Psychological Aspects of Weapon Safety
advertisement

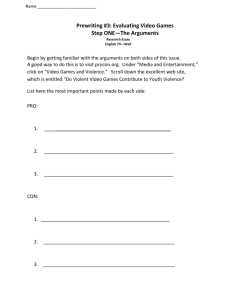
PROTECTING THE RIGHTS OF THERAPISTS WITH DIFFICULT AND THREATENING CLIENTS: ETHICAL AND LEGAL CONSIDERATIONS Florida Psychological Association (3 HOURS) Abridged Powerpoint from seminar originally presented by: Presented by Ernest J. Bordini, Ph.D. & Robert Henley Woody, Ph. D., Sc. D., J. D., ABPP July 14, 2006 -- Sarasota, Florida PROTECTING THE RIGHTS OF THERAPISTS WITH DIFFICULT AND THREATENING CLIENTS: ETHICAL AND LEGAL CONSIDERATIONS (3 HOURS) Presented by July 14, 2006 -- Sarasota, Florida Presenters: Robert Henley Woody, Ph. D., Sc. D., J. D., ABPP Ernest J. Bordini, Ph. D. (Clinical Psychology Associates of North Central Florida, P.A., Gainesville, FL) Tony Galietti WORKPLACE VIOLENCE Workplace Homicide Trends • Workplace homicides 1993 through 2002 declined from 1,074 workplace homicides in 1993 to 609 in 2002 - a 43% decline. • This decline did not, however, occur uniformly across all demographic and occupational categories. • Within that time period, health service industry homicides did not decline 14 in 1993 vs. 13 in 2002. • Source: Census of Fatal Occupational Injuries (CFOI) • The Bureau of Labor Statistics’ Census of Fatal Occupational Injuries (CFOI) reported an average of just under 800 homicides per year between 1992 and 2006. The largest number of homicides in one year (n=1080) occurred in 1994, while the lowest number (n=540) occurred in 2006. Workplace Homicide Trends • Victimization rate for mental health professionals and custodial workers was 6.82 per 100 workers compared to a rate of 1.26 per 100 workers across all occupations combined (Durhart 2001). • Non-fatal assaults on health care workers includes assaults bruises, lacerations, broken bones and concussions but those reported to the Bureau of Labor Statistics (BLS) only include injuries severe enough to result in lost time from work. • References: Duhart, D.T. (2001). Violence in the workplace, 199399 (No. December 2001, NCJ 190076). Washington, DC: U.S. Department of Justice, Office of Justice Programs. ABC7 Newsline: Psychologist Gunned Down In Vallejo Office • Nov. 2, 2005 Was it a patient who murdered an East Bay psychologist? Vallejo police are planning to look through his patient files after the doctor was gunned down after a long day of counseling. It's a theory Vallejo police confirm they're pursuing, after the 64-year-old Polonsky was gunned down in his office Tuesday night. • A lone gunman walked up to Polonsky's second floor office past a waiting patient and shot the doctor in the chest in the hallway. • Dr. Polonsky provided family, couples and individual therapy in Vallejo for 25 years. •ABC7 Talks To Victim's Sons • Reform school teens charged in counselor's death • • Tuesday, November 11, 2003 - By Barbara White Stack and Patrick Hernan, Pittsburgh Post-Gazette • Two teenagers at a Mercer County reform school yesterday were accused of strangling a school counselor, whose legs and hands had been tied and a sheet fastened around his neck and head, and taking his truck to Pittsburgh. Assaults in the Health Care Sector • Average of 1.7 million episodes/yr. of victimization at work per year 1993-1999 (Department of Justice National Crime Victimization Survey (NCVS), Durhart, 2001). • The health care sector continues to lead all other industry sectors in incidence of nonfatal workplace assaults. In 2000, 48% of all nonfatal injuries from violent acts against workers occurred in the health care sector (Bureau of Labor Statistics BLS, 2001). • Nurses, nurse's aides and orderlies suffer the highest proportion of these injuries. Non-Fatal Victimizations I ncidence rates for nonfatal assaults and violent acts by industry, 2000 Incidence rate per 10,000 full-time workers Source: U.S. Department of Labor, Bureau of Labor Statistics. (2001). Survey of Occupational Injuries and Illnesses, 2000. Violent Crime against Mental Health Workers Violent crime for all occupations is 12.6 per 1,000 workers. • The average annual rate for physicians is 16.2; • for nurses,21.9; • for mental health professionals, 68.2; • for mental health custodial workers, 69. Factors Associated with Workplace Violence in Health Care Settings OSHA, 2004 • The prevalence of handguns and other weapons among patients, their families or friends; • The