PowerPoint
advertisement

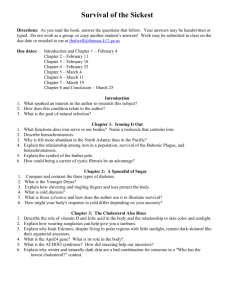
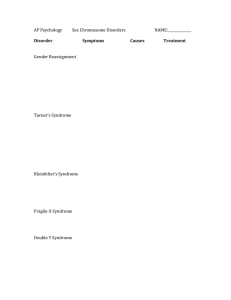
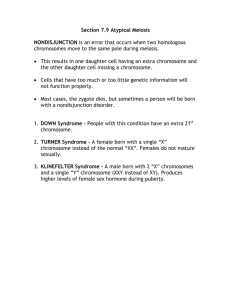
Medical Genetics Robert F. Waters, Ph.D. Pathology, Etiology, Pathogenesis, Pathophysiology Aneuploidy Metabolic Mutations Adducts Porphyrias Produced mainly in: Porphyrin Rings – Liver – Erythrocyte producing cells of bone marrow Not mature erythrocytes (lack of mitochondria) Initial step and last three steps are in the mitochondria Glycine and Succinyl CoA are precursors Hemin is feedback inhibitor of -aminolevulinic dehydrase (ALA) ( -delta) – Lead is inhibitor of this pathway Porphyrin Uses Cytochromes – P450, b5, ETS Hemoglobin Porphyrins Cont: Addition of ferrous iron in mitochondria – ferrochelatase Porphyrias Usually hereditary porphyrin production defects General Classification – Erythropoietic (defect in RBCs) – Hepatic (Defect in liver) Usually autosomal dominant Heme Degradation First product is biliverdin (open ring) – Heme oxygenase Biliverdin plus CO yields bilirubin – Biliverdin reductase NADP Bilirubin – Gut (microbial enzymes act on bilirubin) Produce Urobilinogen – Absorbed and carried to liver to produce Urobilin Yellow color – Large intestine further microbial enzymes produce Stercobilin Characteristic brown color – Liver Conjugation with 2 moles of glucuronic acid – Glucuronyl bilirubin transferase – Forms bilirubin diglucuronide (polar and soluble) detox Hemoglobin Porphyrin ring Iron Oxygen Binding Two alpha chains and two beta chains – 1 2 1 2 Thalassemias Structure of Hemoglobin Thalassemias and types Alpha Thalassemias Thalassemias-Cont: Alpha thalassemia usually more severe – Thalassemia major – Variety of deletions (usually) Beta thalassemia usually less severe – Thalassemia minor – Usually single nucleotide substitutions Thalassemia Tx Red Blood Cell Transfusions Chelation Hemoglobinopathies-Cont: Thalassemias (thalassa-sea:many cases around Mediterranian Sea) – + 0 (some production vs. none) – + 0(some production vs. none) Alpha thalassemias affect fetal and postpartum hemoglobin Beta thalassemias affect only postpartum Genetics of Hemoglobin 12 – Chromosome 16 Diploid designation 12/12 – Produced in utero 1 2 – Chromosome 11 – Produced postpartum only Alpha-like chains () – pre- & post-natal – (zeta) Beta-like chains () – Essentially post-natal – (sigma, epsilon, gamma) Hemoglobinopathies Very common AR-Sickle Cell Anemia – HbA vs HbS (6 GluVal) Life long hemolytic anemia Sickle Cell Anemia (AR) Sickle cell anemia is the most common inherited blood disorder in the United States, affecting about 1 in 500 African Americans. SCA is characterized by episodes of pain, chronic hemolytic anemia and severe infections, usually beginning in early childhood. Autosomal recessive disease caused by a point mutation in the hemoglobin beta gene (HBB) found on chromosome 11p15.5. called HbS. Though, as yet, there is no cure for SCA, a combination of fluids, painkillers, antibiotics and transfusions are used to treat symptoms and complications. Hydroxyurea, an antitumor drug, has been shown to be effective in preventing painful crises. Hydroxyurea induces the formation of fetal Hb (HbF)—a Hb normally found in the fetus or newborn—which, when present in individuals with SCA, prevents sickling. Other HbS Anemia Tx Vaso-occlusive treatments Folic acid and penicillin Hydroxyurea Bone marrow transplants Sickle Cell Cont: HbS Renal Failure Iron and Iron Storage Diseases Association with copper – Absorption from lumen in intestine Ceruloplasmin – Cupric to cuprous, ferrous to ferric – Vitamin C – Wilson’s disease 1:100,000 – Lack of copper transport proteins Copper in Enzymes Iron Contained in…. Some Examples Hemoglobin, myoglobin NO binding, guanylate cyclase ETS hemes Cytochrome b5 in desaturation Iron-sulfur (Complex I, aconitase, xanthine oxidase, ferrochelatase (heme synth.) Phenylalaine hydroxylase, tyrosine hydroxylase, dioxygenases Etc. Transferrin Plasma protein – Glycoprotein synthesized by liver – Single polypeptide (~700 AA’s) High affinity for ferric iron No affinity for ferrous iron Serum levels about 30umol/L – Serum has excess iron binding capacity Transferrin Cont: Transferrin production increased during – Iron deficiency – Pregnancy (high estrogen levels) – Women taking oral contraceptives Transferrin production decreased – – – – – Excess iron Infection Inflammation Neoplasia Protein catabolic state Transferred to recipient cells by– Transferrin-binding Receptors Ferritin Store iron in ferrous non-toxic state Relatively short term storage Handoff to/from transferrin Handoff to/from hemosiderin Mainly intracellular – Not usually in the serum unless iron storage saturation Hemosiderin Long term storage Handoff to/from ferritin Exist in times of iron overload Probably a form of iron-ferritin complexes in a type of micelle formation in tissues Hypochromic Microcytic Anemia Pale RBCs due to low levels of hemoglobin Hemochromatosis (AR) Excess iron (free iron due to saturation of tranferrin) Arthritis, liver cancer, coronary occlusions Early diagnosis and treatment AR inheritance with gene on chromosome 6 Treatment – Venesection (removal of blood) Removal of 500ml of blood over specified frequency and period of time to lower iron reserves High frequency is 500ml per week over 1-2 year period of time – Chelation Hereditary Hemochromatosis What are the symptoms of hemochromatosis? Joint pain is the most common complaint of people with hemochromatosis. Other common symptoms include fatigue, lack of energy, abdominal pain, loss of sex drive, and heart problems. However, many people have no symptoms when they are diagnosed. If the disease is not detected and treated early, iron may accumulate in body tissues and eventually lead to serious problems such as… arthritis liver disease, including an enlarged liver, cirrhosis, cancer, and liver failure damage to the pancreas, possibly causing diabetes heart abnormalities, such as irregular heart rhythms or congestive heart failure impotence early menopause abnormal pigmentation of the skin, making it look gray or bronze thyroid deficiency damage to the adrenal glands Hemochromatosis Dx Blood tests can determine whether the amount of iron stored in the body is too high. The transferrin saturation test reveals how much iron is bound to the protein that carries iron in the blood. Transferrin saturation values higher than 45 percent are considered too high. The total iron binding capacity test measures how well your blood can transport iron, and the serum ferritin test shows the level of iron in the liver. If either of these tests shows higher than normal levels of iron in the body, doctors can order a special blood test to detect the HFE mutation, which will confirm the diagnosis. A liver biopsy may be needed, in which case a tiny piece of liver tissue is removed and examined with a microscope. Hemochromatosis Tx Phlebotomy Should be more dietary resolution Alpha-1-Antitrypsin Deficiency (AR) Alpha-1 antitrypsin deficiency (Alpha-1) is a hereditary genetic disorder which may lead to the development of lung and/or liver disease. It is the most common genetic cause of liver disease in children. Adults can also be affected by Alpha-1 and may develop lung conditions such as emphysema as well as liver problems. Fortunately, many persons diagnosed with Alpha-1 never develop any of the associated diseases. Alpha-1-Continued Liver Cancer COPD Latent manifestation Tx – Steroids – Herbs???? Albinism-Lack of Melanin Pigment Tyrosine production Tyrosine transport Autism Insistence on sameness; resistance to change Difficulty in expressing needs; using gestures or pointing instead of words Repeating words or phrases in place of normal, responsive language