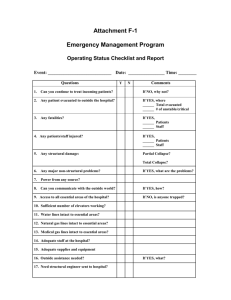
b) Current pressure on hospital beds
advertisement

Mental Health and Dementia Inpatient Services Redesign - Summary What is this summary about? Bath and North East Somerset Clinical Commissioning Group (BaNES CCG) and Avon and Wiltshire Mental Health Partnership NHS Trust (AWP) are thinking about the future of mental health and dementia inpatient care across Bath and North East Somerset (B&NES). Having heard from lots of partners, including service users and carers, they now have 4 options to help improve the care that people receive. This is a chance to say what you think about these options. What do you need to do? This 4 page summary gives an overview of the information used to develop these 4 options, and what work has been done so far to reach this point. Options - The 4 options that are proposed are listed in more detail in the ‘Options paper’. This includes the benefits and issues associated with each one. See W: (LINK) Full briefing - This is only a summary of the process so far. If you want to read more see the full ‘Briefing Paper for Mental Health and Dementia Inpatient Services Redesign’ (add link) Survey - Once you have read the Options paper and have made your choice about which option you feel BaNES CCG and AWP should take, please complete the short survey W: (add link) Why is this redesign happening? BaNES CCG and AWP, the local specialist mental health services provider, are thinking about mental health and dementia inpatient services at the same time to try and make sure that staff, money and buildings are used efficiently and support the people who need them most, now and in the future. What are they trying to achieve? The redesign aims to deliver best value for money, and accessible and effective services. That means services that support carers. It means services that allow people who are experiencing mental health problems to recover and lead satisfying, safe and meaningful lives in their local communities. This is not new. It is something that service users, carers, service providers and commissioners have been talking about for many years. This redesign has been shaped by all these discussions. What are the priorities of this redesign? 1) To provide inpatient services that offer safe and effective assessment and treatment for people experiencing severe mental distress. 2) To provide inpatient wards that are designed and built to a standard that supports people to feel better, and supports staff to be able to provide the best care. 3) For mental health services to work much more closely with other NHS services so people’s physical and mental health needs are met at the same time. 4) To provide services that respond to people’s needs, ensuring greater control by service users and their carers. 5) To provide adult and older adult services that give people care in or near to where they live. How are services being provided now? Currently adult acute mental health inpatient beds are located at the Sycamore Ward in the Hillview Lodge building on the Royal United Hospital (RUH) site in Bath. Sycamore Ward has 23 beds which provide specialist mental health assessment and treatment. Some of the people that access this ward will recover and not need another inpatient admission. Some may go on to receive treatment over the course of their lifetime. A report from the Care Quality Commission in June 2014, following a visit to the Sycamore Ward in 1 December 2013, confirmed issues with the building that AWP were already aware of. This confirmed that the accommodation is no longer fit for purpose. AWP felt that they needed to take action on Sycamore Ward and this resulted in: A reduction of beds at Hillview Lodge from 23 to 15. An agreement to take in people from B&NES only. A decision to prioritise older adults to go into more suitable facilities in Callington Road Hospital in Brislington or other neighbouring units depending on where the person lives. The removal of “swing beds” which are used as male or female beds depending on demand Building work to address patient safety. The longer term unsuitability of the Sycamore Ward is clear and further action has to be taken. This action is getting more and more urgent and this redesign is a major part. Currently inpatient assessment for people with dementia is located at Ward 4 at St Martin’s Hospital in Bath. There are 12 beds in Ward 4. Commissioners and staff are concerned about the limitations on Ward 4 due to its shape and size. It was not purpose-built to assess and treat people with severe dementia. This makes some aspects of delivering care challenging. Ideally an inpatient dementia ward should include: personalised bed areas for patients with familiar objects, like photos; good lighting; space for activities; calm spaces; obvious doorways so people can move about easily. These are not new concerns. It was noted in 2008, when the number of dementia beds at St Martin’s Hospital was reduced from 40 to 20, that dementia beds would be better suited to