increasing use of hospitals by police and the criminal justice system for criminal holds and the care of acutely disturbed, violent individuals; • The increasing number of acute and chronic mentally ill patients being released from hospitals without follow-up care • The availability of drugs or money at hospitals, clinics and pharmacies, making them likely robbery targets; • Factors such as the unrestricted movement of the public in clinics and hospitals and long waits in emergency or clinic areas that lead to client frustration over an inability to obtain needed services promptly; • The increasing presence of gang members, drug or alcohol abusers, trauma patients or distraught family members; • Low staffing levels during times of increased activity such as mealtimes, visiting times and when staff are transporting patients; • Isolated work with clients during examinations or treatment; • Solo work, often in remote locations with no backup or way to get assistance, such as communication devices or alarm systems (this is particularly true in highcrime settings); • Lack of staff training in recognizing and managing escalating hostile and assaultive behavior; and • Poorly lit parking areas. Workplace Violence in Health Care Settings OSHA, 2004 • Elements of an effective violence prevention program • Management commitment and employee involvement; • Worksite analysis; • Hazard prevention and control; • Safety and health training; and • Recordkeeping and program evaluation. De-institutionalization means higher risk patients are being seen outpatient De-institutionalization means higher risk patients are being seen outpatient “Even patients estimated to be at high risk of violence to others may be discharged in a few weeks, or increasingly, in a few days, assuming that they are ever hospitalized in the first place” Monahan, J., Bonnie, R., Appelbaum, P. S., Hyde, P. S., Steadman, H. J., & Swartz, M. S. (2001). Mandated community treatment: Beyond outpatient commitment. Psychiatric Services, 52, 1198– 1205. What do most therapists consider in assessing violence risk? • • • • history of violence (66%) Medication noncompliance (33%) substance abuse (28%) poor anger control (21%) • Eric B. Elbogen, Matthew T. Huss, Alan J. Tomkins, Mario J. Scalora Clinical Decision Making About Psychopathy and Violence Risk Assessment in Public Sector Mental Health Settings Psychological Services 2005, 2(2) 133–141 Kevin S. Douglas, Jennifer L. Skeem VIOLENCE RISK ASSESSMENT Getting Specific About Being Dynamic Psychology Public Policy, and Law 2005, Vol. 11, No. 3 347–383 A causal dynamic risk factor is a variable that has been shown to: 1. precede and increase the likelihood of violence (i.e., be a risk factor); 2. change spontaneously or through intervention (i.e., be a dynamic factor); 3. predict changes in the likelihood of violence when altered (i.e., be a causal dynamic risk factor). Evolution of Study of Static Factors to Dynamic Risk Factors for Violence Proposed Dynamic Risk Factors • • • • • • • • • • • Impulsiveness Negative affectivity Anger Negative mood Psychosis Antisocial attitudes Substance use and related problems Interpersonal relationships Treatment alliance and adherence Treatment and medication compliance Treatment–provider alliance • Kevin S. Douglas, Jennifer L. Skeem VIOLENCE RISK ASSESSMENT - Getting Specific About Being Dynamic Psychology, Public Policy, and Law 2005, Vol. 11, No. 3, 347–383 Screening for Domestic Violence: Recommendations Based on a Practice Survey Sarah L. Samuelson and Clark D. Campbell Professional Psychology: Research and Practice 2005, Vol. 36, No. 3, 276–282 • Steps That Psychologists Can Take to Assist Victims of Domestic Violence • Decide to implement a screening protocol. • Obtain more training as needed. Previous training may be insufficient • or outdated. • Establish links with community resources prior to screening • implementation. • Obtain information regarding hotline numbers, local shelters, domestic • violence therapy groups, law enforcement, legal aid, advocacy • groups, educational and financial services, and food and housing • assistance. Screening for Domestic Violence: Recommendations Based on a Practice Survey Sarah L. Samuelson and Clark D. Campbell Professional Psychology: Research and Practice 2005, Vol. 36, No. 3, 276–282 • Maintain a