February 12 & 19
advertisement

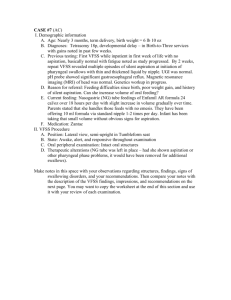
SPHSC 543 FEBRUARY 12-19, 2010 Questions? TRANSITIONAL FEEDING Begins at 4-6 months in normal infants … Primarily related to CNS and anatomic changes … Allows new patterns of food manipulation Eruption of teeth is the most notable change … Mandibular before maxillary … Girls before boys 20 teeth by second year, 32 by adult TRANSITIONAL Teeth as sensory receptors versus motor purposes Molars important for crushing and grinding food Tongue movements are basic to food manipulation … Anterior-posterior (AP) movement … Lateral movement TRANSITION FROM LIQUIDS Smooth solids – homogeneous or with fine granular bits … Mashed by tongue gestures at midline Semifirm solids – soft but holds together … Tongue moves laterally and tongue/jaw make vertical motions … A prelude to molar chewing Solids – require more mature mastication … Vertical movements become associated with alternating lateral motions … Fully matures between 3-6 years TRANSITIONS Solid foods characterized by: … Handles lumps and textures with ground or mashed foods … Coarsely chopped foods cooked ground meats, lunch meats, soft cooked chicken/fish … Coarsely chopped table foods, most meats, many raw vegetables/fruits. Brain development from sensory input related to feeding extending to midbrain, cerebellum, thalamus and cerebral cortex With maturity, children begin to evaluate their food and you start to see food preferences. TASTE AND SMELL Important roles in feeding Experience Preference “Supertasters” CESSATION OF NIPPLE-FEEDING Multi-factorial … Age, culture, maternal desire, lifestyle Need appropriate CNS development and coordination to manage cup drinking … Open cup … Sippy cup Prolonged nipple-feeding and dental caries OVERALL DEVELOPMENT Take away information: Changing feeding experiences are just a portion of a more general evolution of the developing child Sensory and motor skills improve and the child acquires food preferences. METHODS OF FEEDING DELIVERY Oral includes bottle, breast, cup, straw, fingers, utensil Orogastric Nasogastric … Short term usage Gastrostomy … Longer term Continuous or bolus But wait….new information is afoot. Duodenum or jejunum FEEDING DELIVERY METHODS Parenteral … For severe GI disorders that prevent use of the GI tract … Peripheral vein access … Central venous catheter CLINICAL FEEDING EVALUATION Observation is the key component of the clinical feeding evaluation … Eyes … Ears … Hands Need to understand the normal functions and how they interact … Interaction of reflexes … Developmental changes … Respiration … Gastrointestinal … Etc. CLINICAL FEEDING EVALUATION Consider the ‘whole’ infant Gather information from all sources Plan the feeding observation … Equipment … Food textures … Physiologic monitors … Naturalistic and/or elicited CLINICAL FEEDING EVALUATION Structured feeding history … Parent description of the problem – allows them to be in control for the first part of the interview … State/behavior – of infant … Schedule – basic nutritional intake and amount of time spent feeding each day … Method of feeding – helps determine a ‘typical’ feeding … Feeding problems observed by parent – alerts the clinician for what to look for TREATMENT EXPLORATION – HINT FOR FINAL EXAM Develop hypotheses Synthesize information … What is the child’s level of function? … What factors interfere with feeding function? … How well does the child’s feeding performance “match” the caregiver concerns or expectations? … Is additional information necessary? … Are there treatment techniques available that appear to improve oral feeding function? KEY AREAS Physiologic control Motoric control Behavior and state Response to tactile input Oral-motor control Sucking, swallowing and breathing General observations CLINICAL FEEDING EVALUATION From Wolf & Glass, 1992 From Wolf & Glass, 1992 CLINICAL FEEDING EVALUATION An infant’s responses to the environment can indicate how stressful the baby finds the environment and how well she is able to adapt Response to the environment is manifested through behaviors in any of the following systems: … Autonomic or physiologic … Motoric … State … Attention What is happening during the feeding at the time of the stress cue? AUTONOMIC/PHYSIOLOGIC Heart rate … Initial and post-feeding … Highest/lowest values … Abrupt changes