Investigations of the Bacterial Pathogenesis of the Ilioanal Reservoir
advertisement

The Management of
Pouchitis and Cuffitis
Dr. Matt. Johnson
Prof R.J.Nicholls
Dr. A.Forbes
Prof P.Ciclitira
Proctocolectomy
UC
10-20% all UC patients
For medical refractory disease or dysplasia
FAP
Mean age at diagnosis of cancer = 39y
A Pouch
Pathological changes within a
normal Healthy Pouch
6/52
6/12
plasma cell infiltration
raised eosinophils
Later = lymphocyte infiltration
Villous atrophy
>6/12
“Normal adaptation” with cell influx stabilizing
Tendency to colonic metaplasia “colonic type mucosa”
Pouch Flora
Prox
jejunum
Ileum
Pouch
Caecum
103 (cfu/g of dry stool)
105-8
107-10
1011-12
{Nicholls RJ, 1981}{Tabaquhali S, 1970}
Pouch Flora
The proportion of anaerobes increases distally
Ileum =
1:1
Caecum =
1000:1
(Anaerobe : aerobe)
{Philipsin, 1975}
Ileal Pouch =
100:1
Colonic type flora (bacterioides, bifidobacteria)
{Shepherd NA, 1989}
Bowel Flora
10x as many bacteria as cells in the body
1kg of our weight
55% of stool
“the neglected organ”
{Bocci V,1992}
Bacterial profiles are genetically determined and
remain stable lifelong
{Farrell RJ,2002}
{van de Merwe JP, 1988}
Pouchitis
Endoscopic Findings in Pouchitis
Oedema
Granularity
Friable
Loss of vascular
Mucosal exudates
Ulceration
These changes can be patchy
Inflammation is often worse in the posterior/dependent
segment of the pouch)
Histological Pouchitis Definitions
1986 Moskowitz Histopathological Scoring System
> 4 = Pouchitis
Acute
Acute PMNC infiltration into the crypts and surface epithelium (3/3)
1. Mild
2. Moderate + Crypt Abscesses
3. Severe + Crypt Abscesses
Superficial ulceration (3/3)
1. <25% of field
2. 25-50%
3. >50%
Chronic
Chronic (lymphocytic) infiltration (3/3)
Degree of villous atrophy (3/3)
Pouchitis Symptoms
A) Post Op Stool Frequency
B) Rectal Bleeding
C) Faecal Urgency* +/- Cramps
D) Fever (unusual)
* usually due to inflammation at the distal/efferent limb of the
pouch
There is often poor correlation between symptoms and either
the endoscopic or histology appearance
Pouchitis Disease Activity Index,
Sandborn 1994
>7 = Acute Pouchitis
Clinical Pattern
After 6/12 patients fall into 3 catagories;
1.
No pouchitis (45%)
Episodic Pouchitis (42%)
Chronic Pouchitis (13%)
2.
3.
= > 4/52
Relapsing / Remitting (>3-4 a year)
Antibiotic Dependent
Persistent / Refractory Pouchitis
Causes of Pouchitis
Known Causes of Pouch Inflammation
Crohn’s
Ischaemia
Radiation
Specific pathogenic infections (CDT, CMV)
Localised infection (pelivic abscess)
?Reaction to secondary bile acids
?Stasis (no association found)
Dysbiosis (alteration in the balance of the normal bowel flora)
Bacterial Aetiology for IBD - UC
In 1989 a case report with active refractory UC
Rx= Antibiotics and an enema of “normal” faecal bacteria
Benefits were maintained for 6 months
{Bennet JD, 1989}
Antibiotics
Reduce severity and duration of UC
{Dickinson RJ, 1985}{Mantzaris GJ, 1994}{Turunen UM, 1998}{Present DH, 1998}{Cummings JH, 2001}
Improve Pouchitis - endoscopy and histology
{Madden MV, 1994}{Kmiot WA, 1993}{Hurst RD, 1996/8}{Shen B, 2001}{Scott AD, 1989}{Gionchetti P,
1999}{Mimura T, 2002}
Treatment of Acute Pouchitis
1.
