Cases 61-80 - Extras Springer
advertisement

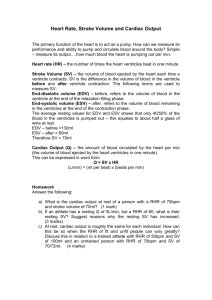
Teaching Cases JAN BOGAERT Cases 61-80 CLINICAL CARDIAC MRI SECOND EDITION Cases 61-80 ASD type secundum TOF + myocardial infarction Univentricular heart LV dysfunction in TOF patient Membranous VSD Ebstein’s Disease Complex CHD Partial non-expansion or agenesis RV Muscular VSD Uncorrected TOF Giant aneurysm of sinus of Valsalva TOF + Waterston Anastomosis Fontan circulation Corrected TOF with severe PR Persistent ductus arteriosus TOF+ severe subvalvular PS Situs inversus totalis Incidental finding of CHD in patient with severe AS Scimitar vein Decompensated TOF TOF with MAPCA’s Abbreviations Ao, aorta / AR, aortic regurgitation / AS, aortic stenosis / ARVC-D, arrhythmogenic RV cardiomyopathy-dysplasia / ASD, atrial septal defect / AV, aortic valve / CAD, coronary artery disease / CMP, cardiomyopathy / CT, computed tomography / DCM, dilated cardiomyopathy / DILV, double inlet LV / EDV, end-diastolic volume / EF, ejection fraction / ESV, end-systolic volume / HCM, hypertrophic cardiomyopathy / ICD, intracardiac device / IVC, inferior vena cava / LA, left atrium / LV, left ventricle / LVM, left ventricular mass / LVNC, left ventricular non-compaction / LVOT, LV outflow tract / MAPCA, major aortic pulmonary collateral artery / MI, myocardial infarction / MPI, myocardial perfusion imaging / MR, mitral regurgitation / MV, mitral valve / MVL, mitral valve leaflet / PAHT, pulmonary arterial hypertension / PAPVR – partial anomalous pulmonary venous return / PCMRI, phase-contrast MRI / PCI, percutaneous coronary intervention / PR, pulmonary regurgitation / PS, pulmonary stenosis / PT, pulmonary trunk / PV, pulmonary valve / RA, right atrium / RFA, radiofrequency ablation / RV, right ventricle / RVOT, RV outflow tract / STEMI, ST-elevation MI / SVC, superior vena cava / TGA, transposition of the great arteries / TOF, tetralogy of Fallot / TR, tricuspid regurgitation / US, ultrasound / UVH, univentricular heart / VSD, ventricular septal defect / WT, wall thickness. ASD Type Secundum 33-year-old woman with large type secundum ASD. Baseline cardiac MRI (left panel): LV EDV 96 ml – SV 54 ml – EF 56% / RV EDV 319 ml – SV 159 ml – EF 49%. Flow Ao 57 ml/hb – PT 178 ml/hb – Qp/Qs > 3. Dilated PT. Large, multifenestrated ASD. Normal entrance of pulmonary veins in LA MRI post ASD closure(right panel): LV EDV 127 ml – EF 75% / RV EDV 143 ml – EF 61%. Flow Ao 86 ml/hb – PT 91 ml/hb. Qp/Qs = 1. See similar case Fig. 13 Congenital Heart Disease Univentricular Heart 39-year-old man with complex CHD: congenitally corrected TGA (L-TGA), double inlet left ventricle (DILV), VSD, non-restrictive univentricular heart (UVH), dominant LV, rudimentary RV, and PS. Cardiac MRI : UVH EDV 405 ml – EF 59%, globally well preserved myocardial contractility. PS (PC-MRI: 56 mm Hg) with post-stenotic dilation of PT (57 mm). Membranous VSD 20-year-old woman with known membranous VSD, cardiac US shows gradient of 80mm Hg over VSD, no evidence of PAHT. Cardiac MRI: LV EDV 197 ml – SV 129 ml – EF 66% / RV EDV 105 ml – SV 65 ml – EF 60%. PC-MRI, Ao flow 57 ml/hb – PT 135 ml/hb, yielding Qp/Qs of 2.36. Presence of membranous VSD with systolic jet (arrow, right panel). The RV is non-dilated and non-hypertrophied while the LV EDV and SV are more than two-fold the EDV and SV of RV. See also Fig.16 and Table 5 Congenital Heart Disease Muscular VSD 73-year-old woman with history of mitral and tricuspid valve repair for MR / TR, persistence and gradual increase of dyspnea. Cardiac MRI: LV EDV 180 ml – EF 57% - SV 103 ml / RV EDV 245 ml – EF 22% - SV 54 ml. LR-shunt, flow ascending aorta 53 ml/hb – pulmonary trunk 112 ml/hb (Qp/Qs = ±2). Thinned appearance of apical ventricular septum with multi-fenestrated VSD (see dark-flow zones PC-MRI, right middle panel). Though the etiology of the muscular VSD in this elderly woman is uncertain, a myocardial infarction is the most likely hypothesis. Uncorrected Tetralogy of Fallot 38-year-old woman with tetralogy of Fallot, pulmonary valve atresia, VSD, right aortic arch, major aortic pulmonary collateral arteries (MAPCA’s). LV EDV 260 ml – EF 58% / RV EDV 290 ml – EF 44% - moderate to