Electrocardiography Fall 2011 FINAL for
advertisement

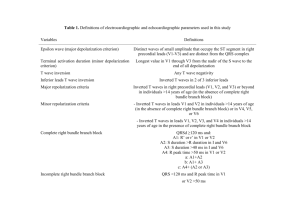
Introduction to Electrocardiography Information contained in the ECG Disturbances of rhythm and conduction. Ischemic damage to the myocardium. The anatomical orientation of the heart. Relative size of the heart chambers. The influence of some drugs and electrolyte disturbances (for example, hypokalemia). Interpretation of electrical activity of the heart Precise interpretation of electrical activity of the heart as recorded with electrodes on the skin is difficult because: The distribution of charge within the heart is multidirectional and constantly changing. The configuration of cardiac action potentials varies from region to region. The position of the heart changes continually throughout the cardiac cycle. Conductivity through the extracellular fluid is not uniform. The surface of the body is not simple geometrically. Cell model to show origin of electrocardiogram record: resting cell positive electrode ECG record Negative electrode Cardiac myocyte isoelectric In the resting cell the surface is uniformly positive compared to the cell interior. There is no potential difference between different points on the cell surface. The ECG records a baseline (the isoelectric line). Cell model to show origin of electrocardiogram record: partial depolarization creates a potential difference between two points on the cell surface Current flows from negative to positive regions positive electrode ECG record depolarization Negative electrode Depolarization of part of the cell membrane creates a potential difference between the resting and depolarized regions on the surface. By convention, current flows from negative to positive and from the depolarized region to the “resting” region. If the wave of depolarization is directed towards the positive electrode, the ECG records a positive (upward) deflection. Cell model to show origin of electrocardiogram record: complete depolarization returns the ECG signal to baseline positive electrode ECG record Negative electrode When the cell is completely depolarized, once again there is no potential difference between any two points on the outside of the cell membrane. The recorded potential returns to the baseline level. Cell model to show origin of electrocardiogram record: repolarization produces an ECG signal below baseline positive electrode ECG record Negative electrode repolarization As repolarization occurs, current flows in the opposite direction than during depolarization. Consequently the recorded potential is opposite in direction to the potential during depolarization. Cell model to show origin of electrocardiogram record: repolarization completed: ECG signal returns to baseline positive electrode ECG record Negative electrode Repolarization is slower than depolarization so the peak value is less than during depolarization and the duration of the wave is longer. With the return to the resting state the recorded potential returns to baseline. Standard labeling of an ECG waveform in lead 1 R Atrial depolarization T S P Q ST PR Atrial depolarization & conduction through AV node QRS QT Ventricular depolarization & atrial repolarization Ventricular repolarization Factors affecting the amplitude of the ECG signal Obese subject with hypothyroidism Hypertensive subject with cardiac hypertrophy (Signals are drawn to scale) The amplitude of the ECG signal is affected by the amount of myocardial tissue the orientation of the heart in the chest the thickness and type of tissue between the heart and the electrode. For example, pericardial fluid, emphysematous lung tissue or obesity increase electrical resistance between the heart and the electrodes, reducing the amplitude of the ECG signal. Correspondence between a ventricular action potential & the ECG P QRS 1 0 T 2 3 4 The QRS complex is produced by the summed upstrokes (phase 0) of the ventricular myocyte action potentials. The S-T segment corresponds to the plateaus of the action potentials. The T wave is produced by ventricular repolarization. Normal ECG intervals: calculating the intervals in an ECG helps determine if the recording is normal or what kinds of abnormalities may exist. ECG intervals (seconds) average range Events in heart 0.18** 0.12 to 0.20 Atrial depolarization & conduction through AV node QRS duration 0.08 0.06 to 0.10 Ventricular depolarization QT interval 0.40 Varies with HR Ventricular depolarization & repolarization ST interval 0.32 --- PR interval* Ventricles depolarized; ST interval normally lies on isoelectric line * Measured from the beginning of the P wave to the beginning of the QRS complex ** Shortens as heart rate increases from average of 0.18 at a HR of 70 to 0.14 a t a HR of 130. Path of excitation in the heart Sino-atrial node originates action potentials Conduction velocity for action potentials is greater in the Purkinje fibers than in myocytes so excitation spreads rapidly through the ventricles allowing coordinated contraction of the ventricular muscle. APs are propagated between myocytes via gap junctions. Atrial myocytes Atrioventricular node Bundle of His Right & left bundle branches Purkinje fibers Ventricular myocytes Path of repolarization Ventricular endocardium is depolarized before epicardium. The duration of action potentials in the endocardium is greater than the duration of APs in the epicardium. Myocytes in the epicardium begin to repolarize before myocytes in the endocardium. Therefore repolarization spreads through the ventricle in the opposite direction to depolarization, so in the ECG depolarization (QRS) and repolarization (T wave) are both positive deflections. Right & left bundle branches Purkinje fibers endocardium QRS epicardium P T Einthoven’s triangle: placement of electrodes RA + - - + RL (ground) + LL LA Einthoven’s triangle is a system of placing electrodes to measure the electrical activity of the heart in the frontal plane. Electrodes (red circles) are placed on the right arm (RA), left arm (LA) and left leg (LL). The electrodes are grounded to the right leg (RL). ECG Leads measure potential differences (voltages) between electrodes. Definition of leads in Einthoven’s triangle (frontal plane): Lead I: between RA and LA Lead II: between RA and LL Lead III: between LA and LL RA - Lead I + - Lead II LA Lead III + + LL Leads I, II & III are bipolar: they measure the potential difference (PD) between 2 points. Size & polarity of the potentials are related to the path of depolarization or repolarization RA - Lead I + - LA Normal range for the mean electrical axis is – 30 to + 90 degrees. - 30 Lead III Lead II Lead I (zero) + + + 90 LL The shaded arrow is a vector (has magnitude & direction). This vector represents depolarization during the QRS complex & is called the mean electrical axis of the heart in the frontal plane. The mean electrical axis is normally is 60 degrees to the horizontal. Example of a shift in the mean electrical axis Lead I RA + - - LA Lead III Lead II + + LL Example: a shift to the right to 120 degrees: Lead I polarity is reversed because projection of the vector on lead I is from + to pole. Lead II magnitude is decreased, lead III magnitude is increased. A shift in the electrical axis changes the magnitude & direction of the ECG signals. When evaluating an ECG the axis may be determined from the magnitude and direction of the signals in the six frontal plane leads. Einthoven’s triangle and the axial reference system for the ECG An axial reference system is used to compare tracings from all 6 leads in the frontal plane. The 6 leads include Leads I, II and III and the unipolar limb leads AVR, AVL, & AVF (next slide) RA -- Lead I +- LA I III Lead III Lead II + - 90° + LL Leads I, II & III of Einthoven’s triangle + 120 ° 0° II + 90 ° Leads I, II & III in axial reference system The unipolar limb leads AVR, AVL, & AVF are measured as the PD between one limb and the electrical average of the other two limbs. + + aVR aVL + aVR (augmented right arm) aVF aVF (augmented left foot) aVL (augmented left arm) Axial reference system: six leads measuring the ECG in the frontal plane - 90° For each lead, the arrow points toward the positive pole. - 150 ° An axis beyond - 30 ° is called left axis deviation. aVL aVR I III 0° II aVF An axis beyond + 90 ° is called right axis deviation. - 30 ° + 120 ° + 90 ° Normal range for the mean electrical axis is – 30 to + 90 degrees The mean electrical axis is determined from the magnitude and direction of the signals in the six frontal plane leads. V6 V5 LV Six standard precordial leads V4 V1 V1 V2 V3 V2 V3 V6 V5 V4 