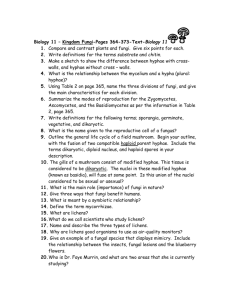
Characteristics of Fungi
advertisement

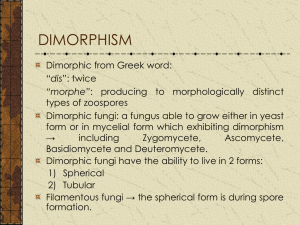
Characteristics of Fungi Non-motile eukaryotes lacking chlorophyll – Contain nucleus, mitochondria, 80S ribosomes – Cell wall is composed of polysaccharides , polypeptides and chitin and the cell membrane contains sterol which prevent many antibacterial antibiotics being effective against fungi. – Larger than bacteria – Relatively simple nutritional requirements, wide range of growth rates • Form visible colonies in days to weeks Unicellular or multicellular depending on the species Fungi can be divided into: Yeast, Mould (filamentous fungi) and Dimporphic fungi 1 Molds Multicellular, tubular structures (hyphae) Hyphae can be septate (regular crosswalls) or nonseptate (coenocytic) depending on the species (grow by apical extension) – Vegetative hyphae grow on or in media (absorb nutrients); form seen in tissue, few distinguishing features – Aerial hyphae contain structures for production of spores (asexual propagules); usually only seen in culture 2 Molds - identification Identification based on colony morphology (pigment, texture) and morphology of reproductive structures – Conidia - spores formed by budding (blastoconidia) or disarticulation of existing hypha (arthroconidia) – Sporangiospores - produced by free-cell formation within sporangium in nonseptate molds 1 1. 2. 3. 4. 5. Conidiopspores Phialides Vesicle Conidiophore Septate hyphae 1 3 2 3 4 2 5 5 1. 2. 3. 4. sporangium sporangiophore Endospores Nonseptate hyphae 5. rhizoids 4 3 Colonial Morphology of Fungi Cryptococcus Trichophyton Wangiella neoformans tonsurans dermatitidis Candida T. mentaAspergillus albicans grophytes fumigatus 4 Yeasts Unicellular, 3-5 µm, reproduce by budding (blastoconidia formation) or fission Identified by microscopic morphology (grow on cornmeal agar) and biochemical tests (sugar assimilation, enzymatic activity). Molds and yeast are not exclusive forms, some species may exist in both yeast and mold forms (dimorphism). 5 Classification of Fungi Taxonomy is based on structural features of the teleomorph (sexual phase). – Zygomycota - includes all fungi with nonseptate hyphae – Ascomycota - includes most human pathogens – Basidiomycota - mainly plant pathogens – Deuteromycota (fungi imperfecti) 6 Isolation of fungi Direct examination:Wet specimen preparations – e.g. Aspergillus hyphae in sputum or Cryptococcus neoformans in CSF (mixed with india ink) – Potassium hydroxide (KOH) cleared specimens , e.g. dermatophyes (ringworm fungi) in skin scrapings, nails or hair – Stained preparation: e.g. Candida albicans in Gram stained smears of vaginal discharge or pneumocystis carinii in Giemsa or other stained preparations of bronchoalveolar lavage or sputum. 7 Isolation of fungi Culture Media – General purpose media • BHI + blood, inhibitory mold agar • Sabouraud dextrose agar – Mycosel • Sabouraud + chloramphenicol and cycloheximide • For isolation of dermatophytes (some pathogenic fungi are inhibited by cycloheximide) Incubation – 30°C for 30 days 8 Medically important fungi Molds • • • • • Dermatophyte Fungi causing mycetoma داء القدم الفطري Fungi causing chromomycosis فطر ملون Aspergillus species Zygomycetes: Mucor عفن فطري Yeast • Candida albicans • Cryptococcus neoformans • Malassezia furfur Dimorphic • • • • Histoplasma species Blastomyces dermatitidis Paracoccidioides brasiliensis Coccidioides immitis 9 Fungal Infections Fungi generally have low pathogenic potential – Only a few true pathogens; many opportunists – Most are acquired from exog/environ sources – Pathology caused by tissue invasion and/or host inflammatory response. Many fungal infections can be characterized by extent of invasion Type of infection superficial cutaneous subcutaneous deep/systemic opportunistic Example Malasezzia furfur