Respiratory rate … Pre/post-feeding … Highest, lowest, trends … Returns to baseline BREATHING Quality of respiration Parameters: respiratory effort, changes in respiratory pattern, sound of respirations. Work of breathing Endurance AUTONOMIC/PHYSIOLOGIC Oxygen saturations … Amount of o2 in blood and avail for exchange at tissue level … Generally expressed as a percentage of 100 Color … Face, neck, mouth (circumoral) … Eyes (circumorbital). … Pale … Blue/purple … Red or ruddy AUTONOMIC STRESS CUES From Wolf & Glass, 1992 MOTORIC Overall neuromotor control … Disorganized … Tone Muscle tone … At rest … Change with activity … Quality of movement … Tonal variations versus movement disorder MOTORIC Reflexes … Primitive … Integration … extinguish Posture … Development of antigravity postural control … Feeding position Motor Response to environment Knowledge of feeder MOTORIC STRESS CUES From Wolf & Glass, 1992 FEEDING POSITION Normally feeding babies – adaptable Even slight feeding problems might need help for optimal feeding. Overall body posture reflects slight flexion Trunk is neutrally aligned and well supported in a semi-reclined position, with orientation of the head and extremities about the midline. Using proper positioning during feeding not only affects respiratory mechanism, oral-motor control and swallowing control, but it may also assist in the development of early head/neck postural responses. STATE States of alertness … State 1 – deep sleep … State 2 – light sleep … State 3 – drowsy or semi-dozing … State 4 – quiet alert … State 5 – active alert … State 6 – crying STATE Not one optimal state for every baby FT (full term) – should have clear differentiation between states Preemies – may seem more disorganized and lack clarity of state Older babies – spend more time awake/alert and have clearer/more predictable state changes STATE-RELATED STRESS CUES From Wolf & Glass, 1991 STATE Is state or state control interfering with feeding? How does parent respond or support baby? What is the baby’s state throughout the feeding? Factors interfering with state control (immaturity or neurological impairment) may require prolonged need for state-related intervention. TACTILE INPUT Tactually elicited reflexes present at birth allow the infant to seek out and obtain nutrition safely. Ability to accept touch to the cheeks, lips, gums and tongue is a prerequisite for feedings and the infant’s survival. Expression of oral reflexes varied depending on a number of factors. Must adapt to the tactile components of the tools used in feeding TACTILE INPUT Face … Cheeks to lips to gums to tongue … Head, trunk, extremities Input –graded … firm and smooth (pressure from fingers or toy) to … soft and smooth (stuffed animal or soft finger touch) to … prickly or unusual (rubber hedgehog toy). … Same with sold foods … move from smooth/pureed to chunky (baby food/cottage cheese) to crunchy (crackers) DEGREE/PERSISTENCE OF RESPONSE Absent responses Hyposensitive Hypersensitive and Aversive … Immaturity … Chronic illness … Experience … Neurologic impairment ORAL MOTOR – TONGUE Resting position … Soft, thin, flat, moderately rounded tip Size … Relative to oral cavity Deviations … Tongue-tip elevation … Humped/bunched/retracted Tone … Clonus … Fasiculations … Asymmetric JAW Resting position … Stable platform for tongue, lips, cheeks Size … Micrognathic … Retrognathic Deviations … Asymmetrical or lateral Range of motion … Poorly graded … Clenching, biting LIPS/CHEEKS Resting position … Soft, symmetrical … Well-defined Fat or sucking pads … Positional stability Deviations … Tight, pulled back … Pursed or floppy Tone … Hypotonia PALATE Shape … Intact … Smooth contour … Roughly approximates shape of tongue … Narrow, grooved, arched or flat Clefting … Interferes with ability to achieve negative intraoral pressure for suction Asymmetry SUCKING-SWALLOWINGBREATHING Evaluate the integrity of each as well as their coordination/organization Rhythmicity – hallmark of normal sucking Suction Nutritive VS Non-nutritive Coughing/choking Oral secretions Noisy breathing Nasal regurgitation Frequency of respiratory infections GENERAL OBSERVATIONS Method of feeding Bottle/nipple used Length of feeding, amount taken Reason for ending the feeding Spitting/emesis Parent-child interaction RED FLAGS Prolonged feeding time Limited volume Uncoordinated