Laughing (and/or crying) for no apparent reason; showing distress for reasons not apparent to others Preference to being alone; aloof manner Tantrums Difficulty in mixing with others Not wanting to cuddle or be cuddled Little or no eye contact Unresponsive to normal teaching methods Sustained odd play Spinning objects Obsessive attachment to objects Apparent over-sensitivity or under-sensitivity to pain No real fears of danger Noticeable physical over-activity or extreme under-activity Uneven gross/fine motor skills Non-responsive to verbal cues; acts as if deaf, although hearing tests are in normal range Carnitine Deficiency Muscle metabolism is impaired, causing myopathy, hypoglycemia, or cardiomyopathy. Most often, treatment consists of dietary Lcarnitine, avoid strenuous exercise, avoid fasting. G6PD Deficiency (XR) Partial protection against malaria??? X-Linked Recessive Favism (Fava Beans) Insufficient formation of NADPH – High oxidative stress in erythrocytes – Lipid metabolism affected Phenylketonuria Lack of tyrosine production Form neurotoxic phenylketones – Phenylalanine dehydrogenase Feed with tyrosine – T3, T4 thyroxines – L-Dopa – Dopamine – Epinephrine – Melanin Pigment, etc. Galactosemia Problems with speech, language, hearing, fine-motor coordination, hemorrhage of the gel-like substance of the eye, tremors, stunted growth, and certain learning disabilities. Types associated with galactose kinase and galactose-1-phosphate uridyl transferase Klinefelter syndrome (XXY syndrome) Some affected boys will have more features of the syndrome than others and there will be a difference in the degree of severity In some cases, a diagnosis of XXY syndrome is not made until a boy approaches puberty and some men may never be diagnosed with the condition The most common features include learning difficulties and a tendency to grow at a slightly quicker rate than their peers so that their final height may be more than expected, but is usually within the normal range; reduction in body hair, beard growth and testicular size that can be treated with the male hormone testosterone; while sexuality is normal men with the syndrome may be infertile Having a son with XXY syndrome does not appear to be related to either the age of the mother or the father at the time of conception Those with 47,XXY in all their cells usually are infertile Turner Syndrome XO The victim in question possesses a genetic structure in which one or many parts of the X chromosome remains absent in the cell formation. Symptoms – – – – – – – Small fingernails Horseshoe shaped kidney Low Hairline Poor body development Increased weight Absence of a menstrual cycle, and Sterility of the reproductive organs. Down’s Syndrome Triplo-21 The reasons for this disease are known Types – a)Trisomy 21: In most cases (95%), all the body cells of the patient have three chromosomes 21, which happens due to the meiosis non-disjunction. – b)Mosaic Down Syndrome: Only some body cells have an extra chromosome 21 (non disjunction in mitosis). – c)Translocation Down Syndrome: In this case, a part of chromosome 21 is attached to another chromosome. So the patients have 2 chromosomes 21 plus a part of a third chromosome 21. Down’s Continued The level of superoxide disimutase-1, which is coded by a gene on chromosome 21, is on average, 150% of the values found in normal individuals’ blood as well as other cells. The high enzyme activity results in a high rate of conversion of superoxides to peroxides, resulting in high levels of peroxides that may damage DNA and lipids. Over expression of lymphocyte function associated antigen-1(LFA1), which is also coded on chromosome 21, may lead to an abnormal interaction between cells from the thymus, resulting in aberrant T-cell maturation and selection. Overexpression of the interferon receptor gene also located on chromosome 21 is common in Down syndrome and may also contribute to immune deficiency. Low serum zinc common in Down syndrome, may also cause weak immunity. Down’s Continued The most significant abnormality of the immune system in Down syndrome is a 30-fold increase in the incidence of acute leukemia 200-fold increase in acute megakaryocytic leukemia. 