dermatophytes sporotrichosis histoplasmosis candidiasis 10 Dermatophytes Fungi that cause superficial/cutaneous infections – Confined to keratinized tissue (hair, skin, nails) – Cause of ringworm (eg tinea capitis, tinea pedis); inflammation greatest at advancing edge. – All are molds. Many species produce macroconidia • Epidermophyton (2 spp), Microsporum (16 spp), Trichophyton (24 spp) – Transmitted indirectly via desquamated skin and hair (combs االمشاطhats قبعه, showers, etc). Diagnosis based on direct exam of scrapings, culture on selective media. M. canis 11 Subcutaneous Mycoses Caused by direct inoculation of organisms from soil or decaying plants – Generally cause localized infection – Hands and feet are most common sites Sporotrichosis داء الشعيرات المبوغة – Caused by dimorphic fungus Sporothrix schenkii • Mold in environment, yeast in infected tissue – Commonly affects hands trauma from thorns (شوكهeg rose gardens); causes lympho-cutaneous infection • Extracutaneous (pulmonary) and disseminated disease uncommon 12 Subcutaneous Mycoses (continued) Chromoblastomycosisالفطر البرعمي الملون – Slow, progressive, granulomatous infection. – Skin lesions contain dark brown sclerotic bodies. – Caused by dematiaceous (black) molds, eg Cladosporium, Phialophora. Mycetoma – Swollen lesion, granules (containing organisms) draining from sinuses. – Can be caused by fungi eg Pseudoallescheria or actinomycetes (prokaryotes) 13 Candidiasis Genus Candida - diverse group of yeasts – Budding yeast, stain Gram-positive – ID based on biochemical tests and morphology (corn meal agar) C. albicans - most important pathogen – Multiple forms: budding yeast, pseudohyphae, true hyphae. Forms germ tubes (in presence of serum). 14 Pathogenesis of Candida infections Most infections are endogenous – Candida is component of normal oral, GI, vaginal flora Pathogenic factors – Essential role of mucosal adherence – Alterations in micro-environment and/or microbial flora predispose to symptomatic infection. – Germ tube formation, proteinases, phospholipases may contribute to local invasion by C. albicans 15 Candida infections Cutaneous infections - nails, diaper rash, Mucosal infections – thrush (tongue, oral mucosa), pseudo-membrane; seen with inhaled steroids, cancer, HIV – esophagitis in suppressed pts (mucosal invasion) – vulvovaginitis (discharge containing epithelial cells, pseudohyphae, hyphae) 16 Candida infections Candidemia/disseminated candidiasis – Candida spp are 4th leading cause of nosocomial bloodstream infections – Antibiotics, iv catheters increase risk • Antibiotics eliminate normal GI flora, permit overgrowth of Candida and entry across damaged mucosa • IVs provide entry through skin – Dissemination to kidney, brain, myocardium, eye is common. • Ocular candidiasis - white cotton ball-like lesions of retina; can cause blindness 17 Candida infections (continued) Urinary tract candidiasis – Usually seen in pts with urinary catheter. Hepatosplenic candidiasis – Occurs in severely compromised (neutropenic) pts. Multifocal abscesses 18 Candidiasis - Diagnosis Direct microscopic examination – Important to demonstrate tissue invasion in mucosal infection; positive culture alone may be due to colonization Culture – Candida spp grow well on standard media. – Candidemia readily detected with commercial blood culture systems. 19 Cryptococcus neoformans Encapsulated yeast – Identification based on presence of capsule, urease, growth at 37°C, melanin synthesis, and sugar assimilation. Major virulence factors – Polysaccharide capsule • Antiphagocytic • Immunosuppressive – Melanin synthesis 20 C. neoformans - Clinical features Acquired by inhalation – Most infections are asymptomatic. May present as isolated pulmonary nodule (r/o carcinoma) Cryptococcal meningitis – Dissemination from lung. Life-threatening – Major opportunistic infection in HIV pts with low CD4 counts 21 Cryptococcocal meningitis Diagnosis – CSF WBC count may not be elevated • Poor prognostic sign – Direct detection of capsular antigen in CSF • Latex agglutination or EIA • High sensitivity and specificity; has displaced India ink (lacks sensitivity) – Culture - gold standard Treatment – Amphotericin B + 5-fluorocytosine – In HIV patients, C. neoformans cannot be eradicated, requires suppressive therapy. 