SSB Coughing, choking, sputtering with feeds Recurrent respiratory problems Persistent drooling Slow weight gain/FTT Food aversion/sensitivity Problems transitioning to next diet level Poor oral motor skills DIAGNOSTIC TESTS/PROCEDURES Basic understanding of common tests regardless of professional practice setting. Strengths/limitations Implications of results Integrate data into clinical feeding observation Is additional information needed? Most developed for adults; lack of normative data with children (manometry, FEES, scintigraphy) PHYSIOLOGICAL MONITORING Heart rate, respiratory rate, oxygen saturation Cardiorespiratory monitor … Numerical and visual display of heartbeat and respiration … Averaged over a given period of time (e.g., 10 secs … Strengths – quick approximation of infant’s status. … Movement artifact /not always accurate PHYSIOLOGICAL MONITORING Oximetry – … Oxygen saturation of capillary blood flow through an external sensor. … Expressed as a percentage of 100. … Normal infant -- sats above 95% Below 90% generally indicate some degree of hypoxia. Baseline, changes in response to work/handling, effectiveness of O2 treatment PHYSIOLOGICAL MONITORING Strengths – … Easy to transport, non-invasive … Ongoing, instantaneous info … More reliable index than observation Limitations – … Very sensitive to movement … Natural pigment of baby … Ambient light/infrared heating sources PHYSIOLOGICAL MONITORING Pneumogram – … Two-channel study based on chest wall excursion and heart rate … Computerized –multichannel recording of parameters such as heart rate, RR, O2 sats, nasal airflow, esophageal pressures … Gives exact values rather than averaged values so subtle changes in parameters are identified. PHYSIOLOGICAL MONITORS Polysomnogram – “Sleep study” … Multichannel recording of respiration, airflow, chest and diaphragm movement, oxygen and carbon dioxide levels, heart rate and esophageal pressures … EEG recordings for length of two complete sleep cycles … Measures the greatest number of variables … Differentiates between central and obstructive apnea, apnea secondary to seizures, obstructive apnea due to GER or airway collapse … Limitations – specialized sleep lab, expertise GASTROINTESTINAL Technetium scan (AKA GE scintigraphy or a milk scan) … Small amount of radionuclide isotope is added to the feeding … Images are made every 30 seconds over a one hour period after the feeding looking for material in the esophagus. … Number/height of reflux episodes calculated and compared with standards … Gastric emptying computed by measuring the percentage of food remaining within the stomach after on hour. GASTROINTESTINAL Strength … Info on several important parameters of GER: Acidity/alkaline reflux … Unlikely to miss reflux events … Height of reflux in esophagus … Contribution of delayed gastric emptying … Radioactive tracer not absorbed and total radiation exposure is low Criticized … Overly sensitive to reflux … High false positive rate GASTROESOPHAGEAL Barium swallow (AKA esophogram or upper GI) … Evaluates structure and function of esophagus and stomach … Ba delivered either orally or NG tube … Fluoroscopy – real-time events observed … Still photos taken for later review … Esophageal motility can be evaluated … Presence of spontaneous reflux or attempt to elicit by giving pressure to abdomen … Rad exposure is proportional to time of exposure, but generally brief … Not sensitive enough to GER, may detect aspiration UGI From Wolf & Glass, 1992 GASTROINTESTINAL pH probe –GER … Sensor inserted through nose to an area just above LES to continuously measure acidity of esophagus … At least a 24 hour hospital stay … Record kept at beside of baby’s activities for later correlation with changes in pH. Data is recorded on the total number of episodes of pH <4.0, total time with pH<4.0, number of episodes greater than 5 mins, and longest episode of pH<4.0. Typically, episodes of pH<4.0 must last longer than 10 secs to be recorded. GASTROINTESTINAL pH probe –GER … Sensor inserted through nose to an area just above LES to continuously measure acidity of esophagus … At least a 24 hour hospital stay … Record kept at beside of baby’s activities for later correlation with changes in pH. Data is recorded on the total number of episodes of pH <4.0, total time with pH<4.0, number of episodes greater than 5 