Clinical Mentorship and Assessment of Operating Department
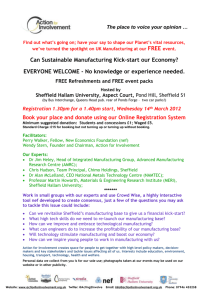
advertisement

Clinical Mentorship and Assessment of Operating Department Practitioner Students Mentor Preparation/Update Sheffield Hallam University © SHEFFIELD HALLAM UNIVERSITY 2009 Sheffield Hallam University 2007 1 SHU ODP mentorship preparation/update overview 2007 Introductions Levels of competence Aims Action planning Who’s who in the SHU ODP team Exercises What is mentorship and how does it Action plans relate to modern practice Placement review The philosophy of mentor preparation Student review Who can mentor Listening and trusting Supervision Interprofessional learning Scope of practice Codes of conduct Introduction to the modules Mentor update quiz Roles and responsibilities Questions Clinical assessment Evaluation Competence Reflection Direct observation Questions Mini assignments Sheffield Hallam University 2007 2 Aim of this session To discuss how you and I support students To introduce or update the assessment tools and strategies To introduce or update the paperwork To encourage you to think about the mentorship relationship. Sheffield Hallam University 2007 3 Who are the team at Sheffield Hallam University ? At present a team of 6 lecturers working alongside other university colleagues who also support student ODP's. John Rutherford Karen DeMasi Debbie Hall David Fotheringham Brears Martin Reilly Ray Swann Sheffield Hallam University 2007 4 What is Mentorship? The origins of the word spring from Homer's "The Odyssey", where Odysseus, off to war, chose "Mentor" (who was the goddess Athene), to protect and advise his son "Telemachus." This has translated to the modern day as an "experienced and trusted adviser" (Oxford Dictionary). The Dept of Health states that; Mentors & teachers are vital to the preparation of the next generation of practitioners. Sheffield Hallam University 2007 5 Mentors require "robust preparation" for their role. Mentor preparation equips appropriately qualified and experienced practitioners to assume responsibility for the student's learning in the practice setting, the quality of that learning, and the assessment of competencies to demonstrate the extent to which learning outcomes are met. (DoH 2001) MENTORS: •Facilitate student learning across pre & post registration programmes. •Supervise, support & guide students in practice in institutional and non-institutional settings. •Implement improved assessment procedures. Sheffield Hallam University 2007 6 What qualifications do I need to be a mentor for SHU ODP students? Qualified registered practitioner (ODP, Nurse, Other) At least 1 year post registration experience Recognised teaching qualifications Recognised mentorship courses Sheffield Hallam University 2007 7 Clarification Student supervision Sheffield Hallam University 2007 8 Supervision of ODP students while on Clinical placement A policy has been developed following consultation with clinical staff, by which ODP students should be supervised while on clinical placement. These guidelines protect patients, students & practitioners during clinical placement and assessments. These are an integral element of the Diploma HE in ODP. Supervised students are able to work safely and within their scope of practice Sheffield Hallam University 2007 9 Supervision of ODP students while on Clinical placement SUPERNUMERY STATUS- university students & not employees- should not be included 'in numbers'( please refer to Mentor handbook SHU 2007) SCOPE OF PRACTICE – Students and staff should be aware of their roles & responsibilities. Students who do not work within this scope either through choice or coercion could be disciplined. Placement sites knowingly allowing this may lose their eligibility to have students. GUIDELINES: Anaesthetic duties- Students must be supervised at all times by an appropriately qualified practitioner who is in the area where the student is working. Scrubbed duties- Someone will be scrubbed with the student at all times. PACU- Students should not be left unsupervised. Sheffield Hallam University 2007 10 Module overview Sheffield Hallam University 2007 11 Overview of SHU ODP student curriculum Semester 1 Semester 2 Interprofessional Education Year 1 120 Credits Clinical Education in ODP (30c) Principles of Anaesthetic Practice 1 (20c) Human Biology (10c) Foundations of Operating Department Practice (10c) Principles of Surgical Practice 1 (20c) Introduction to IT Skills (10c) Year 2 120 Credits Principles of Surgical Practice 2 (20c) Advanced Human Biology (20c) Interprofessional Education Clinical Education in ODP (20c) Principles of Anaesthetic Practice 2 (20c) Sheffield Hallam University 2007 Principles of Post Anaesthetic Care (10c) 12 Roles & Responsibilities The studentTo reflect on the fact that they are undertaking a programme of learning that will lead to a professionally recognised qualification. Professional behaviour; Time keeping, attendance in clinical & academic placements. Guidelines as detailed in the preparation for placement document on the ODP website At least 80% attendance in university and 100% attendance in clinical placement On Clinical placement these guidelines should be followed; Students must always work under direct supervision. Students must always treat mentors with respect Students