The 6 precordial leads (V1 to V6) measure potentials in a transverse plane around the apex of the heart at right angles to the frontal plane. They measure the PD between the electrode and ground so they are unipolar leads. There are 12 leads in a standard ECG Six leads meaure potentials in the frontal plane 3 Leads (I, II & III) for Einthoven’s Triangle 3 Calculated leads: aVR (augmented right arm) aVL (augmented left arm) aVF (augmented left foot) Six leads measure potentials in a transverse plane across the heart. Precordial leads V1 to V6 12 Lead ECG: Normal sinus rhythm at a rate of 71 beats/min, a P wave axis of 45°, and a PR interval of 0.15 sec. Cardinal features of sinus rhythm: The P wave is upright in leads I and II Each P wave is usually followed by a QRS complex The normal adult resting heart rate is 6099 beats/min ©2007 UpToDate Example: Ventricular depolarization recorded by precordial leads V1 & V6 (1) At rest ECG leads show baseline PD + - - - LV - - - + - - + V6 + - + - + -- + (2) Depolarization begins in the septum V6 - ++ + + + V1 V1 (3) Depolarization spreads to apex (4) Depolarization spreads to LV & RV V6 + - -- + + + + + + ++ - - V1 + - -- + - - + + + - + + + - V6 + + + ++ V1 + - -- Depolarization is complete - + + + - -- + + - + + + - - + ++ - + - + -- V1 Note that step 4 is repeated from previous slide V6 + + V6 + + (5) Depolarization is complete; trace returns to baseline. + -- (4) Depolarization spreads to LV & RV; signal from LV dominates + - + + + + + + ++ V1 + -- Calibration of the ECG Paper speed = 25 mm/sec 1 mm = 1/25 sec or 0.04 sec 1 sec 0.2 sec Calibration Signal (1 mV) paper speed = 25 mm/sec 0.1 mV 0.04 sec 1 mm Calculation of heart rate from the ECG 16 mm Small box = 1 mm2 Paper speed = 25 mm/sec 1 mm = 0.04 sec = 1 small box Heart rate = beats/min = [mm per minute]/[number of mm between beats], Substituting numbers: mm beats min Heart rate mm min beat 25 mm 60 sec beats sec min HR 94 16 mm min beat Since 1 small box = 0.04 sec, intervals can be calculated from trace also Heart Block Heart block is due to delay or blockade of excitation in the conducting system. First degree heart block refers to a prolonged PR interval (> 0.2 sec) and is due to a defect at the AV node & may be functional or structural. Functional block occurs when the conducting impulse reaches a region that is still refractory from the preceding depolarization. Causes include some anti arrhythmic drugs, or AV nodal ischemia. Structural block is due to irreversible damage in the conducting system, for example due to infarction or degeneration with aging. First degree block is usually benign. Second degree heart block refers to intermittent complete blockade of the conducting signal so that some P waves are not followed by a QRS complex. There are two types QRS and several causes. P P 2nd degree block Third degree heart block is complete dissociation between the atrial rhythm and the QRS complex. The ventricular rhythm is due to an ectopic pacemaker distal to the AV node. Third degree block requires treatment with a pacemaker. QRS 3rd degree block P P QRS P P Reentry and arrythmias Errors in conduction can cause abnormal rhythms or arrhythmias One common cause of potentially serious arrythmias is re-entry Reentry occurs when an anatomical or pathological fault causes action potentials to continuously circulate around an abnormal path in the myocardium Reentry may occur as multiple, irregular continuously moving circuits leading to fibrillation or disorganized contraction of the myocardium Reentry can occur where there is a branching path of myocardial tissue Normally APs in the connecting branch extinguish each other. Unilateral block with normal conduction velocity Cells in blocked area are in refractory period so AP cannot propagate in a retrograde direction Unilateral block with slow conduction Reentry: If conduction is slow, as APs travel in a retrograde direction, they reach tissue which has passed the refractory period and is excitable, so the APs continues to cycle. Conditions for reentry: A branching pathway of myocardium with unilateral block plus decreased conduction velocity. Conduction blocks may be caused by ischemia, inflammation, fibrosis or some drugs. Reentry circuits may cause tachycardia, atrial or ventricular fibrillation.