Review: Osteoporosis
advertisement

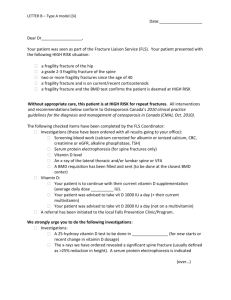
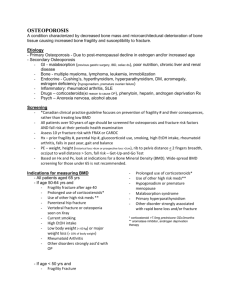
Review: Osteoporosis Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, UOttawa Twitter: @RolandHalil July, 2015 Objectives 8.3 Osteoporosis • Define osteoporosis and list risk factors for osteoporotic fracture • Screen for osteoporosis or reduced bone density appropriately according to age, sex and risk factors. • Manage osteoporosis and osteopenia effectively and according to guidelines including lifestyle advice (including exercise and diet), and medications where appropriate. Resources • 2010 Osteoporosis Clinical Guidelines - Osteoporosis Canada – http://www.osteoporosis.ca/health-care-professionals/guidelines/ – http://www.cmaj.ca/content/early/2010/10/12/cmaj.100771.full.pdf+html • 2013 Appraisal of the 2010 Clinical Practice Guideline for the Diagnosis and Management of Osteoporosis in Canada; – Canadian Task Force on Preventive Health Care (CTFPHC) – http://canadiantaskforce.ca/appraised-guidelines/2013-osteoporosis/ • 2014 Clinician’s guide to prevention and treatment of osteoporosis; – National Osteoporosis Foundation. 2014 Issue, Version 1; – http://nof.org/files/nof/public/content/file/2791/upload/919.pdf Osteoporosis • Goals of Therapy – Prevention – Detection – Treatment Osteoporosis • The most common bone disease in humans • Characterized by: – Low bone mass – Deterioration of bone tissue – Disruption of bone architecture – Compromised bone strength – Increase fracture risk Osteoporosis • WHO diagnostic classification: – BMD T score < 2.5 at the hip or lumbar spine • (T-score = standard deviations below the mean BMD of a young-adult reference population) • (Z-score = standard deviations below the mean BMD of an age-, sex- and ethnicity-matched reference population) • The risk of fractures is highest in those with the lowest BMD; BUT: – …the majority of fractures occur in patients with “low bone mass” rather than “osteoporosis”, due to the large number of patients in this range • Lifetime osteoporosis-related fracture risk: – Caucasian women: 1 in 2 • N.B. Among women the annual incidence of osteoporotic fracture is more than twice that of heart attack, stroke and breast cancer combined – Men: 1 in 5 Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville (MD): Office of the Surgeon General (US); 2004. Available from: http://www.ncbi.nlm.nih.gov/books/NBK45513/ Osteoporosis Burden of disease • Fragility fractures are responsible for excess mortality, morbidity, chronic pain, admission to institutions and economic costs. – Causes 80% of all fractures in menopausal women >50 y.o. – Increased morbidity & mortality post-fracture • • • • Hip fractures: 8.4% to 36% excess mortality within 1 year Hip fractures: 2.5x increased risk of future fractures Vertebral fractures: 5x increase in 2nd vertebral fracture Vertebral fractures: 2x-3x increase in fracture at other sites • N.B. Osteoporosis is less frequent in African Americans, but those with osteoporosis have the same elevated fracture risk as Caucasians Osteoporosis Burden of disease • Post-fracture mortality and institutionalization rates: – Higher for men than women. – ~ 20% of hip fracture patients require long-term nursing home care • Only 40% fully regain their pre-fracture level of independence • Majority of vertebral fractures are initially clinically silent – Often associated with symptoms of pain, disability, deformity and mortality. – Postural changes associated with kyphosis may limit activity, result in restrictive lung disease and lumbar fractures may alter abdominal anatomy, leading to constipation, abdominal pain, distention, reduced appetite and premature satiety Osteoporosis Pathophysiology Osteoporosis Pathophysiology • Bones are not static! They are dynamic – always remodeling – Bone remodeling by osteoblasts and osteoclasts • (Blasts build; Clasts chew) • Bone loss occurs when bone removal > bone growth – Menopause • Remodeling accelerates, enhancing the effect of bone loss – Advancing age – Sex steroid deficiency – Glucocorticoid use • Effect: – disordered skeletal architecture – increased fracture risk Osteoporosis Risk of Fracture Osteoporosis Risk of Fracture Skeletal Fragility 2014 Clinician’s guide to prevention and treatment of osteoporosis; National Osteoporosis Foundation. 