must never undertake duties outside their capabilities. Students in doubt should always ask for assistance or seek advice from university. No-one else can take responsibility for the students action's. They alone will be held responsible professionally/legally if they take on duties that are outside their role. Sheffield Hallam University 2007 13 Roles & Responsibilities Placement co-ordinator Responsible for organising student's clinical experience. Is the 'link' between all the phases of the students education & will link with the university & clinical mentors to ensure that students receive the experience they require to complete the course and meet standards of proficiency. Responsible for ensuring students are progressing in the clinical setting. Complete End of semester reviews. Check the work students have undertaken in each allocation. Liase with mentors as required. Responsible for the support of students (as an 'expert' in ) the use of reflection Sheffield Hallam University 2007 14 Roles & Responsibilities Clinical mentor The person who will work with the student most of the time on clinical placement. Will give support & instruction Will assess competence using methods described and support the student in the use of reflection Students may find themselves working with a number of mentors/practitioners. A multiple mentor model allows the NAMED mentor to organise a placement to ensure that the student works with appropriate practitioners at all times. Ensuring assessment of skills is done accurately. Assessment in practice is randomly monitored by the visiting lecturer Sheffield Hallam University 2007 15 Roles & Responsibilities Clinical Link lecturer A member of the university teaching staff linked to the clinical placement. Will visit 5 times per year. To ensure students are progressing to the correct level, have completed the work required of the portfolio. Assist in the event of placement site problems. Monitors live assessments to ensure consistency Sheffield Hallam University 2007 16 Clinical Assessments! PORTFOLIO DEVELOPMENT Assessment process Clinical competencies The assessment process for the clinical competencies and the clinical education modules are intrinsically linked. The clinical work and underpinning knowledge created by completing the clinical skills will assist in the development of the portfolio required at the end of the module. Reflective accounts The reflective accounts required in the review process may be be used in the portfolio, and any evidence used to show knowledge to the clinical mentors can be developed to form part of the information in the portfolio, in addition reflective practice is an ideal assessment method in clinical competence, supporting live observation. Reflection is an important component in the assessment strategy and students are encouraged to use this as one of their assessment methods in practice to support observed practice Sheffield Hallam University 2007 17 Clinical Competencies To pass the clinical competencies in the portfolio the student will need to show competence in both 1. the direct observation section (mentor watching them work) and 2. one of the other areas to indicate they understand the underpinning principles, policies and responsibility of the role. However in areas where student are unable to be assessed using direct observation, two of the other forms of evidence can be used but only as detailed in the assessment guidelines for clinical education. Student and mentor should highlight in the plan how they intend to show competence in the assessments Sheffield Hallam University 2007 18 Assessment areas Direct Observation. This involves observing the student undertake the tasks in the clinical competencies until they meet the required level for the year. The number of times required to show competence will depend of the student’s ability and the area of practice. Verbal/Written Questions. The easiest way to assess the students underpinning knowledge of the skills they are undertaking. Verbal questions are effective and quick and can be undertaken in the clinical area whilst you are working with the student. However be sure to make some notes though as a record of what you asked. Often the most effective way of assessing someone's knowledge is to get them to talk it through, reflection is a powerful tool as it comes from real situations. Sheffield Hallam University 2007 19 Assessment areas Written Questions. These can be either given to the student to take away and do in their study time or completed in the presence of the assessor. There is no minimal or maximum number of questions; however it is important to use the appropriate competence levels for marking and assessing knowledge. Again it is essential for the student to have a record of the questions and a conformation of competence. Assignments. The university sees small assignments as a useful tool in assessing students knowledge in practice. It is advised that they should be no more than 500 words in length and where possible the student should reference their work. This method should only be used in circumstances where live assessment is impossible and this is highlighted in the assessment criteria of the competencies document Sheffield Hallam University 2007 20 Assessment areas Reflective accounts by the student, students are encouraged to