Dermatologic Problems / Integumentary System
advertisement

Dermatologic Problems/
Integumentary System
Physical Examination
Obtain history
WHATS UP
Inspection
Palpation
Gloves are worn during examination
Physical Examination
Observe for:
Color
Temperature
Moisture
Dryness
Physical Examination
Skin texture (rough-smooth)
Lesions
Vascularity
Mobility
Texture of hair and nails
Skin turgor
Physical Examination
Color
Varies from person to person
Ivory-deep brown
Pigmentations r/t
Sun exposure
Fevers
Sunburn, inflammationPink or
Reddish hue
Pallor
Decreased skin tones
Physical Examination
Color
Vascularity
Observed in
Bluish hue
Conjunctivae
Mucous membranes
Cyanosis = cellular hypoxia
Jaundice
Yellow pigment
sclera
mucous membrane
Physical Examination
Color
Dark skinned persons
Have reddish base and undertones
Buccal mucosa, tongue, lips,nails normally appear
pink
Cyanosis-skin assumes grayish cast
Age related changes
Physical Examination
Types of dressings
Wet-dry dressings
Moisture-retentive dressings
Already impregnated with moisture
Occlusive dressings
Cover wound
Physical Examination
Topical medications
Lotions, suspensions
Clear solutions, liniment,
Powders, creams,
Gels, pastes,
Ointments, sprays,
Corticosteroids etc.
Wounds
Abrasion – skin is rubbed or scraped
off
Lacerations – torn, ragged, irregular
edges made by blunt objects
Avulsions – the tearing away of tissue
from a body part
Incisions – cuts made by sharp cutting
instruments
Punctures – caused by objects that
penetrate tissue while leaving a small
surface opening
Amputations – traumatic is the
nonsurgical removal of a limb from the
body
Wound Healing
1st intention
2nd intention
3rd intention
Diagnostic Tests/Treatments
Cultures
Skin biopsy
Wood’s light examination
Skin testing (allergies)
Open wet dressing/other dressings
Therapeutic baths
Topical meds
Herpes Zoster {Shingles}
Acute inflammatory and infectious
disorder
Painful vesicular eruption
Bright red edematous plaques along the
nerve from one or more posterior ganglia
Herpes Zoster {Shingles}
cont’d
Eruption follows the course of the nerve
Almost always unilateral
Herpes Zoster {Shingles}
Cause
Varicella-zoster virus (like chicken-pox)
Incubation period 7-21 days
Vesicles appear in 3-4 days
Occur posteriorly
Progress anteriorly & peripherally
Along dermatome
Duration 10 days to 5 weeks
cont’d
Herpes Zoster {Shingles}
cont’d
Occurs most frequently in
Elderly
Immunosuppressed
Malignancy or injury to spinal or cranial nerve
Herpes Zoster {Shingles}
Complications
Facial and acoustic nerve involvement
Hearing loss
Tinnitus
Facial paralysis
Vertigo
painful
cont’d
Herpes Zoster {Shingles}
cont’d
Complications
Full thickness skin necrosis and scarring
Systematic infection from scratching, causing
virus to enter blood stream
Herpes Zoster {Shingles}
Medical treatment
Control outbreak
Reduce pain and discomfort
Prevent complications
Acyclovir (Zovirax) IV, PO, topically
Corticosteroids
Antihistamines
Antibiotics
cont’d
Herpes Zoster {Shingles}
cont’d
Nursing Care
Cool compresses two-three times per day
Help cleanse and dry lesions
Measures to decrease itching
Medication
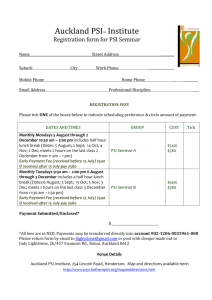
Parasitic Skin Infections (PSI)
Higher risk situations?