mins, and longest episode of pH<4.0. Typically, episodes of pH<4.0 must last longer than 10 secs to be recorded GASTROESOPHAGEAL Data generates a reflux score ‘Gold standard’ for evaluation of GER AIRWAY/GASTROINTESTINAL Pediatric Endoscopy … Esophagoscopy/esophageal manometry, laryngoscopy, bronchoscopy Rigid or flexible tube Directly observes structures within the body Obtain tissue via biosy or aspiration Treatment Advances in fiberoptics permitted flexible endoscopes that can be used with even extremely small infants VIDEOFLUOROSCOPIC SWALLOWING STUDY (VFSS) VFSS aka MBS … Specifically designed to assess the pharyngeal swallow … Normal feeding situation is simulated but may need to use ‘tricks’ … Purpose –document aspiration, reason for aspiration and the point at which it occurs … Assess possible therapeutic interventions … Positioning can be customized VFSS From Wolf & Glass, 1992 CFE LIMITATIONS Info not readily obtained at bedside: … VP function … Laryngeal elevation and closure … Pharyngeal motility, transit time … Pooling of secretions and contrast in valleculae and pyriform … Number of swallows to clear material … Presence and timing of aspiration in relation to the swallow. … Bolus movement through UES and esophagus VFSS SLP/MD … Observations relating to timing of swallow … Coordination in oral/pharyngeal phase … Phary peristalsis … Pooled material prior to swallow or residue after … Esophageal transit time … Aspiration before, during, after swallow VFSS Seating/postioning – … Support of trunk, neck and head … Semireclining angle of approx 45 degrees. … Tumbleform chair … Child’s own seating system … Most wheelchairs don’t fit; some have removable parts … Height of seat in relation to floor VFSS Need careful guidelines for appropriate … Radiologic risks to infant versus the yield of info from the test … How will information be used? Personnel involved varies – … OT, SLP, MD, tech … Regardless, should have expertise in infant and skill in interpreting images Parent participation VFSS Emergency back up equip and personnel as needed Flexible enough protocol to address each baby’s needs Endurance VFSS -- FEEDING TECHNIQUE Multiple variables … Nipple, syringe, nipple alternating with pacifier to look at NNS and NS, spoon, cup, straw, liquid thickness, solids Bolus type, amount, texture, temperature, timing can be varied Risk of aspiration kept at minimum Caregivers provide samples of food … Regularly given … Causing trouble … Introduction Lateral view -- most important and most information VFSS AP view— … Documenting asymmetry/pooling … Head positions Therapeutic changes Flexed, extended, turned, etc. Neurologically impaired … Better at handling homogeneous consistency VFSS Alternate feeding methods with plans for oral-motor stimulation Repeat studies: … Significant change in medical or neurological status … Recurrence of previous symptoms … Previous documentation of silent aspiration … Tx program changes are indicated for diet textures or compensation techniques Improved oral-motor function in profoundly neurologically impaired children have not shown to be directly correlated with improved pharyngeal transit time. VFSS -- LIMITATIONS Lack of standardization – … Positioning … Amount and order of presentation … Therapeutic modifications … Overly sensitive VFSS VS CLINICAL FEEDING EVALUATION (CFE) Benefits of CFE first – … Establish baseline behaviors to compare with feeding during VFSS. … Feeding during VFSS is often not representative Paradoxical performance Has significant feeding d/o but swallows Ba without difficulty Pre-determine types/textures of foods, order of presentation, optimal positioning, equipment needed Able to formulate and test treatment strategies VFSS Confirms need for VFSS … Radiation exposure Signs during CFE … Coughing/choking … Noisy, wet respirations … Subtle signs –unexplained respiratory infection or illness, difficulty managing oral secretions. Aspiration can be silent … Logemann reports 40% of adult patients who asp during VFSS not identified during bedside VFSS Pay particular attention to medical history, parent descript of feeding, subtle indicators of potential swallow dysfunction Generalizability of feeding sample has been questioned … Relatively brief sampling … Ba may alter baby’s swallowing response Not intended to identify GER as objective, but can be seen