Chapter 63 Management of Patients with Neurologic Trauma
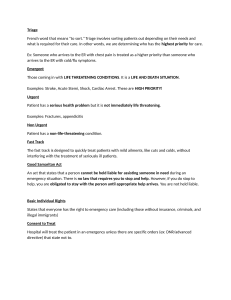
advertisement

1 Head Injury A broad classification that includes injury to the scalp, skull, or brain 1.4 million people receive head injuries every year in the U.S. The most common cause of death from trauma Most common cause of brain trauma is MVA Group at highest risk group for brain trauma is males age 15–24 Those younger than 5 years and the elderly are also at increased risk Prevention 2 Pathophysiology of Brain Damage Primary injury: due to the initial damage Contusions, lacerations, damage to blood vessels, acceleration/deceleration injury, or due to foreign object penetration Secondary injury: damage evolves after the initial insult Due to cerebral edema, ischemia, or chemical changes associated with the trauma 3 Pathophysiology of Traumatic Brain Injury 4 Manifestations Manifestations depend upon the severity and location of the injury Scalp wounds Tend to bleed heavily, and are also portals for infection Skull fractures Usually have localized, persistent pain Fractures of the base of the skull Bleeding from nose, pharynx, or ears Battle’s sign—ecchymosis behind the ear CSF leak—halo sign—ring of fluid around the blood stain from drainage 5 Basilar Fractures Allow CSF to Leak from the Nose and Ears 6 Manifestations of Brain Injury Altered LOC Pupillary abnormalities Sudden onset of neurologic deficits and neurologic changes; changes in sense, movement, reflexes Changes in vital signs Headache Seizures 7 Brain Injury Closed brain injury (blunt trauma): acceleration/deceleration injury occurs when the head accelerates and then rapidly decelerates, damaging brain tissue Open brain injury: object penetrates the brain or trauma is so severe that the scalp and skull are opened Concussion: a temporary loss of consciousness with no apparent structural damage Contusion: more severe injury with possible surface hemorrhage Symptoms and recovery depend upon the amount of damage and associated cerebral edema Longer period of unconsciousness with more symptoms of neurologic deficits and changes in vital signs 8 Brain Injury Diffuse axonal injury: involves widespread damage to axons in the cerebral hemispheres, corpus callosum, and brain stem. It can be seen with mild, moderate, or severe head trauma. Patient develops immediate coma. Intracranial bleeding Epidural hematoma Subdural hematoma Acute and subacute Chronic Intracerebral hemorrhage and hematoma 9 Concussion Patient may be admitted for observation or sent home Observation of patients after head trauma; report immediately Observe for any changes in LOC Difficulty in awakening, lethargy, dizziness, confusion, irritability, anxiety Difficulty in speaking or movement Severe headache Vomiting Patient should be aroused and assessed frequently 10 Location of Subdural, Intracerebral and Epidural Hemorrhages 11 Epidural Hematoma Blood collection in the space between the skull and the dura. Patient may have a brief loss of consciousness with return of lucid state then as hematoma expands increased ICP will often suddenly reduce LOC. An emergency situation! Treatment include measures to reduce ICP, remove the clot and stop bleeding—burr holes or craniotomy. Patient will need monitoring and support of vital body functions; respiratory support. 12 Subdural Hematoma Collection of blood between the dura and the brain Acute/Subacute Acute: symptoms develop over 24–48 hours Subacute: symptoms develop over 48 hours to 2 weeks Requires immediate craniotomy and control of ICP Chronic Develops over weeks to months Causative injury may be minor and forgotten Clinical signs and symptoms may fluctuate Treatment is evacuation of the clot 13 Intracerebral Hemorrhage Hemorrhage occurs into the substance of the brain May be due to trauma or a nontraumatic cause Treatment Supportive care Control of ICP Administration of fluids, electrolytes, and antihypertensive medications Craniotomy or craniectomy to remove clot and control hemorrhage; this may not be possible due the location or lack of circumscribed area of hemorrhage 14 Diagnostic Evaluation Physical and neurologic exam Skull and spinal x-rays CT scan MRI PET (Positron emission tomography) 15 Management of the Patient with a Head Injury Assume cervical spine injury until this is ruled out Therapy to preserve brain homeostasis and prevent secondary damage Treat cerebral edema Maintain cerebral perfusion; treat hypotension, hypovolemia and bleeding, monitor and manage ICP Maintain oxygenation; cardiovascular and respiratory function Manage fluid and electrolyte balance 16 Supportive Measures Respiratory support; intubation and mechanical ventilation Seizure precautions and prevention NG to manage reduced gastric motility and prevent aspiration Fluid and electrolyte maintenance Pain and anxiety management Nutrition 17 Nursing Process: The Care of the Patient with Brain Injury—Assessment Health history with focus upon the immediate injury, time, cause, and the direction and force of the blow Baseline assessment LOC—Glasgow Coma Scale Frequent and ongoing neurologic assessment Multisystem assessment 18 Nursing Process: The Care of the Patient with Brain Injury—Diagnoses Ineffective airway clearance and impaired gas exchange Ineffective cerebral perfusion Deficient fluid volume Imbalanced nutrition Risk for injury Risk for imbalanced body temperature Risk for impaired skin integrity Disturbed thought patterns Disturbed sleep pattern Interrupted family process Deficient knowledge 19 Collaborative Problems/Potential Complications Decreased cerebral perfusion Cerebral edema and herniation Impaired oxygenation and ventilation Impaired fluid, electrolyte, and nutritional balance Risk of posttraumatic seizures 20 Nursing Process: The Care of the Patient with Brain Injury—Planning Major goals may include Maintenance of patent airway, Adequate cerebral perfusion pressure (CPP), Fluid and electrolyte balance, Adequate nutritional status, Prevention of secondary injury, Maintenance of normal temperature, Maintenance of skin integrity, Improvement of cognitive function, Prevention of sleep deprivation, Effective family coping, Increased knowledge about rehabilitation process, and Absence of complications. 