Metronidazole 1-2g PO for 7/7{MaddenMV,1994}
55% SEs = N+V, abdo discomfort,headache, skin rash,
metallic taste, disulfiram like reaction with Xol, peripheral
neuropathy
3.
Metronidazole suppositories (40-160mg/d) {Isaacs 1997}
Ciprofloxacin 500mg bd PO 7/7 {Shen 2001}
7/7 course < 14/7 course < combination
2.
Cipro + Metro {Mimura T, 2002}
Cipro + Rifampicin {Gionchetti P, 1999}
Prophylactic doses (increased resistance)
Other Treatments to Consider
1.
2.
3.
Pentasa 2g bd PO {Tytgat GN,1988}{Shepherd NA, 1989}
Budesonide 9mg PO {Shepherd NA, 1989}
Budesonide suppositories {Boschi, 1992}
4.
5.
6.
60% relapse
Azathioprine {MacMillan 1999}
Bismuth Subsalicylate {Tremaine 1998}
Glutamine / Butyrate (SCFA) enemas/suppos
{de Silva HJ, 1989}
7.
Allopurinol 300mg bd PO {Levin KE, 1992}
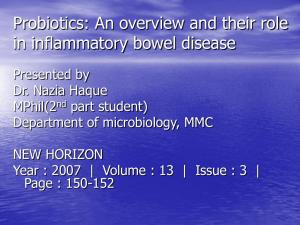
Probiotic Therapy for Pouchitis
VSL 3 (Gionchetti 1994)
4x lactobacilli
3x bifidobacteria
1x Strep Salivarius
1x S. thermaphiles
Remission can be maintained in 92.5% at 9/12 Vs
0% in the placebo group
Probiotic Trials in Acute Pouchitis
High dose of probiotics is effective in the treatment of mild pouchitis. A pilot study.
Amanidini C, Gionchetti P et al. Digestive and Liver Disease 2002; 34 (Suppl. 1):A96
Abstract
Positive results
NB = Not written up into a paper ?why
Probiotic Trials in Chronic Pouchitis
Oral bacteriotherapy as maintainance therapy in patients wih chronic pouchitis: a double blind placebo
controlled trial. Giochetti P, et al. Gastroenterology 2000; 119:305-309
40 Patients
Placebo
6g VSL 3
n = 20
n = 20
n = 20
Relapse
n=0
Remission
after 9/12
n=3
n = 17
Trials of Probiotics as Prophylaxis
Prophylaxis of pouchitis onset with probiotic therapy: a double blind placebo controlled trial.
Giochetti P, et al. Gastroenterology 2000; 124: 1202-1209
40 Patients
Placebo
6g VSL 3
n = 20
n = 20
n=8
Pouchitis
40%
n=2
10%
n = 12
Remission
n = 18
60%
after 12/12
90%
Probiotics as od Maintainance
Once daily high high dose probiotic therapy maintaining remission in recurrent/refractory pouchitis.
