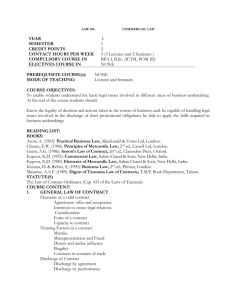
OR Refuses Discharge Plan
advertisement

Management Strategies for High Risk Patients 03/14/15 Objectives • Describe patient and situation types that should be escalated for early intervention and risk mitigation • Identify key disciplines for an interdisciplinary approach to identifying and managing high risk patient situations • Define escalation and communication strategies to mobilize systems and resources to manage high risk patient situations. 2 Sometimes You Get Really Stuck….. The Urban Legend 3 High Risk Early Escalation Triggers Potential/Actual Complex Condition Disabling/Life Limiting Condition Multiple Specialty Care Needs High Cost Medications/Outpatient Needs AND Barriers to Discharge Patient and Family Limitations/Issues Self-Pay/ Uninsurable Limited Insurance Coverage/High Co-Pays OR Refuses Discharge Plan 4 Legal/Regulatory Considerations • CMS Medicare Requirements • 42 CFR Conditions of Participation • State Requirements • Virginia Hospital Provider Manual • Follows Federal Regulations • Joint Commission Accreditation Standards • Standard RI.01.02.01: The hospital respects the patient's right to participate in decisions about his or her care, treatment, and services. • Note: For hospitals that use Joint Commission accreditation for deemed status purposes: This right is not to be construed as a mechanism to demand the provision of treatment or services deemed medically unnecessary or inappropriate. • Standard PC.04.01.03: The hospital discharges or transfers the patient based on his or her assessed needs and the organization’s ability to meet those needs. • For hospitals that use Joint Commission accreditation for deemed status purposes and have swing beds used for long term care: The written notice before transfer or discharge specified in the CoP from 42 CFR 483.12(a)(4) • Standard PC.04.01.05: Before the organization discharges or transfers a patient, it informs and educates the patient about his or her follow-up care, treatment, or services 5 Medicare Provider Regulations 42 CFR §412.42 Also Information in 42 CFR §405, 422, and 489 6 Virginia Medicaid Provider Manual; Chapter V 7 8 High Risk Process Tiered process for timely review and escalation Level I Level II Level III Ad Hoc Interdisciplinary Team Meeting Leadership High Risk Meeting CEO Meeting Goals of High Risk Process: • Ensure legal/regulatory requirements are met • • • • • 9 Appropriate Transfer of Care and/or Discharge Facilitate complicated care decisions Maintain respectful patient/family engagement Achieve clinical outcomes Mitigate financial losses Level I: Ad Hoc High Risk Team Meeting Interdisciplinary Team • • • • • • • • • • 10 Case Management Leadership Physician Advisor Social Work Leadership Financial and Business Operations Leadership Corporate Counsel Case Manager Social Worker Attending Physician/Subspecialist Consultants Nursing Medicaid Intermediary As Indicated 11 Level II: Leadership High Risk Team Meeting Supports Ad Hoc Team with decision making, allocation of resources, and work with external agents only if needed: 12 • • • • • • • Chief Medical Officer Chief Nursing Officer Chief Financial Officer Chief Legal Officer Chief Operating Officer Chief Public Affairs Officer Chief Quality Officer Defined Escalation Process • • • • • • • • 13 SBAR E-Mail Sent to Ad Hoc Team and High Risk Team Meeting When Clinical Team Available Phone Access for Non-Clinical Providers Case Management Facilitates Meeting Action Steps Outlined at Meeting Follow-up E-Mail Sent After Meeting All Escalated Cases Tracked Weekly Long LOS Rounds for Continued Tracking Case Study: SBAR S: 21 year old with Duchenne’s Muscular Dystrophy admitted on 11/29/14 with respiratory distress. Patient stable for discharge since 2/16/15 but placement limited due to age, tracheotomy, CPAP, Medicaid, and family. STM LTC has accepted the patient for transfer tomorrow but now Disability Law Center and family are raising last minute concerns about the transfer. Medicaid has denied all PICU days for past 14 days. B: Patient admitted 3 days before move into assisted living facility. Trach has disqualified him from this facility. Family unable to care for patient in their homes. Initial plan was SNF placement but patient medically appropriate for custodial care. A private individual and group home were options, but state refused funding. The placement at STM is approved by Medicaid but family cites low CMS ratings. Other facilities are further away. Team now in disagreement about discharge plan. A: 21 year with Medicaid denial has disposition plan being challenged by the Disability Law Center and family on the day prior to transfer. R: High Risk Meeting Needed to make sure the entire team is on the same page with patient transfer. 14 Case Study: Follow-Up E-Mail Today we had a meeting on the discharge plan. The plans below are in the order of the patient’s preference: 1. Discharge to Private Home with DDA Funding: The Disabilities Lawyer met with state yesterday and will hear back today. If he gets accepted he would be discharged Monday when 16 hours of nursing and home equipment can be in place. Case Management is working with agency to get PDN nurse staffing and equipment. 