30% of adults with Down syndrome are deficient in IgG-2 and/or IgG-4 and these deficiencies are also common in children with Down syndrome. ---selenium supplementation may increase Cystic Fibrosis (AR) Sinus Infections Poor Growth Diarrhea Infertility Difficulty breathing Hemophilia (XR) Deep internal bleeding Joint damage Transfusion transmitted infection Poor reactions which can result from the treatment of the clotting factor Intracranial hemorrhage Klinefelter’s Syndrome XXY, XXXY Symptoms – – – – – The most important symptom is the male infertility. small testes inability to produce sperms rounded body type difficulties in reading, writing, or even language problems Tx – Testosterone (Early) Urea Cycle Disorders Examples – Argininemia – Citrullinemia – Argininosuccinic aciduria Symptoms – Clinical features are the result of the development of hyperammonemia – encephalopathy and include poor feeding, – lethargy leading to coma – Hyperventilation – muscle tone abnormalities and, – death. Spina bifida Folate (folic acid) DEGRADES BY COOKING! Folate occurs naturally in food. Cereals, baked goods, leafy vegetables (spinach, broccoli, lettuce), okra, asparagus, fruits (bananas, melons, lemons), legumes, yeast, mushrooms, organ meat (beef liver, kidney), orange juice, and tomato juice. Alzheimer's, Parkinson’s and Dementia Curcuminoids Turmeric Glutathione Tay-Sachs Disease lethal genetic disorder Mutation lies in the gene Hex A --hexaminidase A on Chromosome 15 The most important ganglioside for Tay-Sachs is the Ganglioside GM2. This material is found in the nerve cells of the brain and especially in the cell membranes. In the case of Tay-Sachs Disease there is no enough activity of the enzyme and the gangliosides are accumulated with destructive results. The accumulation of GM2 in the nervous tissue causes a gradual destruction of the nervous system. The apparently healthy baby gradually stops laughing, crawling, smiling, grasping, turning around. Later people with Tay-Sachs becomes blind and paralyzed and unable to shallow and contact with its surrounding. One of the most common symptom is a red spot in the eyes. The death seems to be fatal (in the classic Tay-Sachs Disease) and comes around age of 5. Tay-Sachs Inheritance (AR) Amyotrophic Lateral Sclerosis Lou Gehrig’s disease also known as familial amyotrophic lateral sclerosis (ALS) ISIS-SOD1Rx is an antisense drug designed to inhibit the production of SOD1. ALS Continued Muscles in the body are damaged first Speech problems Problems with moving, swallowing (dysphagia), and speaking or forming words (dysarthria) Exaggerated reflexes (hyperreflexia) including an overactive gag reflex Does not affect cognitive abilities, patients are aware of their progressive loss of function and may become anxious and depressed. Eventually lose the ability to breathe on their own and must depend on ventilatory support for survival GILBERT’S SYNDROME Alagille syndrome Often affects the liver and other organs, including the heart, eyes, spine and kidneys. Jaundice, usually present at birth (yellowing of the skin) Severe itching (caused by the buildup of bile salt in the body) Pale, loose or clay-colored stools (this happens because there is little or no bile reaching the intestine to color the bowel movements) Poor weight gain (due to a lack of bile needed to digest and absorb fat) Poor growth Marfan’s Syndrome Bones (arms, legs, fingers, and toes) that are longer than normal A long, narrow face Crowded teeth because the roof of the mouth is arched A breastbone