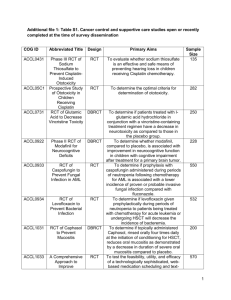
1045-1215 - cancer
advertisement
SUMMER COURSE: INTRODUCTION TO EPIDEMIOLOGY The Primary Study Designs AUGUST 25, 1045-1215 Dr. N. Birkett, School of Epidemiology, Public Health and Preventive Medicine, University of Ottawa Session Overview • Classification of epidemiological study designs • Hierarchy of evidence • Brief overview of key designs • Ecological study • Case-control • Cohort • Randomized controlled trial Scenario (1) A surgeon mentions over coffee that she has been treating a lot of cases of adenocarcinoma of the esophagus in the past few years. This is quite a change from when she was a resident where nearly all cases of esophageal cancer were of the squamous cell type. She also notes that she hardly ever sees a woman with esophageal cancer; the typical patient is an overweight man with a history of heavy smoking. Scenario (2) This gets you interested. A number of questions enter your mind: • Has there really been a shift in pattern? • What are the characteristics of the people getting adenocarcinoma of the esophagus? • Do people who smoke more actually have a higher risk? Does smoking cause adenocarcinoma of the esophagus? • What happens to people with this cancer? • How well does surgery do in treating people? Does it affect survival, quality of life or nothing? Types (1) Can group the previous scenarios into 3 broad groups: 1&2 Descriptive observational Analytic hypothesis generating hypothesis testing 3&4 5 Analytic hypothesis testing experimental observational Types (2) Descriptive • • • Attempt to describe a situation. There is no a-priori hypothesis or theory being tested. Rather, we just want to learn about how the condition is distributed. Tends to use very simple statistics. Analytic • • Usually more focused on pre-specified theories or hypotheses Uses more complex statistics (e.g. logistic regression) Types (3) Hypothesis generating • Early stage study designed to generate hypotheses or ideas to be tested in more focused studies. • Very unusual to have NO prior hypothesis or theory. • • Some people argue science is never done in isolation from prior biases/hypotheses. Most studies will generate hypotheses even if not the main purpose Hypothesis testing • A main purpose of the study is to test a specific theory or hypothesis. • Uses more complex designs and statistics • Karl Popper and falsification. Types (4) Observational • Studies people ‘as they lie’. Decision about whether to be exposed is made by subjects • Most common epidemiological study type. • Most potential for bias and error. Experimental • Exposure is determined by the investigator. • Most well known type is a Randomized Controlled Trial (RCT). BUT, this is not the only type. • Unethical in many situations (e.g. does smoking cause esophageal cancer?) • Often viewed as the ‘gold standard’ of study designs Scenario (3) Back to our research questions. Has there really been a shift in pattern? • Obtain data from Canadian Cancer Registry from 1980 to 2000. Compute incidence and look for trends. • • Depends on the availability of cancer morphology information in registry Look at US SEER data set • Chart review of tertiary care hospitals Scenario (4) What are the characteristics of people getting adenocarcinoma of the esophagus(ACE)? • Chart review of tertiary care hospitals • Review Canadian Cancer Registry records for geographic distribution, etc. • Depends on the availability of information • Look at US SEER data set • Recruit group of ACE patients and ask a range of questions about their past • • Lack of comparison group Collect data for various countries and see if those with high ACE rates have higher rates of something else. Scenario (5) Do people who smoke more actually have a higher risk? Does smoking cause ACE? • Collect a group of smokers and a group of non-smokers. Follow them to see if smokers get more ACE. • • Need large group and long follow-up Collect a group of people with ACE and a group without ACE and see if the former has more smokers in it. Scenario (6) What happens to people with this cancer? • Identify a group of people with ACE. Follow them up every two months to find out what has happened to them • • • • • Death Treatment Quality of life Progression; biomarkers Some design questions: • • Do you need to follow any people without ACE? When in the course of the disease should you recruit subjects? Scenario (7) How well does surgery do in treating people? • Identify a group of people with ACE, some of whom have had surgery and some who haven’t. Follow them up every two months to find out what has happened to them and compare the groups • Identify patients with new ACE. Flip a coin to determine if each patient will get surgery or not. Non-surgery patients would get standard care. Follow-up them up as in above study. Hierarchy of Evidence (1) • Studies can be roughly ranked on the strength of evidence the provide. • Only an approximate guide: a very bad RCT can provide less evidence than a really good case series. Warning! ANY attempt to classify studies is doomed to failure. • Some studies just don’t ‘fit’ • Some studies have multiple objectives and/or designs. Types of Epidemiological Studies Case Study Case Series Ecological (correlational) Weaker Stronger Laboratory and anecdotal clinical evidence suggest that some common non-antineoplastic drugs may affect the course of cancer. The authors present two cases that appear to be consistent with such a possibility: that of a 63-year-old woman in whom a high-grade angiosarcoma of the forehead improved after discontinuation of lithium therapy and then progressed rapidly