severe hypertrophy. Big outlet VSD (22mm). Overriding aorta. Dilated ascending aorta (51x48 mm) with moderate AR (regurgitant fraction 10%) – severe TR. Tetralogy of Fallot + Waterston Anastomosis 41-year-old woman known with Waterston anastomosis for tetralogy of Fallot, presenting with Eisenmenger syndrome, right heart failure, cardiac cirrhosis and chronic renal insufficiency. Cardiac MRI: LV EDV 128 ml – EF 47% / RV EDV 260 ml – EF 47% - severe RV hypertrophy. Large membranous VSD. Hypoplastic RVOT – hypoplastic PV. Severe TR (PC-MRI: 80 ml) with RA/IVC dilatation. Atrial septal aneurysm. Dilated aortic root. Right aortic arch with mirror-image branching. Waterston anatomosis with bidirectional flow (video right panels). Tetralogy of Fallot with Severe PR 22-year-old woman with surgically corrected tetralogy of Fallot (infundibular resection) send for cardiac MRI study to evaluate severe PR and RV volumes/function. LV EDV 162 ml – EF 47% / RV EDV 300 ml – EF 35 % - diffuse hypokinetic wall motion. Diastolic flattening of ventricular septum. Severe PR (PC-MRI, right panel: regurgitant volume 45 ml). Tetralogy of Fallot with Severe Subvalvular PS 11-year-old boy with surgical repair tetralogy of Fallot (infundibular patch), Melody valve for PS, presenting with residual subvalvular PS. Cardiac MRI shows muscular subvalvular PS with minimal diameter (5.5x9.5mm), and a peak velocity of 4.5 m/s (gradient of 64 mm Hg). Severe RV hypertrophy but preserved myocardial contractility (RV EDV 123 ml – EF 58%). Presence of Melody valve. Since RFA is unsuccessful, surgical resection of subvalvular PS performed, showing a prominent muscular ring in RVOT. Decompensated Tetralogy of Fallot 45-year-old man with surgically corrected TOF, admitted with diastolic heart failure. Cardiac MRI shows moderately dilated RV (EDV 240 ml) with preserved systolic function (EF 66%), presence of moderate PR (19%), TI and mild PS. Focally thickened pericardium with some compression of inferolaterobasal wall. Cardiac CT shows heavily calcified pulmonalis homograft, focally thickened and calcified pericardium constricting RV. Surgery: redo pulmonalis homograft, TV plasty and pericardiectomy. Tetralogy of Fallot + MAPCA’s 40-year-old man with uncorrected TOF, PV atresia, subaortic VSD, MAPCA’s, pulmonary hypertension, AR (3-4/4) treated with AV prosthesis, dilated ascending Ao, right aortic arch. NYHA III. LV EDV 357 ml – EF 41% / RV EDV 252 ml – EF 42% - severe RV hypertrophy. AR 27%, dilated aortic root 56 mm, complete agenesis RVOT - PV. Multiple MAPCA’s originating from aortic arch and descending Ao supplying pulmonary circulation. CT (performed after AV replacement) nicely shows the number, origin, and course of the MAPCA’s. See similar case Fig. 22 Congenital Heart Disease Tetralogy of Fallot + Myocardial Infarction (1) 43-year-old man with corrected TOF presenting extensive inferior MI (late presentation), secondary MR and heart failure. LV EDV 280 ml – EF 32%, thinning of entire LV inferior wall with a-dyskinetic wall motion. RV EDV 279 ml, EF 32%, moderate to severe hypokinesia. Severe MR and TR, small PR. Small LV apical thrombus. Tetralogy of Fallot + Myocardial Infarction (2) Late Gd imaging shows almost complete transmural enhancement of LV inferior wall (segments 3,4,9,10,15)(arrows, right panels). Enhancement of anterolateral LV papillary muscle (arrowhead right panel) Small apical thrombus (arrowhead, middle panels). Severe MR and TR (arrows, left panel). LV Dysfunction in Fallot Patient (1) 35-year-old man with history of surgical repair for tetralogy of Fallot, presenting with LV dysfunction, and presence of emboli in LCx and distal LAD coronary artery. Cardiac MRI: LV EDV 198 ml - EF: 37% - hypokinesia in ventricular septum and in (thinned) lateral wall. RV EDV 185 ml – EF 47%. Moderate PS (36 mm Hg) and PR (34%). Late Gd imaging shows extensive transmural enhancement in anteroseptal wall (segments 2,89,14,17) and lateral wall (segments 5,6,11,12,16) with presence of microvascular obstruction. Enhancement of the RV anterior free wall. Findings of acute extensive infarction in two perfusion territories. No etiology for the emboli found. LV Dysfunction in Fallot Patient (2) Follow