Dietary guidelines for the different types of Dialysis from the talk the
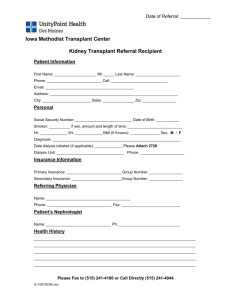
advertisement

What can I eat? Renal Dietitians Diet is an important part of your treatment, along with any medication you choose Why do I need to change my diet? • The kidneys remove waste products and excess fluid from the blood • When they do not work properly these waste products and excess fluid build up in our blood • As the levels increase other parts of our body can be affected and we can feel unwell • Altering our diet can help prevent some levels increasing too much When do I need to change my diet? • When your blood levels and/or fluid start to build up to harmful levels • Your Doctor or Nurse will let you and the Dietitian know when this happens • Alternatively you may lose your appetite and/or experience weight loss • You might see a Dietitian before starting dialysis • All people on dialysis are seen by a Dietitian What happens when I see a Dietitian? • Your diet will be individually assessed and tailored according to: • Your appetite • The type of food you normally eat • Other specific diets you may be following e.g. if you have diabetes • Your blood results • Your urine output • Your weight and height • The type of dialysis you choose Dialysis • Helps remove waste products and fluid from the blood • Unfortunately it is not as efficient as normal healthy kidneys • Usually some type of dietary modifications are necessary Haemodialysis • You attend the unit three times a week • The dialysis machine removes waste products and fluid • Waste products and fluid build up between dialysis sessions • Your diet is designed to stop these waste products and fluid getting to a level that could be harmful Peritoneal dialysis • You do this type of dialysis every day • It allows a slow continuous removal of waste products and fluid from your body • Less build up of waste products but some care with diet and fluids might be needed • A high protein intake and healthy eating are important to help maintain adequate nutrition and avoid undesirable weight gain Dietary guidelines Nutrient Recommended intake on haemodialysis Recommended intake on peritoneal dialysis Energy (calories) Sufficient to keep you at a healthy weight As for haemodialysis, but you may find weight gain a problem due to absorption of glucose (calories) from the dialysis fluid (about 320 calories a day from 4 bags) Protein (meat, fish, eggs, cheese, milk and pulses) Moderate, which may be more or less than your usual intake High, as protein is removed into the bags during dialysis Potassium (a mineral found naturally in most foods) Depends on blood levels, but intake often needs to be modified Depends on blood level, but intake less likely to need adjusting Phosphate (a mineral found naturally in protein foods, particularly in offal, shellfish, oily fish and game) Depends on blood levels, but intake is often modified. May also require phosphate binders to achieve phosphate control (see drug section) Depends on blood levels. Intake is likely to be modified. May also require phosphate binders to achieve phosphate control (see drug section) Dietary guidelines (continued) Nutrient Recommended intake on haemodialysis Recommended intake on peritoneal dialysis Fluid Depends on urine output, allowance is usually 500ml plus equivalent of your 24 hour urine output Depends on urine output and amount of fluid removed daily by dialysis (ultrafiltration). Usually more than on haemodialysis Salt Okay to use small amounts in cooking, none to be added at the table. Reduce your intake of salty and processed foods and use alternative flavourings As for haemodialysis Fibre (fruit, vegetables and wholemeal products) Normal amount to keep your bowels healthy Normal / high intake to prevent constipation, as constipation reduces the effectiveness of the dialysis Vitamins Supplements of water soluble vitamins will be prescribed routinely Supplements will be prescribed as necessary What happens when I see a Dietitian? • The aim of our advice is to keep you in the best nutritional status possible • We will give you ideas on what to eat as well as what to avoid • You may receive written information • We will give you our contact number for future queries • We will arrange follow up as needed What shall I do now? • If you have seen a Dietitian follow the advice given • Try to maintain a healthy weight • Try to eat a variety of foods to ensure a balanced diet • Aim to drink about 8 glasses/cups of fluid each day • If your appetite is reduced and you are losing weight let your Doctor, Nurse or Dietitian know as soon as possible What shall I do now? • Reducing your salt intake can help reduce your blood pressure. Try: - adding less in cooking - not to add salt at the table - to avoid salty foods, e.g. processed foods - to avoid salt substitutes - using alternative flavourings • Refer to the ‘Healthy eating for your kidneys’ information sheet in your pack for further advice How do I contact a Dietitian? • Telephone our department to arrange to speak with one of the Renal Dietitians – 01603 287011 • Leave a message with any of the renal team • Remember, you do not have to wait for a Doctor to refer you. Thank you for listening – are there any questions?