2014 Issue, Version 1; Release Date: April 1, 2014 http://nof.org/files/nof/public/content/file/2791/upload/919.pdf Skeletal Fragility (for all) (steroid use + immobility + dz effects) Skeletal Fragility (via changes in bone metabolism and/or falls risk) (↓Ca2+) (↓Ca2+) Osteoporosis Risk of Fracture Osteoporosis Risk of Fracture 2014 Clinician’s guide to prevention and treatment of osteoporosis; National Osteoporosis Foundation. 2014 Issue, Version 1; Release Date: April 1, 2014 http://nof.org/files/nof/public/content/file/2791/upload/919.pdf Falls Risk Osteoporosis Evaluation / Detection • Who should I assess for osteoporosis and fracture risk? • Patients > 50y.o. – Assess risk factors for osteoporosis and fracture to identify those at high risk. » (see previous slides on skeletal fragility and falls risk) • Patients > 50y.o. + Hx of fragility fracture should be assessed [grade A]. Osteoporosis Evaluation / Detection – Assessment: • Detailed history • Focused physical exam 1. Measure height annually, and assess for the presence of vertebral fractures [grade A]. • If > 2 cm height loss – get imaging 2. Assess history of falls in the past year. If there has been such a fall, a multifactorial risk assessment should be conducted, including the ability to get out of a chair without using arms [grade A]. BMD measurement William D. Leslie, MD MSc FRCPC, Umanitoba. Module 5 - Speaking of Bones Osteoporosis For Health Professionals: Fracture Risk Assessment . http://www.osteoporosis.ca/wp-content/uploads/Module-5-Fracture-Risk-Assessment-ppt.pdf 10 Year Fracture Risk The T-score for the femoral neck is derived from the National Health and Nutrition Education Survey III (NHANES III) reference database for white women. CAROC scoring tool: http://www.osteoporosis.ca/multimedia/pdf/CAROC.pdf CAROC Risk Score CAROC: 10 Year Fracture Risk Canadian Association of Radiologists & Osteoporosis Canada • CAROC risk score increased by one category if: • (i.e. Low to Moderate or Moderate to High) 1. Fragility fracture after age 40 2. Recent prolonged systemic glucocorticoid use • For eg. – – 60y.o. woman; femoral neck T-score = -2.8 Hx of fragility # CAROC scoring tool: http://www.osteoporosis.ca/multimedia/pdf/CAROC.pdf FRAX http://www.shef.ac.uk/FRAX/ FRAX http://www.shef.ac.uk/FRAX/ 2010 Guidelines HOW DO I ASSESS 10-YEAR FRACTURE RISK? • 1. Absolute fracture risk based on age, BMD, prior fragility fractures and glucocorticoid use [Grade A]. • 2. Calculate risk using the 2010 CAROC tool and/or Canadian FRAX tool, because they have been validated in the Canadian population [Grade A]. – 3. For purposes of reporting BMD, the 2010 CAROC tool is the preferred national risk assessment system [Grade D]. – 4. Only the T-score for the femoral neck (derived from the reference range for white women of the NHANES III) should be used to calculate risk of future osteoporotic fractures under either system [Grade D]. – 5. Individuals with a T-score for the lumbar spine or total hip ≤ –2.5 should be considered to have at least moderate risk [Grade D]. • 6. Multiple fractures confer greater risk than a single fracture. In addition, prior fractures of the hip and vertebra carry greater risk than fractures at other sites [Grade B]. Osteoporosis Therapeutic Options • A) Exercise and Falls Prevention – 1. Resistance training and/or weight bearing aerobic exercises [grade B]. – 2. Core stability exercises to compensate for weakness or postural abnormalities for patients