that sticks out or caves in A curved backbone Flat feet Nearsightedness Glaucoma (high pressure within the eye) at a young age Cataracts (the eye’s lens becomes cloudy) A shift in one or both lenses of the eye A detached retina in the eye Stiff air sacs in the lungs. A collapsed lung if the air sacs become stretched or swollen Snoring or not breathing for short periods (called sleep apnea) while sleeping Inborn Errors of Metabolism Enzymatic defect (structure) Enzyme substrate problem Enzyme co-enzyme malfunction Enzyme co-factor (metal) malfunction Build up before—feed after Usually autosomal recessive – Otherwise would probably be lethal Some are hemizygous (XY) Consequences-Overview Accumulation of a precursor – Accumulated precursor may be toxic E.g., pyruvate – Alternate minor pathways may start producing other toxic metabolites E.g., PKU Deficiency of product – Product may be precursor to other substance. E.g., tyrosine and thyronines – Feedback inhibition may be impaired due to lack of product Causes lack of feedback inhibition PDH Complex Build up of lactate and pyruvate May be E1, E2, E3 lesion Also affects alphaketoglutarate dehydrogenase Cystinuria Increased secretion of cystine, lysine, arginine, ornithine Aminoaciduria AR (variable expressivity) Renal failure Glycogen storage diseases Type I (von Gierke’s) – Hepatomegaly, mental retardation, hypoglycemia – Glucose-6-phosphatase deficiency – AR Type VIII (Glycogen Storage Disease) – Hepatomegaly,mild acidosis, hypoglycemia – XR – Phorphorylase kinase McArdle’s Disease Type V – myophosphorylase C deficiency – AR difficulty during physical activities like jogging, walking up hills or stairs, swimming, or anything moderately intense Tay-Sachs Disease Onset at 4 to 6 months Death 2 to 4 years AR Degenerative neurological changes – Gangliosidosis Reduced hexosaminidase Hartnup Disease Tryptophan transport Neurological change AR Homocystinuria Dislocated lenses AR Accumulation of methionine and homocystine Lesch-Nyhan Syndrome Uric Aciduria Self-mutilation Mental retardation Cerebral palsy XR Mucopolysaccharidoses I Hurler’s Syndrome “Gargoyle” Appearance Mental retardation Corneal clouding Cardiovascular degeneration Dwarfism Mucopolysaccharide accumulation Mucopolysaccharidoses II Hunter’s Syndrome – Less severe than Hurler’s – No evidence of corneal clouding Pentosuria AR “False Diabetes” Congenital Spherocytosis Episodes of hemolytic anemia Defect in RBC membrane AD – Patients are heterozygous Wilson’s Disease Cirrhosis of liver Neurological damage Improper copper metabolism AR Build up of stored copper Decreased serum levels of ceruloplasmin Treatment by Penicillamine removes stored Cu Maple Syrup Urine Disease BCAA dehydrogenase Alcaptonuria Dark Urine Disease Homogentisic acid AR Vitamin Pathways holoenzyme carboxylase – pyruvate carboxylase CoA NAD FAD, FMN Huntington's disease AD Chorea Latent gene Neurodegenerative disease – The neuron in the center (yellow) contains an abnormal intracellular accumulation of huntingtin called an inclusion body (orange). Duchenne Muscular Dystrophy DMD XR Muscle deterioration early in life Muscles eventually “explode” Fatigue Mental retardation (possible, but does not worsen over time) Muscle weakness Progressive difficulty walking – May be lost by age 12 (Myotonic) Muscular Dystrophy (MD) fat and connective tissue often replace muscle fibers Steinert's disease AD Many other types of inherited muscular dystrophy TYPE I Diabetes Diabetic Ketoacidosis (DKA) Beta cell destruction or deterioration Juvenile onset Type II Diabetes Chromosome I and IV Vasculitis NIDDM to IDDM Systemic Lupus Erythematosus (SLE or Lupus) Autoimmune disease DNase1 deficiency – normally eliminates what is called "garbage DNA" and other cellular debris by chopping them into tiny fragments for easier disposal. Rashes Infection Pain…especially joint pain