Mimura T, et al. GUT 2004; 124: 108-114
36 Patients
Placebo
6g VSL 3
n = 16
n = 20
n = 15
Pouchitis
93%
n = 2, +1
15%
n=1
Remission
n = 17
7%
after 12/12
85%
Probiotic Therapeutic Mechanisms
Increasing the acidity (increases SCFAs)
Altering the hosts immune response at the GI mucosa
Produce antibiotic like substances (bacteriocins)
Increased IgA + IL 10 (anti-inflammatory)
Decreases IFNg and TNFa (pro-inflammatory)
Induces T cell shift towards Th2 (anti-inflammatory)
May competitively inhibit adherence of potentially pathogenic
bacteria
Increase intestinal mucus production
Produce SCFAs and vitamins
What’s on Offer
Name
Strain
Implant
Uses
Saccaromyces
boulardii
Yes
Diarrhoea
Prevention + Rx
Actimel
L.casei strain DN114001
Yes
Stoneyfield
Yogurt
L.reiteri
Yes
Arla
L.acidophilus NCFB
1748
Yes
L.rhamnosus VTT
E-97800
Yes
PrimaLiv
L.rhamnosus 271
Yes
Yakult
L.casei strain
Shirota
Yes
Culturelle
L.casei GG
Yes
CDT
Pro Viva
L.plantarum 299v
Yes
IBS
Diarrhoea Rx
VSL#3 Trial in Chronic Pouchitis
Recently managed to acquire funding for 10 local
patients to receive 1 year of VSL#3
May be able to import for GPs who are prepared to pay
The group will be closely monitored to assess
Cost / Benefit ratio
Primary Culture Assays and PDAI before and 3/12
Assess long term outcome
If successful we will assess the effects of terminating
after 3-6/12
Where’s the Future Heading
Pre-biotics
“Non-Digestible Food (NDF) ingredients that beneficially
effect he host by selectively stimulating the growth and/or
activity of one or a limited number of bacteria in the colon,
that can improve host health” 1 {Gibson G. 1995}
Such CHO – soluble fibre
A) Encourages growth of beneficial (saccharolytic) bacteria
B) Attract harmful (proteolytic) bacteria away from mucosa
(gut wall) by saturating the adhesin-CHO binding sites
Prebiotics Side Effects
Flatulence + Bloating
Rx = Gradually increase fibre with time
Gradual increase in Bifidobacterium
Decrease freely available NDF
Decreases gas formed by other bacteria
Prebiotics and the Pouch
Inulin 24g a day for 21/7 (crossover trial)1
Decreased inflammation in 19/19
pouches
1.
Welters C. et al. Effect of dietary inulin supplementation on
inflammation of pouch mucosa in patients with ileal pouch
anal anastamosis. Diseases of the colon and rectum 45: 621627
Natural Prebiotics
Nutraceuticals = “functional foods”
Inulin / Fructo-oligosaccharides / Lactulose
Transgalacto-oilgosaccharides
Chicory (boiled root = 90% inulin)
Jerusalem artichoke
Onion
Leek
Garlic
Asparagus
Banana
(cereals eg. Oatmeal)
Proportion of pouch patients with nutritional deficiencies
70
60
50
40
Number
of patients
Normal
Deficient
30
20
33%
10
26%
15%
8%
14%
0
Hb
Iron
Folate
B12
Vit D
Conclusion
Pouch histology can help guide the medical
management
Acute pouch inflammation associated with
Chronic pouch inflammation associated with
Anaemia
Iron deficiency
Folate, Vitamin D and B12 deficiencies
Benefits of correcting deficiencies
Prevent potential long term complications
Anecdotal considerable improvement in the QOL
FAP Pouches
Healthy
Inflamed
Chart 1
Percentage of FAP Pouches with Histological Evidence of
Significant Acute, and Mixed Inflammatory Changes
35
55 of 190 had evidence of
endoscopic inflammation
30
25
20
15
10
5
0
Acute
Chronic
Mixed
Histological Inflammation
Chart 2
Percentage of FAP Pouch Patients with PDAI Scores
Diagnostic of Active Pouchitis
Of those 55, 14% had a
PDAI of >7 suggestive of
active pouchitis
50
%
40
30
20
10
0
Histology Endoscopy Clinical
PDAI
PDAI Score and its Individual Components
This gave an overall
prevalence of pouchitis in
FAP pouches as 4%
Cuffitis
Almost exclusive to those with a stapled
anastamosis
There is a 60% risk of leaving residual rectal
mucosa behind when stapling a pouch with a
1-2cm anal transition zone
Even after mucosectomy there is a 20% of
residual islands of rectal mucosa left on the
rectal cuff
Cuffitis Symptoms
1.
2.
3.
4.
Urgency
Diarrhoea (Frequency)
Burning Pain (pre/post-defecation)
Tenesmus
Treatment of Cuffitis
Is similar to the treatment of proctitis
1.
2.
3.
Mesalazine suppositories / enemas
Predsol suppositories / enemas
? Lignocaine gel
Consider
Metronidazole suppositories
Pre – Pouch Ileitis
1.
2.
3.
Pentasa granules / PO
Azathioprine
Other Immuno-modulators