supply of domestic violence literature to offer to clients. • Screen all adolescent and adult clients for domestic violence at the time • of intake. • Also include questions regarding personal safety on client completed • intake forms. • Screen in privacy and maintain confidentiality. • Screen couples individually. Emphasize that this is a standard • component of the intake process. • Validate identified victims’ experiences. Screening for Domestic Violence: Recommendations Based on a Practice Survey Sarah L. Samuelson and Clark D. Campbell Professional Psychology: Research and Practice 2005, Vol. 36, No. 3, 276–282 • • • • • • • • • • • • • Acknowledge that many women experience domestic violence, that domestic violence is illegal and inappropriate, that it results in physical and psychological damage, and that a variety of resources are available for victims. Assess identified victims’ level of safety. What threats have been made to the client? How accessible is the client to the abuser at this time? Is the client requesting immediate protection by law enforcement or the safety of a shelter? If the client is not in imminent danger, has she devised a plan to protect herself and any children if the danger escalates? Does the client know how to access community resources if she feels unsafe? How can employees protect themselves? • Nothing can guarantee that an employee will not become a victim of workplace violence. These steps, however, can help reduce the odds: • Learn how to recognize, avoid, or diffuse potentially violent situations by attending personal safety training programs. • Alert supervisors to any concerns about safety or security and report all incidents immediately in writing. • Avoid traveling alone into unfamiliar locations or situations whenever possible. • Carry only minimal money and required identification into community settings. WHAT IS DISRUPTIVE, THREATENING, ASSAULTIVE, OR VIOLENT BEHAVIOR? • Violent behavior includes any physical assault, with or without weapons; behavior that a reasonable person would interpret as being potentially violent such throwing things at someone or in their general direction, pounding on a desk or door in a threatening manner, or threats to inflict physical harm such as direct or implied threats to hit, shoot, stab, or physically harm someone. WHAT IS DISRUPTIVE, THREATENING, ASSAULTIVE, OR VIOLENT BEHAVIOR? • Disruptive behavior disturbs, interferes with or prevents normal work functions or activities. Examples include yelling, using profanity, waving arms or fists, or verbally abusing others. • Threatening behavior includes oral or written threats to people or property, and can include indirect or even vague threats that imply violent action or retaliation. This involves statements that a reasonable person could believe was a threat. • A specific threat to someone’s safety or well-being with the apparent ability to carry it out is legally considered an assault and may be subject to criminal investigation and prosecution. When faced with an escalating individual Avoid yelling, name calling, sarcasm, or other behaviors -These are disrespectful can go a long was in reducing the intensity of a conflict or problem. Being firm is not the same as being loud. Speaking softer and slower is better. Keeping hands relaxed and avoiding threatening stances, gestures or postures. When dealing with an angry individual, don’t crowd, leave space. When faced with an escalating individual (no threat or weapons) Respond quietly and calmly. Try to de-escalate the situation. Do not take the behavior personally. Ask questions, display respectful concern. Indicate you are taking the person seriously. Communicate understanding by calmly and clearly summarizing what the person is telling you. Dealing with escalation or disruption (no weapons, threat, ctd.) • Consider offering an apology, even if you've done nothing wrong. This may calm the person now. Try to establish mutual cooperation in solving the problem. Try to establish some areas of agreement. • If this does not stop the disruption, and in your judgment the person is upset, but not a threat or dangerous, set some boundaries or limits and seek any necessary assistance: • Calmly and firmly set limits by directing the person to lower their voice, or stop engaging in whatever disruptive behavior they may be