12Lec-Malaria
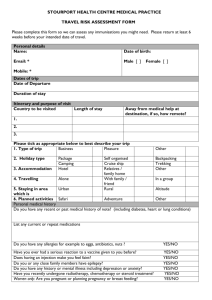
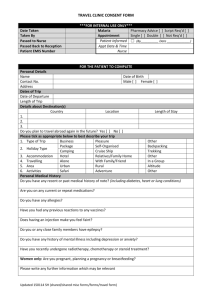
advertisement
PIDSP 19th Annual Convention Taming the beasts: top killers of children - Malaria Dr. Fe Esperanza Espino Research Institute for Tropical Medicine Outline of presentation • • • • • • Local epidemiology Recognition of the disease Diagnosis Evidence-based treatment guidelines Prevention Summary Espino, FE, PIDSP Annual Convention February 2012 LOCAL EPIDEMIOLOGY Espino, FE, PIDSP Annual Convention February 2012 Espino, FE, PIDSP Annual Convention February 2012 Philippine population and malaria mortality rates (1905-’09), malaria morbidity rates (1945-’09) Per 106 Espino, FE, PIDSP Annual Convention February 2012 106 Espino, FE, PIDSP Annual Convention February 2012 Espino, FE, PIDSP PSMIDAnnual AnnualConvention ConventionFebruary November 2012 2011, Manila Philippine malaria statistics (2009) Parameter Population Population at risk for malaria Suspected malaria cases Confirmed malaria cases Malaria deaths (Adapted from WHO, 2010) Espino, FE, PIDSP Annual Convention February 2012 Figures 91, 982,099 6,598,788 (7.2% ) 370,802 19,198 (20.9/100,000 pop’n) 24 (0.02/100,000 pop’n) Espino, FE, PIDSP Annual Convention February 2012 (Modified from Gomes, M., et al, 1994, Bull WHO Espino, FE, PIDSP Annual Convention February 2012 Espino, FE, PIDSP Annual Convention February 2012 Malaria species by age group, Palawan, Philippines (2006 - ’10) (Malaria Program, Dept. of Health) Age group (%) P. falciparum P. vivax (%) (%) P. malariae Mixed Pf/Pv Total <2 1,597 (5.2) (64.6) 835 (7.5) (33.8) 20 22 2,474 2 to < 5 4,101 (13.3) (76.9) 1,124 (10.1) (21.1) 77 32 5,334 5 to 9 6,476 (21.0) (73.1) 2,229 (20.0) (25.2) 55 99 8,859 10 to 14 5,213 (16.9) (73.3) 1,791 (16.1) (25.2) 68 38 7,110 15 to <30 7,124 (23.1) (70.8) 2,771 (24.9) (27.5) 115 49 10,059 > 30 6,319 (20.5) (71.2) 2,400 (21.5) (27.0) 112 50 8,881 30,830 (72.2) 11,150 (26.1) 447 290 42,717 Total (% species) Espino, FE, PIDSP Annual Convention February 2012 Species reservoir by age group, Palawan (2005-10)* (Malaria Study Group, RITM) P. falciparum P. vivax (% total) (% total) <2 2 (2) 0 0 0 102 2 to < 5 8 (2) 8 (2) 0 0 328 5 to 9 35 (7) 11 (2) 3 0 514 10 to 14 21 (7) 14 (4) 1 1 315 15 to <30 24 (6) 9 (2) 2 0 411 > 30 25 (3) 11 (1) 0 3 755 115 (5) 53 6 4 2,425 Age group Total (% species) *Community surveys; those with ages available Espino, FE, PIDSP Annual Convention February 2012 P. malariae P. knowlesi Total slides Severe malaria by species and age group, Philippines (2006-’10) (Malaria Program, Dept. of Health) Age groups (years) P. falciparum (%) P. vivax Mixed infections Total by age group (%) 0-4 21 (25.9) 3 0 25 (25.5) 5-9 7 (8.6) 2 1 10 (10.2) 10-14 8 (9.9) 0 0 8 (8.16) >15 45 (55.6) 9 1 56 (57.1) Total by species 81 (82.7) 14 3 98 Espino, FE, PIDSP Annual Convention February 2012 1000 Rainfall (mm) Rainfall Per 1000 population (in log) 10 Malaria vector (MBR) 800 600 1 400 200 0 0.1 Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Jan Figure 4.5. Mean monthly rainfall, and mean monthly malaria incidence (per 1,000 population), 1988 - 1996, and man-biting rates ofAn. flavirostris, January 1992 to January 1993 (modified from Torres et. al , 1997) Espino, FE, PIDSP Annual Convention February 2012 Monthly malaria cases and rainfall, Morong, Bataan, 1981 to 1997. 400 Malaria cases Rainfall Rainfall in mm./mo, No. of malaria cases 300 200 100 0 '81 '82 '83 '84 '85 '86 Espino, FE, PIDSP Annual Convention February 2012 '87 '88 '89 '90 '91 '92 '93 '94 '95 '96 '97 (From Brooker, S. et al. (2007), Am.J.Trop.Med.Hyg., 77(Suppl. 6) Espino, FE, PIDSP Annual Convention February 2012 61.5% 4.1% 30.9% 3.9% Pre-school (n=460) 19.1% 27.8% 17.9% 35.2% 68.5% 21.1% 6.0% School-age (n=392) Relationship between plasmodia-hookworm co-infection mean [Hb], Kenya based on re-analysis of published data (modified from Brooker, S. et al. (2007), Am.J.Trop.Med.Hyg., 77(Suppl. 