up MRI study, 4 months after, shows adverse RV and LV remodeling, RV EDV 234 ml – EF 38% / LV EDV 239 ml – EF 30%. Thinning of the infarcted areas with disappearance of microvascular dysfunction. In particular the LV lateral wall has become dyskinetic (whereas initially severely hypokinetic). Ebstein’s Disease 4-year-old girl with Ebstein’s disease. Apical implantation (41 mm) of septal leaflet of tricuspid valve with atrialization of RV. Secondary TR (2/4). Small perimembranous VSD. Small PFO. See similar case Fig. 35 Valvular Heart Disease Complex CHD 54-year-old man presenting with complex congenital heart disease (CHD): situs solitus, levocardia, double discordance, VSD with bidirectional shunt, Ebstein malformation. Severe pulmonary hypertension. LV EDV 391 ml – EF 50% - diffuse hypokinesia / RV EDV 491 ml – EF 26% diffuse hypokinesia. Severe TR. Massive dilatation of both atria. Partial Non-Expansion or Agenesis of RV 32-year-old woman with Ebstein’s disease and Glenn surgery (SVC to right PA, RV to left PA). Closure of ASD type II. Impression of excluded RV apex by muscular structure. Cardiac MRI shows severe hypertrophy of trabecular/muscular structures in RV apex (arrow) with almost complete obliteration of the cavity. Presence of a notch between basal and apical part of RV (arrowhead). Severe dilatation of RV, IVC and coronary sinus. Important TR (28 ml/heart beat). Surgical repair of displastic tricuspid valve and resection of muscular structures in RV apex. Giant Aneurysm of Sinus of Valsalva 57-year-old woman with incidental finding of annulo-aortic ectasia (max. 56 mm). The patient mentions a history of car accident (eight years before). Cardiac MRI shows giant aneurysm of sinus of Valsalva orginating from noncoronary cusp (diameter 58x34 mm) prolabating in RA. No evidence of rupture of aneurysm. Moderate AI. Surgical resection of aneurysm and aortic valve replacement. Fontan Circulation 40-year-old man with history of large inlet VSD, hypoplastic bipartite RV without apex, TGA, PS, TR. Right aortic arch. Fontan total cavo-pulmonary connection (TCPC) at age 19 years. Cardiac MRI EDV 127 ml – SV 72 ml - EF 57% (combined RV/LV). Dilated aortic root, flow ascending aorta: 68 ml/hb. Inferior cavopulmonary connection (arrow right middle panel): flow 44 ml/hb. Superior connection (arrow, right panel): flow 26 ml/hb. Flow right PA 41 ml/hb – left PA 34 ml/hb. Patent Ductus Arteriosus 39-year-old man with unsuccessful closure of patent ductus arteriosus (age 12 years), currently presenting with Eisenmenger syndrome (Hct 70%, sat. 60%). NYHA class III. Small intramuscular VSD. Cardiac MRI: LV EDV 116 ml – EF 32% / RV EDV 236 ml – EF 27% - severe RV wall hypertrophy. Inversion of ventricular septum with paradoxical motion. Severe TR (39%), moderate MR (26%) and AR (18%). Dilated RA. Patent ductus arterious (22 mm) with bi-directional shunt. Dilatation of proximal descending aorta (40 mm). Dilated pulmonary trunk. Situs Inversus Totalis 37-year-old woman with dextracardia and situs inversus totalis. Cardiac apex oriented to right side. Right-sided position of morphologic LV. Normal atrioventricular and ventriculoarterial concordance. Right-sided aortic arch. Normal ventricular volumes and systolic function. Left-sided position of liver, right-sided position of spleen. Incidental Finding of CHD in patient with severe AS 50-year-old woman presenting with dyspnea (NYHA II-III), history of aortic coarctation (coarctectomia) and progressive AV stenosis. Cardiac US shows severely degenerated AV valve with PIG of 70 mm Hg and calculated AV orifice of 0.5 cm2. Cardiac MRI: dilated RV (EDV 239 ml – SV 144 ml – EF 60%) / LV EDV 75 ml – SV 43 ml – EF 57%. Intact appearance of atrial septum but partial abnormal pulmonary venous drainage of right upper/middle lobe vein to SVC. Ascending aorta: 42 ml/hb – pulmonary trunk: 139 ml/hb (Qp/Qs: 3.25). Bicuspid aortic valve with peak flow of 3.2 m/s (gradient 41 mm Hg). MV prolapse. Persisting left SVC Scimitar Vein 9-year-old boy with Scimitar syndrome, PAPVR, dextrocardia, situs solitus. Large vein (‘Scimitar’ vein, arrowheads left panel) draining right lower lobe in IVC. Surgical rerouting of abnormal vein toward LA.