21 Interventions Ongoing assessment and monitoring is vital Maintenance of airway Positioning to facilitate drainage of oral secretions with HOB usually elevated 30° to decrease venous pressure Suctioning with caution Prevention of aspiration and respiratory insufficiency Monitor ABGs, ventilation, and mechanical ventilation Monitor for pulmonary complications, potential ARDS 22 Interventions I&O and daily weights Monitor blood and urine electrolytes and osmolality and blood glucose Measures to promote adequate nutrition Strategies to prevent injury Assessment of oxygenation Assessment of bladder and urinary output Assessment for constriction due to dressings and casts Pad side-rails Mittens to prevent self-injury; avoid restraints 23 Interventions Strategies to prevent injury Reduce environmental stimuli Adequate lighting to reduce visual hallucinations Measures to minimize disruption of sleep-wake cycles Skin care Measures to prevent infection Maintaining body temperature Maintain appropriate environmental temperature Use of coverings—sheets, blankets to patient needs Administration of acetaminophen for fever Cooling blankets or cool baths; avoid shivering 24 Interventions Support of cognitive function Support of family Provide and reinforce information Measures to promote effective coping Setting of realistic, well-defined, short-term goals Referral for counseling Support groups Patient and family teaching 25 Spinal Cord Injury (SCI) Definition: Fracture or displacement of one or more vertebrae causing damae to spinal cord and nerve roots with resulting neurological deficit and altered sensory perception or paralysis or both. There will be a total or partial absence of motor and/or sensory function below the level of injury. (Ignatavious and Workman, 2006) 26 Spinal Cord Injury (SCI) A major health problem 200,000 persons in the U.S. live with disability from SCI Causes include MVAs (35%), violence (24%), falls (22%), and sports injuries (8%) Males account for 82% of SCIs Young people ages 16–30 account for more than half of all new SCIs African–Americans are at higher risk Risk factors include alcohol and drug use Prevention 27 Spinal Cord Injury The result of concussion, contusion, laceration or compression of spinal cord. Primary injury is the result of the initial trauma. Secondary injury is usually the result of ischemia, hypoxia, and hemorrhage that destroys the nerve tissues. Secondary injuries are thought to be reversible/preventable during the first 4–6 hours after injury. Treatment is needed to prevent partial injury from developing into more extensive, permanent damage. 28 Clinical Manifestations Manifestations depend on the type and level of injury Incomplete spinal cord lesions (the sensory or motor fibers, or both, are preserved below the lesion): below the injury; total sensory and motor paralysis, loss of bladder and bowel control (usually with urinary retention and bladder distention), loss of sweating and vasomotor tone, & marked reduction of blood pressure. Complete spinal cord lesion (total loss of sensation and voluntary muscle control below the lesion): paraplegia or tetraplegia. If conscious, the patient usually complains of acute pain in the back or neck In high cervical cord injury, acute respiratory failure is the leading cause of death. 29 Spinal and Neurogenic Shock Spinal shock A sudden depression of reflex activity below the level of spinal injury develops due to the loss of autonomic nervous system function below the level of the lesion Muscular flaccidity, lack of sensation and reflexes Neurogenic shock Due to the loss of function of the autonomic nervous system Blood pressure, heart rate, and cardiac output decrease Venous pooling occurs due to peripheral vasodilation Paralyzed portions of the body do not perspire 30 Medical Management: Acute Phase Goals: Prevent further SCI and observe for signs of neurological deficit High dose corticosteroids (controversial) Research is continuing Medical management: Pharmacologic therapy Respiratory therapy Skeletal fracture reduction and traction Surgical management 31 Nursing Process: The Care of the Patient with SCI—Assessment Monitor respirations and breathing pattern Lung sounds and cough Monitor for changes in motor or sensory function; report immediately Assess for spinal shock Monitor for bladder retention or distention, gastric dilation, and ilieus Temperature; potential hyperthermia 32 Nursing Process: The Care of the Patient with SCI—Diagnoses Ineffective breathing pattern Ineffective airway clearance Impaired physical mobility Disturbed sensory perception Risk for impaired skin integrity Impaired urinary elimination Constipation Acute pain 33 Collaborative Problems/Potential Complications DVT Orthostatic hypotension Autonomic dysreflexia 34 Nursing Process: The Care of the Patient with SCI—Planning Major goals may include improved breathing pattern and airway clearance, improved mobility, improved sensory and perceptual awareness, maintenance of skin integrity, promotion of comfort, and absence of complications. 35 Promotion of Effective Breathing and Airway Clearance Monitor carefully to detect potential respiratory failure Pulse oximetry and ABGs Lung sounds Early and vigorous pulmonary care to prevent and remove secretions Suctioning with caution Breathing exercises Assisted coughing Humidification and hydration 36 Improving Mobility Maintain proper body alignment Turn only if spine is stable and as indicated by physician Monitor blood pressure with position changes PROM at least four times a day Use neck brace or collar, as prescribed, when patient is mobilized Move gradually to erect position 37