2. Discharge to LTC: IB in City Farther Away has accepted the patient and is the highest rated facility (4/5). They can accept the patient tomorrow (Friday) if the DDA funding does not come through. Social Work and Case Management will meet with the patient together today to review the above plan with him, and then follow-up with his family. They will keep us apprised of any barriers to discharge and any developments. 15 Case Study: Next….. The state did not make a decision yesterday and is planning to meet with patient next week. Plan to schedule transfer to IB today as that was patient’s first choice based on CMS rating. It is less convenient for the family. The expectation is this will be a temporary inconvenience as longer term options explored. Disability Lawyer on board with plan. 16 Case Study: Team Conflict Social Worker convinced patient and family to refuse discharge until permanent housing arranged Patient and family also refused to have further communication with Case Manager Team members divided on transfer Second High Risk Meeting to openly address conflicting view points 17 Follow-up Thanks to everyone for meeting with the family and the patient to present the discharge plan in a positive win-win fashion The patient and family have agreed to the transfer which will occur at 5:00 p.m. The team will be meeting to debrief on this situation to make the high risk process work better in the future High Risk Leadership Would Have Been Next Step! 18 Data Tracking High Risk CY'14 # HR Cases 44 Total Charges $15,732,046.69 Payment 4,055,150.96 % Recovered* 26% * 3 cases pending 19 DataTracking 20 Case Tracking 21 Focus On All Modes of Entry: Ambulatory The following patient submitted an application for charity and will qualify. Can you please review and let me know if there is any high risk before moving forward. Case Manager Assessment This 17 year old Guatemalan patient was seen in Eye Clinic in Sept 2014 and diagnosed with keratoconus. According to the clinic note she will probably need a hard contact lens for the affected eye. I am unsure that the child has a PCP. Will work with Community Services on resources for contact lens and reach out to family to arrange a PCP. 22 Focus On All Modes of Entry: Peri-Op Patient is schedule to go to OR tomorrow 3/03, patient’s FIC pending and an estimate of charges has been attached, Mother has been informed of the estimate amount. Case Manager Assessment The closed reduction nasal fracture for this 16 year old can be approved. Has the FAP been approved as this is unclear? The patient was seen in the ED after a volley ball injury. The patient lives in Arlington, VA. He will need follow up in the clinic post procedure. Patient has PCP. There is no added follow-up needed. FIC Response The FAP has been approved at 100%. Focus On All Modes of Entry: Emergency Department S- 11 year old uninsured from Liberia admitted from ED with left orbital mass. Patient is not eligible for charity and it is unclear what post discharge care needs will be. B- Patient presented in ED after arriving in area from West Africa on 12/14/14. Family reports eye injury 2 years ago that has grown progressively larger and obstructing vision in left eye for last 8 months. Patient went to OR on 12/14 for removal of mass. No operative note available at this time—unclear if hemangioma or tumor. It’s unclear what the post-discharge care needs will be. Social: Mother and daughter speak Krio and plan to return to their country. It’s assumed they have a Visitor’s Visa which may disqualify them from Emergency Medicaid. A - Patient at risk for not being able to receive care needed and CN at financial risk. R- Obtain input from Ophthalmology and convene High Risk meeting to discuss next steps. 24 Out of Area 25 Focus On All Modes of Entry: Out of Area From Clinic to Out of Area Team 11 year old neuro-oncology patient enrolled in a highly restricted COG study for treatment has MA Medicaid with Pilgrim Health Insurance. Study only available here at CNMC. Patient having MRI today (not covered by study) and will return next week for therapy (covered by study). I requested clinic get authorization if there are any services not covered by study but it was denied as we are out of state. From Case Management to Contracting Here is the information. I would argue for an LOA as the patient is in a very limited clinical trial where there is no in sate provider. We will not bill for anything related to the clinical trial but we do need to bill for routine care and services while she is here. So far it is the MRIs which are needed here to gauge the response to therapy. Outcome: LOA Signed 26 27 Critical for Success • • • • • • • • • 28 Compliance with Regulatory Requirements Escalation Process/Triggers Early Escalation for Discharge Barriers Rapid Response Role Accountabilities Support and Resolve Team Conflict Respect Family/Patient Requests and Concerns Good Relationships with Payers and Providers Upper Leadership Support