Title Goes Here Title Goes Here
advertisement
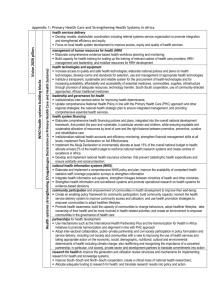
India's HRH Challenge: Initial Findings and Next Steps Peter Berman Lead Health Economist, HDNHE Human Resources for Health, May 28, 09 India HNP in partnership with the Public Health Foundation of India Thanks to Shomikho Raha, Krishna Rao, Aarushi Bhatnagar and others. Background WHO reports India as HRH deficit country with <2.3 health workers/10,000 population GoI launches National Rural Health Mission in 2005 – major scale up of basic health services 2005 public sector has significant deficit of key health workers relative to official norms NRHM issues Indian Public Health Standards (IPHS) – significantly increasing norms States provided some flexible financing for HRH recruitment and contracting India AAA: HRH for More Effective Health Systems Proposed multiyear work CMU emphasis on flexible, applied work with country engagement and policy value Link to states (who control HRH policies) Phase 1: • Measuring the health workforce • “Political Economy” analysis in two states of HRH policy implementation • Exploratory studies of medical and nursing students’ attitudes and career expectations Phase 2: • Intervention evaluation • DCE modeling Partnerships Collaboration with the Public Health Foundation of India Engage National Health Systems Resource Center Links to states where Bank already engaged with state-level operations: UP and TN India: Size and Composition of the Health Workforce Health Worker Density - All India This chart has the basic color palette to use for charts (Per 10,000 Population) You can use this chart and update data or import new charts Allopathic Physician Nurse & Midwife AYUSH Dentist Pharmacist Others Other Traditional All Health Workers 0 2 4 6 NSSO 8 10 12 Census 14 16 18 20 Government Source: National Sample Survey Organisation (NSSO) 2004-05; Census of India 2001; Medical and Nursing Councils of India; Government of India, Central Bureau of Health Intelligence Others = Dietician & Nutritionist, Opticians, Dental Assistant, Physiotherapist, Medical Assistant & Technician and Other Hospital Staff; Other Traditional = Traditional Medicine Practitioner, Faith Healer India: Public-Private Distribution of Health Workforce Distribution of Health Workforce by Sector Rural Urban Allopathic Physician Allopathic Physician Nurse & Midwife Nurse & Midwife AYUSH AYUSH Dentist Dentist Pharmacist Pharmacist Others Others Other Traditional Other Traditional All Health Workers All Health Workers 0 20 40 60 80 Percentage Non-Government 100 Government Source: National Sample Survey Organisation(NSSO), 2004-05 0 20 40 60 80 Percentage Non-Government 100 Government India: Health Workforce Density across States Health Worker Density (Per 10,000 Population) JAMMU & KASHMIR HIMACHAL PRADESH PUNJAB CHANDIGARH UTTARANCHAL HARYANA DELHI ARUNACHAL PRADESH SIKKIM UTTAR PRADESH RAJASTHAN BIHAR ASSAM NAGALAND MEGHALAYA MANIPUR JHARKHAND WEST BENGAL MADHYA PRADESH GUJARAT TRIPURA MIZORAM CHHATTISGARH ORISSA DAMAN & DIU D&N HAVELI MAHARASHTRA ANDHRA PRADESH GOA KARNATAKA PONDICHERRY LAKSHADWEEP 10 16 22 37 - 16 22 37 65 Source: Census of India 2001 TAMIL NADU KERALA A&N ISLANDS Health Workers and Health Outcomes Measles Immunization 80 100 Infant Mortality Tamil Nadu 80 UP Kerala 60 Gujarat Delhi 40 40 Gujarat Immunized (%) 60 Bihar Goa Bihar Kerala Goa 5 10 15 20 25 30 Physican, Nurse and Midwife Density(Per 10,000 Population) Source: Census (2001), NFHS-3 2005/06 Note: Size of circle proportional to per capita government health spending 20 20 Nagaland 5 10 15 20 25 30 Physican, Nurse and Midwife Density (Per 10,000 Population) Source: Census (2001), NFHS-3 2005/06 Note: Size of circle proportional to per capita government health spending Institutional Factors State governments vary widely in ability to translate funds in budget into health workers on the ground • Health departments don’t recruit – public service commission does • In UP 18-24 months from approval of posts to appointment letters – majority of • candidates no longer available/interested at time of appointment In TN some creative solutions… Institutional Factors (2) Contractual workers seen as solution, but also bring problems • In UP, civil service doctors sued state government for unfair employment of • contract doctors – as a result all contracting suspended In TN, successfully implemented ….. Institutional Factors (3) Increasing supply of key health workers constrained by conflicts between central and state regulators • In UP, most government nursing colleges de-certified by central authorities • Lack of promotional movement for faculty • Insufficient faculty for student intake • 3 year colleges admit one class and keep for 3 years • ANM schools closed due to lack of funding since late 1990s • Chhatisgarh instituted 3-year medical assistant degree – struck down by central regulators Career Preferences Medical Students 90% of final-year MBBS intend to pursue PG Course • MBBS alone qualifies them inadequately to practice • Prepared to spend 2/3 years in PG attempts Key Job Characteristics preferred • Salary • Importance to utilizing skills learnt • Good living conditions Medical Students’ Preferences for the Private Sector Greatest benefit of being a Govt. Doctor: Job Security Career Preferences Nursing Students More amenable to entering the job market after GNM • Low likelihood of gaining a seat in B.Sc. Nursing • Seeking a job abroad was much more popular (But B.Sc. is essential for this) Key Job Characteristics preferred • Salary [Very different range from that of medical students] • Rated Job Security as the second most important Nursing Students’ Preference for the Public Sector • Pay is better than the private sector • Greater job security than the private sector • Offered fixed work timings [esp. important for women with obligations to family] Phase 1 products 3 full reports (on website) 6 2-4pp policy notes (pending GoI review) Dedicated website with reports and other links, operated by PHFI Input to annual HRH training course by NIHFW and HSPH Other publications to be determined http://www.hrhindia.org/ Phase 2 work proposed 3-way collaboration with PHFI and NHSRC. Bank mainly in supporting role Inventory of state-level efforts to increase HRH under NRHM (Alliance grant) Impact evaluation in Chhatisgarh State of use of physician substitutes in PHCs (Alliance grant) Discrete Choice Experiment (DCE) study in 3 states of physicians and nurses (HNP Anchor TF grant) Some conclusions for policy and operations Emerging opportunities for Bank work in states: Focus on institutional factors essential to address supply issues Give priority to nurses if we care about rural health outcomes – this will require changes at policy level Develop packages of incentives, recruitment, and retention strategy – multidimension