when treatment with carbamezepine was started and that of a 74-year-old woman with metastatic adenocarcinoma of the colon which regressed when self-treatment with a nonprescription decongestant preparation containing antihistamine was discontinued. The authors suggest ...... that consideration be given to discontinuing all nonessential medications for patients with cancer. RR(1μg/m3) =1.08 RR(10 μg/m3) =2.31 Types of Epidemiological Studies Case Study Case Series Ecological (correlational) Cross-Sectional Case-Control Cohort (Historical) Cohort (Prospective) Weaker Stronger Hierarchy of Evidence (2) Cross-sectional study. • Measures subjects at one point in time. Like a political poll. • Tells you the number (or proportion) of people who have a condition at a point in time (prevalence). • Useful for estimating Burden of Illness • Can look at associations of risk factors with illness but a weak design to look at causation or etiology. • An association might be due to prolonging life, not causing the disease. Hierarchy of Evidence (3) Cross-sectional study. • Consider type 1 diabetes mellitus. • Around 1910, it was a fatal disease (< 1 year survival). You wouldn’t find many cases in a cross-sectional study. • After insulin developed, people now live 20+ years • Cross-sectional study would show that: • • • • Most people with type 1 diabetes were using insulin. Very few people without type 1 diabetes used insulin. Seems to imply insulin use causes diabetes. But, we know that is nonsense. • Incidence-prevalence bias (Neyman bias). Hierarchy of Evidence (4) Case-control study. • Select a group of people with the disease or outcome of interest (cases) • Select a group of people without the disease or outcome of interest (controls or referent group) • Ask each group about history of previous exposure. • Compare occurrence of exposure in the cases and controls. Case-Control Study (1) Disease Exposure YES NO YES a b a+b NO c d c+d a+c b+d N Hierarchy of Evidence (5) Cohort study. • Select a group of people with the exposure of interest • Select a group of people without the exposure of interest • OR simply select a group of people with a range of exposure experiences • Follow all subjects up to determine if they develop new cases of the outcome. • Compare the incidence of the outcome in each group. Cohort Study (1) Disease Exposure YES NO YES a b a+b NO c d c+d a+c b+d N Types of Epidemiological Studies Case Study Case Series Ecological (correlational) Cross-Sectional Case-Control Cohort (Historical) Cohort (Prospective) Non-randomized Clinical Trial Randomized Clinical Trial (RCT) Weaker Stronger Hierarchy of Evidence (5) • Randomized Controlled Trial. • Key feature: decision about which subjects are ‘exposed’ is made by the investigator. • Other than that, an RCT is just a cohort study. • Methodological standards are more rigorous since you have more control over the study and the participants. • Non-RCT’s • Can be very powerful in some settings • Latin squares; BIBD’s Other study names • Other study names & types exist • Quasi-experimental studies • Solomon four group design • Community evaluations • Qualitative Studies RCT design (1) • A randomized controlled trial (RCT) is main method to evaluate new treatments. • Seen by many as ‘gold standard’ design. • Essentially, RCT is a cohort study in which the investigator decides which subjects are in which groups. • Main benefits arise because you can control more features • Who gets which treatment • Balance out ‘other’ treatments/exposures • But, problems can arise if not designed well. RCT Population R Control Group Treated Group RCT design (2) • Document everything in writing. • Maintain audit trail • Register the trial • Clear eligibility criteria • Method of doing allocation • Blinding • Avoid contamination • Avoid co-interventions • Poor compliance/adherence RCT design (3) Clear eligibility criteria • Who enters study? • Clinical criteria • Don’t just say: • Patient must have had a heart attack • Personal features • How is eligibility determined? • Timing • Who does it • What if lab tests can’t be back in time? RCT design (4) Method of doing allocation • Seems simple but can be subverted • Envelopes – pre-opening; transparent • Deliberate fraud • Stratification • Obtain information on risk factors for outcome (e.g. age, cancer stage, sex) • Allocate subject to ensure balance in treatment groups • Availability of stratification factors can be problematic. • Central vs. local methods • 24 hour service, especially with multi-site studies RCT design (5) Blinding • A key feature • Means that someone involved with the study is unaware which treatment has been assigned to the subject. • Requires use of placebos • Hard to produce, especially for non-drug treatments. • Intended to reduce the risk of conscious or unconscious bias • Goniometer example. RCT design (6) Blinding (cont.) • Who should be blinded? • The Patient • Avoid placebo effect • Treatment health care team • People doing evaluation of the outcome • Trial over-sight committee • The analysis team (statistician) • Often impossible to blind some people • How to blind a surgeon about which operation to do? • Essential to blind people doing subjective assessments. RCT design (11) We could go on for hours! RCT’s seem simple but are very complex to design well. Come back and do our graduate courses on the design of intervention studies and RCT’s. Summary • Epidemiological studies have different purposes depending on the ‘stage’ of understanding • Key designs are • Ecological • Cross-sectional • Case-control • Cohort • RCT • Some designs are ‘better’ than others