keep a reflective log of their experiences and use reflection to show how their role is incorporated in the care of patients, team working and using evidence based practice. These can be used as evidence if the information is appropriate for the assessment being undertaken. Sheffield Hallam University 2007 21 Reflection What is reflection? Reflection has been described as a dimension of critical thinking, a term in which individuals engage to explore their experiences in order to lead to new understandings. By using reflection as a learning tool and as a component of learning through experience it helps students to integrate the theory and the practice. o Models of Reflection A model is a structured framework which has been shown to be effective in promoting and enhancing reflection. Some models include: Gibbs, Carper, and Johns. e.g Gibbs (1988) This is simple to use and easy to understand. It has 5 components; 1. A description of what has happened 2. Feelings – what you were thinking and feeling 3. Evaluation – what was good and bad about the experience 4. Conclusion – what else could have been done? 5. Action plan – if it arose again what would you do? Sheffield Hallam University 2007 22 Year 1 Competencies To progress from year one to year two students must show competence in all the clinical skills listed in the clinical competencies. However the university appreciates that by the end of year one the student will not have achieved the level of a competent practitioner. The level the university wishes the mentors to assess in year one is to the level of “SUPERVISED PARTICIPANT”. The mentor is assessing the students progression from observer in the clinical setting to a level where they are actively involved in patient care. Students need to show progression of skills, development of knowledge to be able to recognise links between theory and practice and the ability to undertake routine procedures Sheffield Hallam University 2007 23 Year 2 Competencies In year two of the course students must show competence in all of the clinical skills listed in the clinical competencies. The level the university wishes the mentors to assess the students to in year two is to the level of “COMPETENT” You can interpret this as SAFE OR UNSAFE if that helps The mentor is assessing the student to the level of a newly qualified practitioner. who is able to undertake the skills expected of an Operating Department Practitioner, without specialty in one area. The student is showing competence in routine and emergency procedures where the basic skills of an Operating Department Practitioner are required. Sheffield Hallam University 2007 24 Action Planning Can be completed by the mentor or the student. All decisions need to be agreed by both parties. The information on the action plan can include any of the following items. Period of placement dates Roles to be undertaken Hours of work (NB No more than 37 hrs per week) Who you will be working with. Skills to be focussed on in placement (from clinical competencies) Any learning or teaching required Assessment methods Review times Sheffield Hallam University 2007 25 Action plans for clinical placements STUDENTS NAME……………………………………………… MENTOR………………………………………………………… OTHER STAFF INVOLVED IN PLACEMENT……………………………………………….. PLACEMENT AREA……………………………………… SPECIALITY………………………………………………. CLINICAL ROLE…………………………………………. Plan for achievement of clinical skills Sheffield Hallam University 2007 26 Exercise; Lets do some exercises Sheffield Hallam University 2007 27 Exercise; Action planning In pairs discuss how you would plan to support a year 2 student in the clinical area, formulate an action plan and discuss how you will judge competence. It may be useful for one person to play the student. Discuss how you will ensure that you are assessing consistently Sheffield Hallam University 2007 28 Exercise; Placement review Working alone and using the copy of the placement audit tool look at your placement area and fill in the audit honestly, then join up with someone else and decide what you think could be done better in your department to support students. 1. Where are we now? 2. If there are aspects of educational support we need to improve, how can we achieve these? Sheffield Hallam University 2007 29 Exercise; Student review Working alone and using the copy of the student audit tool look at your placement area and fill in the audit honestly. Think about what the student might say about the placement that you work in. What might they say about the opportunities, the facilities, the mentors? Put yourself in their shoes. Be honest but keep this one to yourself, This could be a placement changing experience. Sheffield Hallam University 2007 30 Exercise; Listening and Trusting Working in groups of 3 identify mentor, student and observer. Mentor and student are seated and blindfolded. The observer chooses 10, 2 dimensional plastic shapes from a selection and gives 5 random shapes to each. Some shapes will be different colours, there is a selection of profiles. The object of the exercise is for student and mentor to match as many objects as possible without touching the other’s objects. Each may ask as many questions as they like of the other. Both can ask the observer “what colour is this” repeatedly if necessary. They may not ask the observer any other questions The