6) Espino, FE, PIDSP Annual Convention February 2012 Pregnant women (n=251) 4.4% • Morphologically similar to P malariae; may be mistaken to be P falciparum • In Rhesus monkey studies – High parasite densities is possible – No significant sequestration in microcirculation • In humans – Reported in children and relatively older adults – May present as a mild from of malaria easily responding to chloroquine but may also be severe and fatal – Fever, headaches, intermittent chills, abdominal pain, sweating and malaise Espino, FE, PIDSP Annual Convention February 2012 RECOGNITION AND DIAGNOSIS Espino, FE, PIDSP Annual Convention February 2012 Could this be malaria? Fever and headache Fever, severe chills and sweats, severe headache Fever, backache, joint pains Fever, abdominal pain, jaundice, thrombocytopenia, anemia Could also be Dengue Typhoid fever Viral hepatitis Fever of unknown origin Ask for Residence History of travel History of blood transfusion Espino, FE, PIDSP Annual Convention February 2012 Diagnostic options before and now Clinical algorithm Fever Thick and thin malaria blood film NO YES Rural health unit Non-microscopic rapid diagnostic tests (RDTs) YES Danger signs Of malaria NO NO Provide chloroquine (Modified from Gomes, M., et al, 1994, Bull WHO and ADS-MCP Project Reports, 1997-2002) Espino, FE, PIDSP Annual Convention February 2012 Make malaria Blood film Amplification of specific nucleic acid sequences (PCR) Malaria RDTs Antigens detected by Malaria RDTs • HRP-2 – histidine-rich protein produced by asexual stages of P. falciparum • pLDH – parasite lactatedehydrogenase antigen produced by asexual and gametocytes of all human Plasmodium species • Aldolase – enzyme in the glycolysis pathway of Plasmodium Espino, FE, PIDSP Annual Convention February 2012 From Malaria Rapid Diagnostic Test Performance – results of WHO product testing Of malaria RDTs Round 1 (2008) WHO recommendations for malaria RDTs • Results should be at least as accurate as results derived from microscopy performed by an average (trained) microscopist • Minimum detectable parasite count by a proficient microscopist is 10 parasites/ul blood • Sensitivity – 95% compared to microscopy – Detection of parasitemia of 100 parasites per ul blood* (or 0.002% parasitemia) Espino, FE, PIDSP Annual Convention February 2012 Espino, FE, PIDSP Annual Convention February 2012 EVIDENCE-BASED TREATMENT GUIDELINES Espino, FE, PIDSP Annual Convention February 2012 Currently available antimalarial drugs •Chloroquine •Sulfadoxine/ Pyrimethamine •Quinine •Mefloquine ARTEMISININ COMBINED THERAPY (ACTs) •Artemetherlumefantrine (Coartem) •Artemisinin-piperaquine •Dihydroartemisinin-piperaquinr •Artesunate – mefloquine •Atovaquone – Chloroguanide •Artesunate-pyronaridine •Antibiotics •Artesunate - amodiaquine •Artesunate -sulfadoxine/ pyrimethamine Primaquine Espino, FE, PIDSP Annual Convention February 2012 Espino, FE, PIDSP Annual Convention February 2012 Coker RJ, et al., 2011; www.thelancet.com; 377:599-609 Monitoring drug resistance • THERAPEUTIC EFFICACY SURVEILLANCE or TES – Standardized protocols developed by WHO wherein response is classified using clinical and parasitological criteria – Gold standard for treatment guidelines – Limited by host immunity, prior treatment with antimalarials, and drug pharmacokinetics/dynamics. • IN VITRO TESTS – Parasites are allowed to mature in microplates pre-dosed with differing dilutions of antimalarial drug – These tests provide baseline data and trends; forecast; precede in vivo resistance – HRP2 or pLDH, enzymes produced by the parasite can also be measured • MOLECULAR MARKERS of