being on the RUH site in the future. It was felt this should be thought about as part of a wider improvement in all mental health inpatient facilities when the opportunity arose. Why is this change needed? a) Demographic pressure There were 179,900 B&NES residents in 2010, an increase of 1.1% (2,000 people) since 2009. This was slightly more than regional and national levels. The Office of National Statistics estimates the population of B&NES will increase by 12%, to 198,800, by 2026. This increase is expected to mainly be in older people; particularly those aged 80+. As a result it is safe to expect that demand for services, particularly for older adults, will increase. b) Current pressure on hospital beds This is being looked into at a national level because pressure on adult acute beds in mental health services has been increasing in recent years. Acute mental health beds at Sycamore Ward During the period April to December 2013, the 23 beds available within Sycamore Ward could provide 5,886 bed ‘days’. In reality, the total number of bed days occupied was 6,279, as people from Bristol, South Gloucestershire, North Somerset, Wiltshire and Swindon also required treatment. During this same period B&NES patients would have used beds in other areas, such as Wiltshire, Bristol, South Gloucestershire, Swindon and North Somerset. Dementia assessment beds at Ward 4 During April to December 2013, the 12 beds available within Ward 4 could provide 2,222 bed ‘days’. In reality, the total number of bed days occupied was 2,939, as people from Bristol, South Gloucestershire, North Somerset, Wiltshire and Swindon also required treatment. During this same period B&NES patients would have used beds in these other areas too. c) Delayed discharge from hospital People are experiencing delays when they are being discharged into a specialist dementia nursing 2 home. There is not enough provision to meet demand elsewhere so people are coming into B&NES. B&NES Council and other neighbouring authorities are working to try and increase the amount of nursing home care in the area. This will take time. d) Modelling future services BaNES CCG has developed some projections for the next ten years based on population growth. At the moment it seems there is just about the right level of provision (although bed pressure is beginning to being felt as explained above). It is felt therefore that an increase in bed numbers is a good idea to ensure that they keep up with the projected demand longer term. e) Financial investment to support change There is no intention to decrease the amount of money available to BaNES CCG to buy hospital bed space. The current amount of money is in place and there will be an assessment to see if any further investment is needed. AWP are already looking at ways of providing the money for the build. So, BaNES CCG and AWP know that: They have to provide new facilities for mental health inpatients. They have recommendations from previous dementia service redesigns to site the dementia inpatient wards on the RUH site. The current number of beds available is just about OK but is beginning to come under pressure. Delays in patient discharge from Ward 4 are increasing due to a lack of nursing home beds. Nationally there is pressure on mental health beds. There is commitment to financial stability (BaNES CCG) and investigating capital investment (AWP). What are the options for the future? Based on all this information BaNES CCG and AWP took suggestions to their partners for comment. These partners included: the CCG Operational Leadership Team and GPs, the Mental Health and Wellbeing Forum (which includes services users and their carers), Dementia Care Pathway Group members and Bath and North East Somerset Healthwatch members. The suggestions that these partners were asked to consider and comment on were: 1) Leave services as they are. 2) Do refurbishment works to Sycamore Ward only. 3) Redevelop all of the existing Hillview Lodge building for adults with mental health problems only. 4) Redevelopment and co-location of dementia beds and mental health beds into Hillview Lodge. 5) Empty, demolish and rebuild on Hillview Lodge site. 6) New build on the RUH site, where dementia services from Ward 4 can be combined with the mental health services from Sycamore Ward. 7) New build in a new location for both services. The feedback from partners on these suggestions was that co-locating mental health beds and dementia beds on the same site at RUH would be best. They felt this would cause the least disruption to service users, their carers and families, and would offer a purpose built design that could support both acute mental health and dementia care on a single site. Being on the RUH site would also link mental health services with physical health services, allowing people to be assessed in one place by different NHS services. Both mental health and dementia services on a new site is also an option for consideration and has been included in the survey for your feedback. 3