e983cc6dc44ea1d7381455cdbb55c3f7

Retroperitoneal surgery
By
2
Dr. Khattab Omar, MD
Prof. & Head of Obstetrics and Gynaecology Department
Faculty of Medicine, Al-Azhar University, Damietta
Introduction
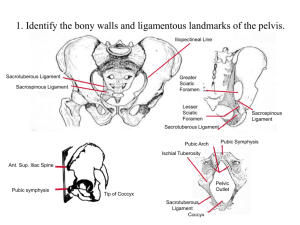
Retroperitoneal space of the true pelvis differs from retroperitoneal areas elsewhere in the abdomen by the presence of the sub-peritoneal areolar
(cellular) connective tissue.
We can recognize about 6 retroperitoneal spaces.
Cardinal lig
The subperitoneal area of the pelvis is partitioned into potential spaces by the various organs & their respective fascial coverings, and by the selective thickenings of the endopelvic fascia into ligaments and septa.
Vesical fascia
Cut edge of the peritoneum
Vesicovaginal lig. & space
Indications for development of retroperitoneal surgical approaches
1- Malignancy & Lymphadenectomy.
2- Endometriosis.
3- Chronic PID.
4- Tubo-ovarian abscess.
5- Large or interligamentous myoma
6- Complications in post-hysterect. reserved ovaries.
7- Hypogastric artery ligation.
8-Vaginally-inaccessible urinary fistula
9- Colpopexy.
10- Laparoscopic hysterectomy.
The pararectal space
Boundaries:
Laterally by the levator ani, medially by the rectum & rectal pillars,
Posteriorly above the ischial spine by the anterolateral aspect of the sacrum.
anteriorly and superiorly peripheral part of the cardinal ligament and the uterine artery divide the paravesical & the pararectal spaces.
Steps
To best develop the pararectal space, dissect between the first portion of the anterior division of the internal iliac artery laterally and the ureter medially.
The uterosacral ligament and the ureter are located very near to each other between the rectovaginal and pararectal spaces.
Remain close to the rectum to avoid the internal iliac vein and its side wall tributaries. Bleeding from these veins might kill the patient.
Laparoscopically
Developing the pararectal space laparoscopically; dissecting behind the uterine artery.
Laparoscopically
The uterine artery and the round ligament are divided and the incision is extended along the anterior broad ligament and bladder peritoneum.
The infundibulopelvic ligament has been divided and the ureter is displaced laterally to extend the peritoneal incision from the broad ligament to just below the uterosacral ligaments. The peritoneum is separated from the uterosacral ligaments, and the peritoneal incision is continued along the posterior cul-de-sac.
The uterosacral ligaments are coagulated and divided (inset).
Entering the retroperitoneum
- A preoperative IVU is recommended.
- In most cases, the round ligament may be divided and the peritoneum lateral to the infundibulopelvic ligament incised without difficulty.
- With large masses or when the anatomy is severely distorted, a paracolic or lateral psoas approach is required.
The round ligament approach
Placing a retractor near to the round ligament provides upward traction on it.
The ligament is then picked up & transfixed.
The broad lig. should be incised sharply in its lateral portion overlying the psoas Ms.
The peritoneum can then be incised cephalad lateral and parallel to the ovarian vessels.
This is followed by sharp & blunt dissection.
The initial dissection should be bounded by the posterior leaflet of the broad ligament
& the ureter medially (the ureter attaches to the broad lig. peritoneum) and the iliac vessels and the pelvic side wall laterally.
The paracolic approach
It is useful when the pelvic anatomy is severely distorted and the round lig not easily identified, or if the pelvis is occupied with a mass.
The paracolic peritoneum is elevated and incised.
The incision begins over the psoas muscle lateral to the ureter and ovarian vessels.
Post
Lt
Rt
Anter
The incision begins over the psoas muscle lateral to the ureter and ovarian vessels.
This is followed by combined sharp and blunt dissection to mobilize medially the coecum or sigmoid colon, or to visualize the ureters.
Dissection is continued down into the pelvis using the ureter as the landmark (ureteric catheter ± inserted) around which both the ovarian and the iliac vessels may be identified.
The retroperitoneal space may also be entered over or lateral to the psoas muscle.
Begin and stay medial to the iliac vessels .
Conclusion
Retroperitoneal approaches might be the magic key to navigate through the darkness of frozen or severely distorted pelvis.
Retroperitoneal navigation should be conducted very cautiously to avoid injury to important structures, particularly veins.