drug resistance – P. falciparum – Chloroquine (pfcrt76), sulfadoxine (dhfr51, dhfr59, dhfr108), and pyrimethamine (dhps436, dhps437, and dhps540), – Provide baseline data and trends – Correlation between mutations and in vivo/in vitro data Espino, FE, PIDSP Annual Convention February 2012 TES categories of response to treatment (blood schizonticides) Falciparum malaria • • • Vivax malaria Adequate clinico-parasitological response (ACPR) Early treatment failure (ETF) – Days 0 - 3 Late treatment failure (LTF) – Days 4 – 28 – Clinico-parasitological failure – Parasitological failure • Adequate response • Treatment failure • Parasitemia and fever from Day 3 to Day 28 after start of treatment • Parasitaemia from Day 7 to 28 after start of treatment regardless of clinical condition 30000 25000 20000 Parasite count Parasite count 25000 20000 15000 10000 15000 10000 5000 5000 0 0 0 1 2 3 4 7 14 21 28 Day after start of treatment Adequate Early tx failure Espino, FE, PIDSP Annual Convention February 2012 0 1 2 3 4 7 14 21 Day after start of treatment Late tx failure Adequate Treatment failure 28 Summary of TES late 1990s to 2011 Drug/ drug combination Provinces Years Chloroquine (Cq) Apayao, Agusan del Sur, Compostela Valley Late 1990s – 2002 Sulfadoxine/ pyrimethamine (SP) Agusan del Sur, Apayao, Kalinga Agusan del Sur, Compostela Valley Cq+SP Falciparum malaria 2002-07 Davao del Sur, Sultan Kudarat 2003-07 CARAGA 2005-06 Compostela valley 2001-02 Isabela Kalinga Coartem (artemether/ lumefantrine) 2001-02 Palawan 2002-03 2005-06 Davao del Sur Sultan Kudarat 2006-07 Zamboanga city Vivax Malaria Chloroquine Primaquine (Pq) Espino, FE, PIDSP Annual Convention February 2012 Palawan/Tawi-Tawi 2011-12? CARAGA 2005-06 Tawi-Tawi 2012? Palawan 2009 – 2011; 2012? Changing treatment guidelines for uncomplicated falciparum malaria based on TES Year < 2002 Malaria treatment level 2002-08 2009-? Firstline Chloroquine (CQ) CQ+SP Coartem Secondline Sulfadoxine/ pyrimethamine (SP) Coartem QN plus, oral Thirdline Quinine (QN) oral Severe Quinine parenteral QN plus (clindamycin or tetracycline or doxycycline) Espino, FE, PIDSP Annual Convention February 2012 QN plus Treatment regimen for uncomplicated falciparum malaria Day 0 – 2 Artemether (20mg)/ lumefantrine (120 mg) 34 kg 25 to 34 kg 15 to 24 kg 5 to 14 kg Day 0 4 tabs 3 tabs 2 tabs 1 tab 8 hrs later 4 tabs 3 tabs 2 tabs 1 tab Day 1 4 tabs BID 3 tabs BID 2 tabs BID 1 tab BID Day 2 4 tabs BID 3 tabs BID 2 tabs BID 1 tab BID Day 3 – Adults Above 12 years 7 to 11 years old 4 to 6 years old 1 to 3 years old Below 1 year 3 tabs 3 tabs 2 tabs 1 tab ½ tab Contraindicated Primaquine (26.3 mg or 15 mg base tablet; 0.75mg/ kg single dose) Espino, FE, PIDSP Annual Convention February 2012 Treatment regimen for uncomplicated vivax malaria Day of treatment • Drug 0 and 1 Chloroquine 150 mg base tablet; 10 mg/kg/day 2 Chloroquine 150 mg base tablet; 5 mg/kg 3 to 17 • Dose (no. of tablets) Primaquine 15 mg base tablet; 0.5 mg/kg/day Adult Four tablets once a day for Days 0 and 1 Two tablets One tablet each day Children 0-11 mos 1-3 years 4-6 years 7-11 years 12-15 years >16 years ½ 1 1½ 2 3 4 Half the above dose per age group Below 1 year 1-3 years 4-6 years 7-11 years > 12 years Contra- indicated 1/3 ½ ¾ 1 In mild-to-moderate G6PD deficiency, primaquine 0.75 mg base/kg body weight given once a week for 8 weeks. In severe G6PD deficiency, primaquine is contraindicated and should not be used. Espino, FE, PIDSP Annual Convention February 2012 Plasmodium vivax relapses • Are important sources of reinfection and transmission • Relapses can occur weeks to years after the initial infection • Risk of relapse of tropical strains is higher than temperate strains • Primaquine is the only commercially available antirelapse drug Risk of