purpose of the exercise is for each to experience the building of a questioning trusting relationship, much like mentorship really. Sheffield Hallam University 2007 31 Exercise; Interprofessional learning Examine the ways that the multi-professional team in your clinical area work together. Make a note of these. Are there ways that this team also learn together? How do health care students in your clinical area learn and work together? What learning opportunities can you provide to assist health care students to experience team work? What learning opportunities can you provide to assist health care students to learn together? Sheffield Hallam University 2007 32 Exercise: Reflection In groups of 3 each group document how you could assess a student using a model of reflection; each choosing a different competency to assess. each group compare methods in order to show consistency of assessing. Sheffield Hallam University 2007 33 Mentor update quiz Questions The following questions are ones commonly asked by and sometimes of mentors. What do you think the correct answers are? Brief answers are given later. Students and mentors are individuals and their circumstances may require individual consideration, so if the answers given do not reflect your answer for any of the question, seek further guidance from your clinical link lecturer. Sheffield Hallam University 2007 34 Mentor update quiz 1. Why do students need to be assessed in practice? 2. What is the best way of assessing clinical skills, in your experience? 3. Who should teach clinical skills? 4. Who should assess clinical skills competency? 5. Where should clinical skills be assessed? 6. How do you feel clinical staff are rewarded for this work? How could they be rewarded? 7. What other aspects of practice should be assessed? Sheffield Hallam University 2007 35 Mentor update quiz 8. Must the student ‘work’ with me the whole time? 9. What do I do first when the student arrives on the ward? 10. What is the role of the Link Lecturer in supporting the student and me? 11. What is the role of the Personal Tutor in supporting the student and me? 12. What do I do if the student does not co-operate with me? 13. How do I get hold of the documents on which to record the student’s progress? 14. What happens to the assessment document after the student and I have filled it in? 15. How can I find out who is the Personal Tutor of a particular student? Sheffield Hallam University 2007 36 Mentor update quiz 16. How can I find out who the Link Lecturer is for the department? 17. What happens if an assessment document gets lost? 18. Who has custody of the assessment document during the student’s placement? 19. What do I do if the student is not performing well enough? 20. What can I do if a student is dangerous? 21. What can I do to reward the student who is exceptional? Sheffield Hallam University 2007 37 Mentor update quiz 22. Must students do as clinical staff tell them? 23. What preparation does the student have before they come on a placement? 24. What should I do when a student is absent or sick? 25. What are the most common problems encountered by students and mentors? 26. Can students ‘work’ double shifts or other unusual shift patterns? 27. What happens to student evaluation forms? 28. What if a student disagrees with my judgement? 29. At what stage do I involve School staff if I have concerns about a student? 30. What if the student wants to change their mentor? Sheffield Hallam University 2007 38 Mentor update quiz 31. How do I assess a student using reflection? Sheffield Hallam University 2007 39 Mentor update quiz Finished? If you are looking at this on line the answers to this quiz are in a word document on the website Sheffield Hallam University 2007 40 Bibloiography AODP (MAY2006V2) Curriculum Document. AODP (2006) Qualifications Framework for Mentors Supporting Learners in Practice: Standards and Guidance for Mentors and Practice Placements in Support of Pre-registration Diploma of Higher Education in Operating Department Practice Provision Barrett R. Mentor supervision and development - exploration of lived experience Career Development International, Volume 7, Number 5, 2002 , pp. 279-283(5) Emerald Group Publishing Limited Benner P (1984) From Novice to Expert: Excellence and Power in Clinical Nursing Practice. Menlo Park, California, Addison-Wesley. The Bristol Royal Infirmary Inquiry (2001). London, The Stationary Office. http://www.bristol-inquiry.org.uk/final_report/rpt_print.htm Department of Health (2002) Learning from Bristol. London, The Stationary Office. http://www.doh.gov.uk/bristolinquiryresponse/bristolresponsefull.pdf Department of Health (1999) Making a Difference. London: Department of Health. http://www.doh.gov.uk/pub/docs/doh/nurstrat.pdf ENB and DoH (2001a) Preparation of Mentors and Teachers. London, The English National Board for Nursing, Midwifery and Health Visiting and The Department of Health. Godshalk, V.M. and Sosik, J.J. (2000), “Does mentor-prote´ge´ agreement on mentor leadership behavior influence the quality of a mentoring relationship?”, Group and Organization Management, Vol. 25 No. 3, pp. 291-317. Gibbs (1988) The Reflective Cycle Learning By Doing; a Guide to teaching and learning methods http://www.nmc-uk.org/cms/content/Publications/!teachers.pdf Sheffield Hallam University 2007 41