Scientific Affairs & Research
advertisement

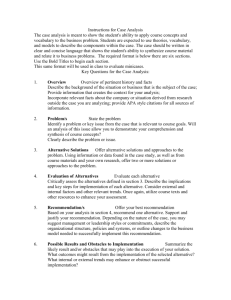
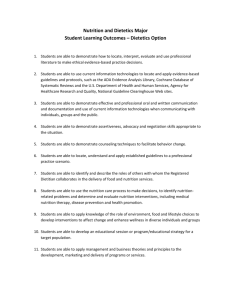
ADA’s Evidence-Based Nutrition Practice Guidelines and Toolkits Kari Kren, MPH, RD, LD Manager, Governance American Dietetic Association November 1, 2006 History of ADA’s MNT Guides 1990’s: Medical Nutrition Therapy Across the Continuum of Care (MNTACC) (research-based) 2001 & 2002: MNT Evidence-Based Guides for Practice Hyperlipidemia, Diabetes Type 1 and 2, Gestational Diabetes, Chronic Kidney Disease 2005 & 2006: Evidence-Based Nutrition Practice Guidelines & Toolkits What’s New? Movement in healthcare towards evidence-based practice More systematic, rigorous process of evidence analysis Use of ADA’s Nutrition Care Process Assessment Diagnosis Intervention Monitoring & Evaluation Guidelines are a free member benefit on the Evidence Analysis Library Toolkits consist of more resources for application of the Guidelines Oversight by Evidence-Based Practice Committee What are Evidence-Based Nutrition Practice Guidelines? Evidence Summaries & Conclusion Statements = what the evidence says Guideline = course of action for the practitioner based on the evidence What are Evidence-Based Nutrition Practice Guidelines? Definition: A series of guiding statements and treatment algorithms which are developed using a systematic process for identifying, analyzing and synthesizing scientific evidence. They are designed to assist practitioner and patient decisions about appropriate nutrition care for specific disease states or conditions in typical settings. Approved by Evidence-Based Practice Committee, 2006 Features of Guidelines Introduction: scope, intent, methods, benefits/harms Recommendations: a series of guiding statements that propose a course of action for practitioners Algorithms: step-by-step flowchart for treatment of the specific disease/condition Appendices: food tables, etc. What are Evidence-Based Toolkits Set of companion documents for application of the practice guideline Disease or condition specific Include: documentation forms outcomes monitoring sheets client education resources case studies MNT protocol for treatment of disease/condition Incorporate Nutrition Care Process as the standard process care Why use these resources? Assist you in: Implementing evidence-based practice Implementing Nutrition Care Process Using recommendations based on a collective body of evidence Training new staff, students and interns Understand treatment for an unfamiliar topic Meeting regulations based on current standards of practice –best practice Current Evidence-Based Guidelines and Toolkits Published on EAL: Disorders of Lipid Metabolism Guideline and Toolkit Adult Weight Management Guideline Critical Illness Guideline Select “Guideline List” From Navigation Bar Select Critical Illness Features of each Recommendation Page Describe “what” and “why” Display rating using AAP adapted scale Strong, Fair, Weak, Consensus, Insufficient Evidence List potential risks/harms for implementing Narrative illustrating the supporting evidence Provide rationale for the recommendation rating Link to supporting evidence Recommendation for Immune-enhancing formula Definition -Risks/Harms -Conditions of Application -Potential Costs -Narrative -Rationale for Rating Recommendation Example • R.5. Blue dye should not be added to EN for detection of aspiration. The risk of using blue dye outweighs any perceived benefit. The presence of blue dye in tracheal secretions is not a sensitive indicator for aspiration. • Strong Imperative • Recommendation Rating • Strong = Practitioners should follow a Strong recommendation unless a clear and compelling rationale for an alternative approach is present. • Imperative = imperative recommendations “require,” or “must,” or “should achieve certain goals,” but do not contain conditional text that would limit their applicability to specified circumstances. Statement Rating Definition Implication for Practice Strong A Strong recommendation means that the workgroup believes that the benefits of the recommended approach clearly exceed the harms (or that the harms clearly exceed the benefits in the case of a strong negative recommendation), and that the quality of the supporting evidence is excellent/good (grade I or II).* In some clearly identified circumstances, strong recommendations may be made based on lesser evidence when high-quality evidence is impossible to obtain and the anticipated benefits strongly outweigh the harms. Practitioners should follow a Strong recommendation unless a clear and compelling rationale for an alternative approach is present. Fair A Fair recommendation means that the workgroup believes that the benefits exceed the harms (or that the harms clearly exceed the benefits in the case of a negative recommendation), but the quality of evidence is not as strong (grade II or III).* In some clearly identified circumstances, recommendations may be made based on lesser evidence when high-quality evidence is impossible to obtain and the anticipated benefits outweigh the harms. Practitioners should generally follow a Fair recommendation but remain alert to new information and be sensitive to patient preferences. Weak A Weak recommendation means that the quality of evidence that exists is suspect or that well-done studies (grade I, II, or III)* show little clear advantage to one approach versus another. Practitioners should be cautious in deciding whether to follow a recommendation classified as Weak, and should exercise judgment and be alert to emerging publications that report evidence. Patient preference should have a substantial influencing role. Consensus A Consensus recommendation means that Expert opinion (grade IV) supports the guideline recommendation even though the available scientific evidence did not present consistent results, or controlled