P. vivax relapse by primaquine dose (in India, Thailand and Brazil) Dose Odds ratio (adjusted) 0 1.0 75 0.42 0.34-0.52 210 0.22 0.16-0.30 315 0.01 0.00-0.08 420 0.05 0.01-0.20 95% CI (modified from Goller et al., 2007, Amer Jour Trop Med Hyg, Vol 76 No. 2) Espino, FE, PIDSP Annual Convention February 2012 Drug (2009 – ongoing) Duration of ff-up Recurence of parasitemia (%) Chloroquine 4 wks* 1/119 (0.8) Primaquine 6 mos 17/95 (17.9) Drug (2005) Duration of ff-up Recurence of parasitemia (%) Chloroquine 4 wks 0/37 *Days 7, 14, 21 and 28. Espino, FE, PIDSP Annual Convention February 2012 Implications? 1. Primaquine dose increased to 30 mg 2. G-6-PD deficiency – Estimations of prevalence • 5.5% in malaria endemic areas in the Philippines(Salazar NP, et al., 1987) • 1.9% Philippine Newborn Screening Program (Silao CLT, et al., 2009) • 2011- Palawan – ongoing survey among high school students – Point-of-care issues • Screening in malaria endemic areas • Confirmation in nearest tertiary hospital with proper equipment and trained staff Espino, FE, PIDSP Annual Convention February 2012 PREVENTION Espino, FE, PIDSP Annual Convention February 2012 Malaria vaccines Goal Reduce disease severity and death Goal Target population Block infection of liver Non-immune travelers in low transmission areas Block emergence from liver or RBC infection Children and pregnant women in high transmission areas Goal Target population Target population Children and pregnant women in high transmission areas In Africa AMA 1 –based vaccine – Phase I and II RTS,S - Phase III Espino, FE, PIDSP Annual Convention February 2012 Prevent transmission Endemic communities Together with blood-stage vaccines, limit spread of vaccine resistance Any population and situation OTHER ISSUES Espino, FE, PIDSP Annual Convention February 2012 Provinces declared malaria-free Aklan Guimaras Albay Iloilo Batangas Leyte Benguet Marinduque Biliran Masbate Bohol No. Samar Camiguin Siquijor Capiz Sorsogon Catanduanes So. Leyte Cavite Surigao del Norte Cebu Western Samar Ea. Samar Espino, FE, PIDSP Annual Convention February 2012 Urban and semi-urban areas where malaria reported • Antipolo • Fairview • Taytay, Rizal Cawag village, Subic, Zambales, 2006 and 2009 2006 Malaria cases 1999 to 2010 450 400 No. cases 350 300 250 200 150 100 2009 50 0 99 00 01 02 03 04 Year Espino, FE, PIDSP Annual Convention February 2012 05 06 07 08 09 10 People at risk for malaria People living in malaria endemic areas http://www.pbase.com/tconelly/rural_ philippines&page=4 Espino, FE, PIDSP Annual Convention February 2012 Travelers, overseas contract workers Summary • Malaria is still a parasitic disease of public health importance in the Philippines • Epidemiology of malaria in the Philippines is changing – Response to treatment (drug resistance) – Control of relapse – New species in humans • Responsibilities of clinicians and public health physicians: – Suspected malaria cases must be confirmed (especially species) – Response to treatment (including anti-relapse treatment) must be monitored during and after treatment – Malaria cases (and response to treatment) must be reported Espino, FE, PIDSP Annual Convention February 2012 Acknowledgement Malaria Study Group, RITM Sponsors • • • • • • • • • Asia Pacific Malaria Elimination Network (APMEN) AusAID Embassy of France GFTAM Pilipinas Shell Foundation, Inc. Roll Back Malaria USAID WHO (WPRO and WR Office) Others Institutional Partners • • • • • • Malaria Program, Dept. Health, Manila CHD Offices, ARMM UP Manila and UP NIH Pilipinas Shell Foundation, Inc. University of Queensland Others Community Partners Agusan del Sur, Agusan del Norte, Apayao, Davao del Sur, Compostela Valley, Isabela, Kalinga, Palawan, Sultan Kudarat, Surigao del Sur, Surigao del Norte, Zamboanga City, Others