doing, with the message that this will make it easier for you to try to help them or help to resolve the problem. • If the behavior persists warn the individual that appropriate action may follow, such as calling for some for of assistance from other staff that may be available, superiors, or if necessary law enforcement. Ask them to leave or follow up with getting assistance if they do not. If the person seems Dangerous: • Try to reduce any audience and find a quiet place to talk, but do not leave yourself alone with the individual. • Maintain a safe distance, do not turn your back, and do not place the individual between you and a safe exit. If seated, sit near the door and make sure someone is nearby if needed. • Do not confront the individual. Let the person speak and as above, try to summarize what their concern is in a neutral and calm manner. Never be sarcastic or make the person feel they have been demeaned. Try to help them “save face” if possible. • NEVER close in our touch the individual yourself to try to remove him/her from the area. If the person seems Dangerous: • Signal as quietly and unobtrusively as you can for help. In high-risk areas it may be helpful to have worked out pre-arranged signals or codes with co-workers. If you need help, the co-worker should alert your supervisor and/or the police if necessary. • Do not mention discipline or the police if you fear an angry or violent response. • If the situation becomes more heated or you fear violence will occur, find a way to excuse yourself and to leave the room or area for help. • Be aware of any weapons. What if there is an assault in progress? • IN AN EMERGENCY OR IF THERE IS VIOLENCE IN PROGRESS • For violent incidents or specific threats of imminent violence, call 91-1. If possible use a phone out of sight/hearing of the individual. Follow instructions. • Do not attempt to intervene physically or deal with the situation yourself. It is critical that the police take charge of any incident that can or does involve physical harm. • Get yourself and others to safety as quickly as possible. • If possible, keep a line open to police until they arrive. • While most of these involve institutional settings, what if a stalker or violent patient attacks at your office? Follows you? • Or • Learns where you live? Dr. Jim Trent Continues to Recover - by Ellen Slicker, PhD and David C. Mathis, EdD • We were all shocked and saddened to learn of one of our professional colleagues being a victim of violence. On January 20, 2001, Jim Trent, PhD, Licensed Psychologist, was shot at his home by an individual he had recently evaluated for “Fitness for Duty.” Dr. Trent innocently opened the door for who he thought was one of his son’s friends. Instead, the man raised a firearm and shot three times. • Dr. Trent was struck twice; once in the right chest and once in his temple. The perpetrator of the shooting, who may have been under some chemical influence, sped away from the crime at an excessive rate of speed, ultimately crashing into a tree, which killed him instantly. Initially, Dr. Trent had severe aphasia, but made rapid improvement. Lately his progress has reached somewhat of a plateau that is at times frustrating to him. He receives physical therapy and speech therapy twice a week. Dr. Jim Trent Continues to Recover - by Ellen Slicker, PhD and David C. Mathis, EdD • While he had previously highly valued the ability to preserve normalcy in his life, he now places a greater emphasis upon protecting the privacy for himself and his family. Another area that he has examined is the type of clinical work he is accepting. Dr. Trent believes that psychologists should recognize and exercise their own choices rather than feeling compelled to “help” everyone. Especially for psychologists in private practice, it is important to recognize limits of resources when dealing with difficult clients. A full recovery is expected for Dr. Trent although he told his wife that he won’t be doing any more “Fitness for Duty” evaluations in the future. Dr. Trent and his family greatly appreciate the support they have received from the community. If threatened called 911 – ………….then what? Psychological Aspects of Firearm Safety •"Criminals are afraid of only two things: Big dogs and guns. They stay away from cops because cops have both." - Ayoob •“Grrrrrr….” - Rocky