with vertebral fractures [grade B]. – 3. Balancing exercises (eg. tai chi), or gait training if at risk of falls [grade A]. – 4. Consider hip protectors in long-term care facilities at high risk for fracture [grade B]. Osteoporosis Therapeutic Options • B) Calcium and Vitamin D – Vit D3 (cholecalciferol): 1000-2000 iu daily • Enhances calcium absorption • Very safe in higher doses – Can administer all once weekly if desired – Elemental Calcium – 1200mg daily by diet first and supplements if needed • Any calcium salt will do • Doses > 1500mg/day may increase risk of CV disease, CVA, kidney stones • See: Calculate-My-Calcium online calculator • http://www.osteoporosis.ca/osteoporosis-and-you/nutrition/calculate-my-calcium/ Osteoporosis Therapeutic Options • C) Pharmacological Therapy – Low risk (Major fracture CAROC or FRAX score = 0-10%) • No drug treatment – Moderate risk (10-20%) • Consider treatment – discuss with patient – High risk (>20%) – High risk: FRAX hip fracture score >3% – High risk: > 50y.o. + Hx of hip or spine fragility fracture – High risk: > 50y.o. + Hx of multiple fractures • Treat Pharmacological Therapy 1st Line Therapy w/ Evidence for Fracture Prevention in Postmenopausal Women How to Choose? William D. Leslie, MD MSc FRCPC, Umanitoba. Module 5 - Speaking of Bones Osteoporosis For Health Professionals: Fracture Risk Assessment . http://www.osteoporosis.ca/wp-content/uploads/Module-5-Fracture-Risk-Assessment-ppt.pdf Pharmacological Therapy 1st Line Therapy w/ Evidence for Fracture Prevention in Postmenopausal Women How to Choose? William D. Leslie, MD MSc FRCPC, Umanitoba. Module 5 - Speaking of Bones Osteoporosis For Health Professionals: Fracture Risk Assessment . http://www.osteoporosis.ca/wp-content/uploads/Module-5-Fracture-Risk-Assessment-ppt.pdf Rational Prescribing Prioritize: 1. Type of harm 2. Quantity of harm 3. Quality of evidence 4. Time to harm Prioritize: 1. Type of benefit 2. Quantity of benefit 3. Quality of evidence 4. Time to benefit 1. Efficacy 2. Toxicity 3. & 4. Cost & Convenience 1st Line Therapy w/ Evidence for Fracture Prevention in Postmenopausal Women How to Choose? William D. Leslie, MD MSc FRCPC, Umanitoba. Module 5 - Speaking of Bones Osteoporosis For Health Professionals: Fracture Risk Assessment . http://www.osteoporosis.ca/wp-content/uploads/Module-5-Fracture-Risk-Assessment-ppt.pdf Agent Alendronate (Fosamax®) (Fosavance®) Toxicity Cost / Convenience Esophagitis Adynamic bone disease Osteonecrosis of the jaw Hypocalcemia 10mg po daily or 70mg po weekly 70mg+(2800iu or 5600iu Vit D) po weekly ODB covered Fasting, ++ H2O admin; upright t1/2 ~ > 10 years! ~ same 5mg po QD / 35mg po qWk / 150mg po qMo [Fasting, ++ H2O admin; upright] 35mg DR formulation – w/ food $$ ODB covered; t1/2 ~ 3 weeks Risedronate (Actonel®) (Actonel DR®) Zoledronate (Aclasta®) Denosumab (Prolia®) ~ same (newer, less known) (minus esophagitis) (plus ?AFib) infusion reactions, myalgias Unknown - too new ?malignancy, ?infection ?CV or ?ocular effects Derm events ONJ Hypocalcemia 5mg IV once yearly ODB covered $$ 60mg sc q6months ODB covered with LU code 428 or 429 $$$ Duration of Therapy • Usually sequential, not combination – Very rarely combo therapy for short term if very high risk – Benefits disappear rapidly after discontinuation – Benefits beyond 5 years not well described – Rare safety concerns more common after 5 years • Little guidance on when to stop or restart – Reassess after 5 – 7 years and ?D/C – Alendronate – t ½ 10 years: 1 - 2 yr off then R/A – Risedronate – t ½ 3 weeks: 6 – 12 mo off then R/A – Denosumab – t ½ 4 weeks: 6 – 12 mo off then R/A Unknowns in the Literature • • • • When to D/C When to restart Ideal duration of therapy Long-term safety data of newer agents • Clinical judgment required Cases • http://www.osteoporosis.ca/wpcontent/uploads/Module-5-Fracture-RiskAssessment-ppt.pdf • Slide #40 onwards Questions?