of needing salvage radiation therapy (28 vs 9%) – More urethral strictures (40% more likely) Hu, Jim et al. Journal of Clinical Oncology, May 2008 Cure Rates: Surgery vs. Seeds • 15,000 studies reviewed • Expert panel determined inclusion criteria • 603 studies met criteria Criteria for the Study Inclusion 1. Patients divided into low, intermediate & high-risk groups 2. Standardized PSA endpoints such as ASTRO, Phoenix, and PSA < 0.2 (surgery) Intermediate Risk: Percentage Progression Free % Progression Free 1 1540 0.9 Brachy 24 8 23 2 22 17 0.8 12 0.7 4 40 3612 32 34 0.6 16 31 43 37 Surgery 8 0.5 0.4 1 2 3 4 5 6 7 Years 8 9 10 11 12 13 14 15 Brachy Surg Side Effects Comparison of: Surgery, Brachytherapy and Beam Radiation Talcott, Journal of Clinical Oncology, 2003 Quality of Life • Prospective study at MGH and Harvard • Questionnaire prior, 3, 12, 24, 36 mo. post Rx. • 522 pts treated with, IMRT, Surgery or • Average age: Surgery patients younger than Brachytherapy patients, who were younger than IMRT patients Urinary Obstruction/Irritation (Higher score = worse function) 30 25 20 RP 15 Brachy 10 5 0 0 mo 3 mo 12 mo 24 mo Incontinence (Higher score = worse function) 30 25 20 Brachy 15 RP Nerve Spare 10 5 0 0 mo 3 mo 12 mo 24 mo Bowel Problems (Higher score = worse function) 9 8 7 6 5 RP 4 Brachy 3 2 1 0 0 mo 3 mo 12 mo 24 mo Sexual Dysfunction (Higher score = worse function) 90 80 70 60 50 RP 40 Brachy 30 20 10 0 0 mo 3 mo 12 mo 24 mo Health Related Quality Of Life Validated Instrument Studies • ~ 4230 patients in 7 studies comparing surgery, IMRT and brachytherapy: • Davis JW, et al. J Urol. 2001;166:947-952 • Wei JT, et al. J Clin Oncol. 2002;20:557-566 • Lee WR, et al. IJROBP. 2001;51:614-623 • Talcott JA et al. JCO 2003; 21(21): 3979 • Miller DC et al. JCO 2005; 23 (12):2772 • Frank SJ et al. J Urol 2007; 177: 2151 • Sanda MG et al. NEJM 2008; 358(12):1250 Summary Treatment Side Effects of the Seven Studies • Seed implants result in: – less incontinence than surgery – more urinary symptoms like urgency or frequency – Better potency than surgery Risks for Men with Low-Risk Prostate Cancer • Unskillful or unnecessary therapy • Inaccurate staging “Either this is the wrong chart or —lets just hope this is the wrong chart” 77777777 777777777 777 “Because of your age, I’m going to recommend doing nothing.” Active Surveillance = Watchful Waiting Active Surveillance Watchful Waiting Aim Individualize therapy Avoid treatment Age Any Older or sicker Monitoring Aggressive Lax Treatment timing Early Late Indications for treatment PSA increase, changes on ultrasound or biopsy Cancer symptoms such as bone pain Treatment intent Cure Symptom control Surgery Vs. “Watching” Bill-Axelson, New England Journal Medicine • Randomized prospective trial 695 men • Mean PSA 12.8 • 75% stage B (palpable nodule) • 25% Gleason 7 (6% with Gleason >8) • Cancer detected by DRE, not PSA Bill-Axelson: 10-Year Results Surgery “Watching” Cancer Survival 90% 85% Risk Reduction 5% Benefit of Surgery Compared to Doing Nothing at All • Intermediate risk or High Risk disease • “Watching” not Active Surveillance • No early treatment for a rising PSA = 20 men operated to save 1 life 10 years later Projected Outcome in Low-Risk Disease on Active Surveillance Journal of Clinical Oncology 2005 • Grade 6 • Rectal exam normal • PSA < 10 • Cancer in <1/3 of cores • Early treatment = 100 men Operated to Save 1 Life 10 Years in the Future Active Surveillance Delaying curative therapy until evidence of cancer growth at which time curative treatment is administered Active Surveillance in 450 Men with Low to Intermediate Risk Disease Klotz—Journal of Clinical Oncology 2010 • Surveillance – PSA and DRE every 3 months – Biopsy every 2-4 years • Progression – Increase in Gleason score – PSA doubling in less than 3 years – New or enlarging nodule on rectal examination Results Ten Years • Patients: – Average age 70 – 71% “Low Risk” • 83% Gleason 3+3, 17% Gleason 3+4 • 85% PSA < 10, 12% PSA 10-15 • 10-year overall survival was 68% – 97 died of causes besides prostate cancer – 5 died of prostate cancer Enhancement of Active Surveillance • • • • Biopsy showing < 1/3 cores positive Color doppler ultrasound every 6 months Multi-Phasic MRI annually Proscar or Avodart Color Doppler Ultrasound • Identifies lesions for monitoring • Measures tumor progression Color Doppler Image Six Months Earlier 3-Tesla Prostate MRI Anatomy Chemical concentrations Cellular density Blood flow Proscar and Avodart Advantages • Inhibit cancer • Improve PSA • • • accuracy Increase biopsy accuracy Improve urination Grow hair Side Effects • Lower libido • Breast growth Conclusions: Active Surveillance • Aggressive, hurried prostate cancer treatment benefits very, very few men • The window of opportunity to defeat early-stage disease is measured in years, not months • Active surveillance rather than immediate radical treatment allows men with low-risk disease to avoid the side effects of treatment for many years if not indefinitely.