22 Histoplasma capsulatum - Dimorphism Filamentous mold in environment – Thin septate hyphae, microconidia, and tuberculate macroconidia (8-14 µm) Budding yeast (2-4 µm) in tissue – Dimorphic transition is thermally dependent and reversible (25°C 37°C). Hyphae, micro- and macroconidia Yeast within histiocyte 23 H. capsulatum - Epidemiology – H. capsulatum can be cultured from soil in endemic areas. Abundant growth in soil containing bird feces (starling roosts, chicken houses) or bat guano (caves). 24 H. capsulatum - Pathogenesis Conidia or hyphal fragments are inhaled, ingested by macrophages. Organisms convert to yeast phase, proliferate in nonimmune macrophages, and spread through RES. Dissemination is common and occurs early, but is usually asymptomatic. CMI response results in macrophage activation, increased fungicidal activity. Infection is contained but not necessarily eradicated. 25 Histoplasmosis - Self-limited Syndromes Acute pulmonary histoplasmosis accounts for most cases of symptomatic infection – Fever, chills, headache, myalgia, anorexia, nonproductive cough, pleuritic chest pain. – Enlarged lymph nodes, patchy infiltrates. – Patients usually improve in several weeks. 5-10% symptomatic cases develop inflammatory syndromes (arthritis, erythema nodosum, or pericarditis) 26 Chronic pulmonary histoplasmosis Slowly progressive pulmonary disease. Usually associated with preexisting lung disease. – Cough, dyspnea, chest pain, fatigue, fever, night sweats, and weight loss Usually progresses if untreated – AmB or itraconazole (depending on disease severity) reduces symptoms, improves radiographic findings, eliminates H. capsulatum from sputum 27 H. capsulatum - Culture Histoplasma produces mycelial growth with characteristic warty مثل الثألولconidia when cultured at room temperature. Small microconidia and characteristic large , round , spiny macroconidia are produced. At 37 C on certain media it is possible to induce the yeast phase of this dimorphic fungus – Sputum best for pulmonary histoplasmosis – Bone marrow or blood best for disseminated histoplasmosis 28 H. capsulatum – Direct examination Examination of infected tissue (eg bone marrow, liver, skin, GI mucosa) can provide rapid presumptive evidence of disseminated histoplasmosis Intracellular yeasts can be seen on peripheral smears in severe disseminated disease NEJM 342:28 29 C. immitis - Dimorphism Grows as hyphae in environment. Forms thickwalled arthroconidia alternating with thin-walled cells. Spherule كريةfilled with endospores in infected tissue. 30 C. immitis - Pathogenesis Arthroconidia are inhaled and convert to spherules that grow to 20-150 µm. Partially resistant to killing by phagocytic cells. Spherules undergo multiple nuclear divisions and segmentation of cytoplasm to produce hundreds of endospores (2-5 µm). The spherule ruptures, releasing endospores that form new spherules. 