Poor hygiene
Living in close quarters
Pediculosis- Lice (PSI)
Infestation by human lice
Pediculosis capitis-head
Pediculosis corporis-body
Pediculosis pubis- pubic or crab
Pediculosis (PSI)
Parasite
Approximately 2-4 mm
Female lays eggs-hundreds-nits
Deposit on hair shaft base
Pediculosis (PSI)
Symptoms
Pruritus
Excoriation
Vectors of other diseases
Typhus
Recurrent fever
Pediculosis Capitis (PSI)
More common in women
Sides and back of scalp
Assess for
Visible white flecks (nits)
Matting and crusting of scalp
Foul odor
Pediculosis Capitis (PSI)
Treatment
Pediculicides
Hand pick or comb nits out
Launder bed linens & vacuum
Seal items in plastic bags for 14 days
Repeat above in 10-14 days
Pediculosis Corporis (PSI)
Lice live and lay eggs in clothing
Itching
Assess for
Excoriation on
Trunks
Abdomen
Extremities
Pediculosis Pubis (PSI)
Intense pruritis
Vulvar region
Peri-rectal
More compact
Crab-like appearance
Pediculosis Pubis (PSI)
Contracted from
Infested bed linens
Sexual intercourse
May also infest
Axilla
Eyelashes
Chest
Pediculosis (PSI)
Treatment
Chemical killing
Clean linens with hot water and soap
Dry-clean
Fine-tooth comb
Treat social contacts
Scabies (PSI)
Contagious skin disease
Mite infestation
Transmitted by
Close-prolonged contact with
Infested companion
Infested bedding
Scabies (PSI)
Characterized by
Epidermal curved or linear ridges
Follicular papules
Pruritus Palms
More intense and unbearable at night
White visible epidermal ridges by
Mite burrowing into outer layers of skin
Scabies (PSI)
Hypersensitivity reaction
Excoriated erythematous papules
Pustules, crusted lesions
Elbows
Axillary folds
Lower abdomen
Buttocks, thighs
Between fingers
Genitalia
Scabies (PSI)
Treatment
Topical sulfur preparations
One-two applications daily
Launder personal items
No disinfectant
Ringworm (PSI)
Ringworm - an infection caused by a
fungus
Jock itch – form of ringworm on
groin area
Athlete’s foot – fungal infection of
foot (feet)
Fungus
live and spread on the top layer of
the skin and on the hair
grow best in warm, moist areas,
contagious via skin-to-skin contact
with a person or animal that has it or
when you share things like towels,
clothing, or sports gear.
You can also get ringworm by
touching an infected dog or cat,
although this form of ringworm is not
common.
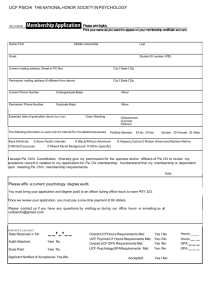
Psoriasis
Lifelong disorder
Exacerbations
Remissions
Cannot be cured
Psoriasis
Pathophysiology
Scaling disorder
Underlying dermal inflammation
Abnormality in proliferation of epidermal cells
in outer skin layers
Normal – 28 days to shed cells
Psoriasis Cells shed every 4-5 days
Psoriasis
Cause-unknown
Genetic predisposition
Environmental factors
May appear after skin trauma
Sunburn
Surgery
Psoriasis
Improves in warmer climates
Aggravated by
Infections
Streptococcal throat infection
Candida infections
Hormonal changes
Psychological stress
Psoriasis
Assessment
History
Family history
Age at onset
Disease progression
Pattern of recurrences
Gradual or sudden
Psoriasis Vulgaris
{Ordinary/Common}
Most common
Thick erythematous papules or plaques
Surrounded by silvery white scales
Psoriasis Vulgaris
{Ordinary/Common}
Common sites
Scalp
Elbows
Trunk
Knees
Sacrum
Extensor surfaces of limbs
Skin Cancers
Overexposure to sunlight
Common skin cancers
Squamous cell carcinoma
Basal cell carcinoma
Melanoma
Actinic Keratosis
Pre-malignant lesions
Cells of epidermis
Chronically sun-damaged skin
Can lead to squamous cell carcinoma
Squamous Cell Carcinoma
Malignant neoplasms of epidermis
Invade locally
Potentially metastic
Ear
Lip
External genitalia
Cause
Repeated irritation or injury
Basal Cell Carcinoma
Basal cell layer of epidermis
Lesions go unnoticed
Metastasis rare
Underlying tissue destruction progresses
to underlying vital structure
Melanomas
Pigmented malignant lesions
Originate in melanin-producing cells of
epidermis
Melanomas
Risk factors
Genetic predisposition
Excessive exposure to UV light
Precursor lesions resembling unusual
moles
Highly metastatic
Survival depends on early diagnosis and
treatment
Skin Cancers
Incidence/Prevalence
Light skinned persons
Outside work
Higher altitudes
Chemical carcinogens
Type I - Often burns, rarely tans. Tends to have freckles, red or fair hair,
and blue or green eyes.