trials were lacking. Practitioners should be flexible in deciding whether to follow a recommendation classified as Consensus, although they may set boundaries on alternatives. Patient preference should have a substantial influencing role. Insufficient Evidence An Insufficient Evidence recommendation means that there is both a lack of pertinent evidence (grade V) * and/or an unclear balance between benefits and harms. Practitioners should feel little constraint in deciding whether to follow a recommendation labeled as Insufficient Evidence and should exercise judgment and be alert to emerging publications that report evidence that clarifies the balance of benefit versus harm. Patient preference should have a substantial influencing role. Drill down as needed Evidence Summary Critical Illness Recommendations Enteral vs. Parenteral Nutrition Timing of Feeding Immune-Enhancing Enteral Formula Feeding Tube Site Blue Dye Use Monitoring Criteria in Critical Care Monitoring Delivery of Energy Blood Glucose Control Energy Expenditure Equipment Patient Condition Environment Test Interpretation Energy Assessment Main Menu: Algorithms Adult Weight Management Algorithms Weight Management Treatment Energy Expenditure Assess Nutritional Status Dietary Interventions Weight Management Treatment Algorithm Assessment Diagnosis Intervention Monitor/Evaluation Select: Determine Diet Intervention Dietary Intervention Algorithm Eating Frequency Portion Control Meal Replacements Nutrition Education Meal Replacements Recommendation Disorders of Lipid Metabolism Toolkit STORE Click here to see sample forms • Choose Quantity • Add to Cart Disorders of Lipid Metabolism Toolkit Contents Summary Page for DLM and DLM with Metabolic Syndrome MNT Flowchart of Encounters MNT Encounter Process Documentation Forms Instructions for Sample Referral Form MNT Sample Referral Form Initial and Follow-up Nutrition Progress Note Sample Case Study #1 Sample Case Study #2 Summary Page for DLM: based on evidence e.g. HDL-C……........…...increase or no change.....>40mg/dL (males), >50mg/dL (females) soluble fiber intake ……….increased intake………. >25g dietary fiber of which 7-13g soluble fiber per day ©2006 American Dietetic Association Disorders of lipid Metabolism Toolkit Encounter Process for Disorders of Lipid Metabolism ENCOUNTER: Initial Encounter 45 to 90 minutes Encounter Process: detailed process for assessment, diagnosis, intervention and monitoring and evaluation of patients with DLM Assessment Obtain the following from client, medical record/information system or clinical referral form within 30 days of encounter. Client History consists of four areas: medication and supplement history, social history, medical/health history, and personal history. •Medication and Supplement History includes, for instance, prescription lipid-lowering, antihypertensive, diabetes, and thyroid medications, over the counter (OTC) drugs, herbal and dietary supplements (for example folate, B-complex vitamins, Co-enzyme Q10, those with potential for food/drug interaction), and illegal drugs. • Social History may include such items as smoking history, alcohol intake (frequency and amount), socioeconomic status, social and medical support, cultural and religious beliefs, housing situation, and social isolation/connection. •Medical/Health History includes chief nutrition complaint, present/past illness particularly of cardiovascular disease, diabetes, thyroid disease, evaluate risk factors for cardiovascular disease, metabolic syndrome, family medical history, especially of premature cardiovascular disease, mental/emotional health and cognitive abilities. •Personal History consists of factors including age, occupation, role in family, and education level. Biochemical Data includes laboratory data, for example, lipid profile, glucose, hemoglobin A1C, liver function tests, thyroid, Lp(a), homocysteine, and high-sensitivity C reactive protein. Anthropometric Measurements include height, weight, weight history, body mass index (BMI), waist circumference (WC), waist to hip ratio (WHR) Physical Exam Findings includes blood pressure, general physical appearance (abdominal girth and presence of xanthomas) muscle and subcutaneous fat wasting, and affect Food and Nutrition History consists of four areas: Food consumption, nutrition and health awareness and management, physical activity and exercise, and food availability Case Studies: • Initial and Follow-up Encounters • Illustrates the Nutrition Care Process • Uses new SL for Nutrition Diagnosis and Intervention DLM Toolkit Contents Client Education Resources Executive Summary and List of ADA Client Education Resources Client Agreement for Care Other Client Education Resources Alcohol Soluble Fiber Tips The Low-down on Trans Fats Health Benefits of Nuts Omega-3 Fatty Acids Sample Menu #1 and #2 Appendices Client Education Materials: 6-7th grade reading level DLM Toolkit Contents Outcomes Monitoring Forms Individual Outcomes Monitoring Form Aggregate Input Form Aggregate Outcomes Monitoring Form Sample Individual Outcomes Form Sample Aggregate Input Form Sample Aggregate Outcomes Form Monitoring Outcomes: use for individuals or a population –monitor change (e.g. kcal, lipid values) • document over several encounters • programmed formulas for % change and averages Upcoming Evidence-Based Guidelines and Toolkits 2006-2007 program year: Adult Weight Management Toolkit Critical Illness Toolkit Pediatric Weight Management Guideline Upcoming guidelines and toolkits: Diabetes Type 1 and 2 Oncology Hypertension Heart Failure Gestational Diabetes Spinal Cord Injury COPD Chronic Kidney Disease Unintended Weight Loss For Further Information: See “Help” tab and FAQs on EAL Or Contact: Kari Kren kkren@eatright.org EAL Help eal@adaevidencelibrary.com Website: www.adaevidencelibrary.com Thank you for your attention! Questions?