31 C. immitis - Epidemiology Can be cultured from soil in areas where disease is endemic. Expected number of infections is 100,000 annually 32 C. immitis - Respiratory Infections 40% of pulmonary infections are symptomatic – Most are self-limited – Fatigue, cough, chest pain. May also have fever, dyspnea, myalgia, and headache Pulmonary nodules – 4% of infections give rise to solitary وحيدةnodule ( 5 cm) – Can form cavities, infreq rupture into pleural space 33 C. immitis - Disseminated infections Occurs in ~ 0.5% of infections. Increased risk: – HIV, organ transplants, steroids, Hodgkin’s Skin is most common site of dissemination Joints and Bones – Prominent synovitis, effusion; knee most common – Vertebrae (multiple) > long bones – culture (50%) and histopathology for diagnosis Meningitis – Headache, vomiting, alt mental status. WBC (mono), prot, gluc in CSF. Culture usually neg. 34 C. immitis - Culture and Histopathology Culture - white fluffy وبريmold at 25-30ºC. – Arthrospores are suggestive but not diagnostic Histopathology – Acute inflammation (PMNs and Eos) assoc with active infection and ruptured spherules – Granulomas assoc with chronic infection, unruptured spherules 35 Blastomyces dermatitidis Microbiology – Hyphae with microconidia at room temp – Convert to broad-based budding yeast at 37ºC. pulmonary infection (asymptomatic or pneumonia); chronic pulmonary disease common Disseminated disease: skin (common) and bones 36 B. dermatitidis - Diagnosis Culture – White light tan mold at room temp, not diagnostic – Identification based on conversion to yeast at 37ºC, Histopathology – Thick walled broad based budding yeast – suppurative and/or granulomatous inflammation 37 Paracoccidiodes brasiliensis Microbiology – Hyphae at room temp. – Converts to yeast with multiple buds at 37ºC. – Probably acquired by inhalation. Pulmonary infection can be asymptomatic, acute, or chronic – Extrapulmonary disease in adults > 30 usually involves oropharyngeal mucosa and regional lymph nodes. 38 Penicillium marneffei Only dimorphic species in genus Penicillium • Infection probably occurs through inhalation • Chronic illness, low-grade fever, wt loss, skin lesions, disseminated infection – Intracellular forms resemble H. capsulatum; extracellular forms exhibit septa (cells divide by fission, not budding) – Grows as mold at 25-30ºC • Produces soluble red pigment • Converts to yeast phase at 37ºC 39 Aspergillus spp. More than 100 species of Aspergillus. Septate hyphae branching at 45 angle. Omnipresent موجودة بكل مكانin environment. A. fumigatus is thermotolerant (up to 55oC) and is found in high concentrations in compost اوراق الشجرsites. Most human disease caused by A. fumigatus, A. flavus, and A. niger. Opportunistic pathogen, airborne spread 40 Aspergillus Infections Allergic bronchopulmonary aspergillosis Aspergilloma (fungus ball) – Colonization of preexisting lung cavity (TB, abscess, etc(. Invasive pulmonary aspergillosis – Occurs in pts with immunosuppression and neutropenia. – Vascular invasion, infarction, cavitation – Hematogenous dissemination common (ocular, cerebral, cutaneous involvement) 41 Aspergillosis - Diagnosis Direct examination – Difficult to distinguish branching septate hyphae of Aspergillus spp from other opportunistic fungi, eg Pseudallescheria, Fusarium. Culture – Aspergillus spp grow well on standard media. Airborne contaminants are a problem. – Need to see several colonies from one specimen or same organism in multiple specimens. 42 Mucormycosis Infections caused by Mucoraceae – Mucor, Rhizopus, Absidia – Broad nonseptate hyphae, sporangia. • Widespread in environment; found in decaying vegetables and fruits, soil, old bread; grow and sporulate on materials containing carbohydrates. R. oryzae is most common clinical isolate. 43 Mucormycosis - Clinical features Rhinocerebral/craniofacial mucormycosis – Infection of paranasal sinuses with extension from ethmoid into orbit or frontal lobe (also cavernous sinus thrombosis). – Prompt diagnosis essential; direct exam of turbinate scrapings and/or sinus aspirate. Pneumonia – Resembles invasive pulmonary aspergillosis Cutaneous infection – Associated with localized trauma – Cellulitis with central necrotic area. 44 Antifungal Drugs Polyenes (Amphotericin B, nystatin) Azoles (fluconazole, itraconazole) Echinocandins (caspofungin) 5-Fluorocytosine 45