Type II - Usually burns, sometimes tans. Tends to have light hair, and
blue or brown eyes.
Type III - Sometimes burns, usually tans. Tends to have brown hair and
eyes.
Type IV - Rarely burns, often tans. Tends to have dark brown eyes and
hair.
Type V - Naturally black-brown skin. Often has dark brown eyes and hair.
Type VI - Naturally black-brown skin. Usually has black-brown eyes and
hair.
Skin Cancers
Prevention
Avoid exposure to sunlight
Use of sunscreen SPF30 or greater
Skin Cancers
Assessment
Age
Race
Family history
Removal of skin growths
Skin Cancers
Assessment
Change in
Size, Color, Sensation
Of any
Mole, Birthmark, Wart, Scar
Hair-bearing areas of body
Skin Cancers
Interventions: Radiation therapy
Elderly
Large, deeply invasive basal cell tumors
Poor risk for surgery
Malignant melanoma resistant
May be used in combination with systemic
chemotherapy
Skin Cancers
Interventions: Surgery
Cryosurgery
Local application of liquid nitrogen
Cell death
Tissue destruction
Hemorrhagic blister formation x 1-2 days
Nursing Care
Clean site with hydrogen peroxide
Topical antibiotic may be ordered
Skin Cancers
Interventions: Plastic or reconstructive
surgery
Wound flaps
Pressure wounds
Skin Flap vs. Skin Graft
Skin Flap
Segment of tissue
attached on one end
while other end is
moved to new site
Nursing Care
Assess for infection
Assess circulation of
tissue
Skin Graft
Section of skin
detached &
transferred
Nursing Care
Keep affected part
immobilized
Inspect dressing
After 2-3 weeks,
massage with oil
No heating pads or
sun exposure
Pressure Ulcers
Etiology
Pressure Ulcers
Etiology
Immobility
Impaired sensory perception or cognition
Decreased tissue perfusion
Decreased nutritional status
Friction and shear
Increased moisture
Pressure Ulcers
Stages
Pressure Ulcers
Stages
Stage I
Non-blanchable erythema
Tissue swelling
C/O discomfort
Stage II
Break in skin
Epidermis
Dermis
Necrosis
Pressure Ulcers
Stages
Stage III
Subcutaneous tissue
Deep crater
With undermining
Without undermining
Stage IV
Underlying structures
May have large undermined area
Pressure Ulcers
Nursing Care
Relieve pressure
Proper positioning
Improve mobility
Improve sensory perception
Improve tissue perfusion
Improve nutritional status
Reduce friction and shear
Minimize moisture
Burns
1st degree – partialthickness (superficial)
2nd degree – partialthickness (deep)
3rd degree – fullthickness
Chemical burns
Electrical burns
Thermal burns
Sunburn
Burns
Extent of burn injury
Rule of nines
Stages of care
I – Emergent
II – Acute
III - Rehabilitation
Burns
Tests
Wound cultures
CBC, BUN, glucose, electrolytes, urine studies
Interventions
IV fluid replacement
Antibiotic/antimicrobial agents
Analgesics
Burns
Treatment
Debridement & cleaning
Dressing
Mechanical, chemical, surgical
Escharotomy
Open, closed, biological, synthetic
Skin grafts
Autograft
Split-thickness
Full-thickness
Burn Care
Impaired gas exchange
Impaired skin integrity
Deficient fluid volume
Pain
Ineffective peripheral tissue perfusion
Risk for sepsis
QUESTIONS?