DEPARTMENT OF PSYCHIATRY
advertisement
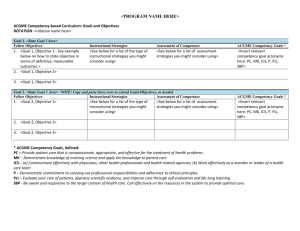
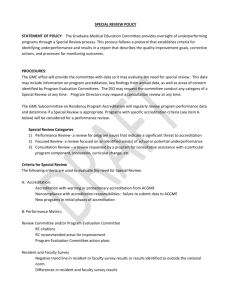
DEPARTMENT OF PSYCHIATRY The Milestone Project: An Update Carol A. Bernstein, MD Associate Professor of Psychiatry Vice Chair for Education and Director of Residency Training Department of Psychiatry NYU School of Medicine Member, Board of Directors, ACGME Beth Israel Medical Center January 14, 2013 With Much Appreciation To: Thomas Nasca, MD, MACP Timothy Brigham, PhD ACGME Staff 2 ACGME Mission Statement “We improve health care by assessing and advancing the quality of resident physicians' education through exemplary accreditation” The Social Contract Compels Educators to assure that graduates: Maintain the values and virtues of professionalism, including excellence in clinical practice, and meet society’s needs Deliver safe, affordable, quality care in a fashion that models these values and virtues, and that meet society’s evolving needs Thomas J. Nasca, MD, MACP The Actions of the ACGME must fulfill the Social Contract And ensure Sponsors that maintain: the safety and quality of care of the patients under the care of residents today the safety and quality of care of the patients under the care of our graduates in their future practice the provision of a humanistic educational environment 5 Educating Physicians who commit to: Being scientifically and clinically competent Minimizing self interest in favor of the protection and promotion of the patient’s health-related interests (Altruism) Maintaining and passing on medicine to future patients, physicians, and society as a public trust, not a merchant guild McCullough, L. The Ethical Concept of Medicine as a Profession. Advances in Bioethics, Volume 10, 17-27. 2006. Thomas J. Nasca, MD, MACP, modified by Timothy P. Brigham Why change now? 7 Brief History Late 1990’s: ACGME/ABMS Competencies developed ACGME requires: Competency framework for curriculum Phased incorporation of competency evaluation Culminates in “competency based accreditation” The “field” left to develop “tools” for the “toolbox” ABMS organizes individual certification in Competency framework Initial Certification Maintenance of Certification Tools developed that may be relevant in GME phase T. Nasca, MD, MACP, 2011 The 2005 ACGME Strategic Plan : 1 At its November 2005 retreat, the ACGME Executive Committee endorsed four strategic priorities designed to enable emergence of the new accreditation model: Foster innovation and improvement in the learning environment Increase the accreditation emphasis on educational outcomes Increase efficiency and reduce burden in accreditation Improve communication and collaboration with key internal and external stakeholders 1 ACGME 2005 Strategic Plan 9 External Pressures 2009 - House of Representatives Codifies “New Physician Competencies” Changing Public Expectations: IOM, MedPac, Macy Reports CMS encouraged to modulate IME payments based on competency outcomes Pressures on the GME System Recognized need to move from “circumstantial” to “intentional” practice in resident education 10 Never be afraid to try something new. Remember that amateurs built the ark, and professionals built the Titanic. Anonymous 11 What Currently Drives the Structure and Content of our Residency Programs? 12 What Will Drive the Structure and Content of our Residency Programs in the Near Future? 13 “One definition of insanity is doing the same thing over and over again, but expecting different results.” Rita Mae Brown Sudden Death, 1983. p. 68 The Conceptual Change From… The Current Accreditation System Rules Corresponding Questions “Correct or Incorrect Answer” Citations and Accreditation Decision 15 The Conceptual Change To… The “Next Accreditation System” 16 Goals of the “Next Accreditation System” (NAS) 17 Goals of NAS: To foster the development of realistic outcomes To free good programs to innovate To help weak programs to improve To reduce the burden of accreditation To provide accountability for outcomes to the public 18 NAS in a Nutshell Continuous Accreditation Model – annually updated Based on annual data submitted, other data requested, and program trends Scheduled Site Visits replaced by 10 year Self Study Visit Standards revised every 10 years Organized by: Structure Resources Core Processes Detailed Processes Outcomes 19 20 Phased Implementation Phase 1 Specialties (and Subspecialties) Internal Medicine Pediatrics Emergency Medicine Diagnostic Radiology Urology Orthopedic Surgery Neurological Surgery Phase 2 Specialties (and Subspecialties) All Other Specialties Institutional Review Transitional Year Implementation Timeline PHASE 1 PHASE 2 Ceased routine Site Visits First round of CLER visits (underway) Will cease routine Site Visits PHASE 1 Will begin Continuous Accreditation 9/2012 1/2012 7/2013 (through 6/2014) 7/2012 1/2013 7/2014 PHASE 2 Will enter “preparation year” PHASE 1 Entered “preparation year” PHASE 2 New Policies and Procedures take effect (7/1/2013) CLER = Clinical Learning Environment Review Will begin Continuous Accreditation Essential Elements Continuous (as opposed to Periodic) Accreditation Increased Focus on Outcomes Enhance flexibility of programs to innovate Standardization Balanced with Specialty Specificity Increased Emphasis on Patient Safety and Quality Improvement Enhanced Continuity Across the Spectrum of Training Transparency Enhanced Institutional Accountability Thomas J. Nasca, MD, MACP “Every system is perfectly designed to yield the result it produces.” The Building Blocks of The Next Accreditation System 25 Trended Performance Indicators Annual ADS Update Program Attrition – Changes in PD/Core Faculty/Residents Program Characteristics – Structure and Resources Scholarly Activity Board Pass Rate – Rolling Rates Resident Survey – Common and Specialty Elements Clinical Experience – Case Logs or other Faculty Survey – Core Faculty Semi-Annual Resident Evaluation and Feedback Annual Sponsor Site Visit (CLER) – Every 18 Months 26 ACGME Goals for Milestones Accountability for effectiveness of educational programs in producing outcomes Collaboration with AAMC, LCME to improve graduation level preparation Collaboration with ABMS, AHA, ACCME, others to identify areas for milestone improvement at the time of graduation from residency Milestones ACGME Goals for Milestones Outcome focused Use of existing tools and observations of the faculty Clinical Competency Committee triangulates the progress of each resident ABMS Board, Academy, Program Directors and RRC jointly define the expectations (Milestones) ABMS Board tracks the identified individual ACGME Review Committee tracks unidentified individual trajectories ACGME and ABMS are able to provide accountability for effectiveness of the educational program in producing outcomes for individual trainees T. Nasca, MD, MACP, 2012 ACGME Goals for Milestones Specialty specific normative data and common expectations for progress of individual residents Less prescriptive ACGME program requirements, lengthened program site visit cycles, less frequent standards revision Promotion of curricular innovation Enhancement of curricular and rotation design Opportunity for communication and improvement across the continuum of medical education Development of specialty specific evaluation tools and techniques T. Nasca, MD, MACP, 2012 ACGME Goals for Milestones Able to provide accountability for effectiveness of educational program in producing outcomes ACGME can work with: AAMC, LCME to focus graduation level preparation ABMS, AHA, ACCME, others to identify areas for milestone improvement at graduation from residency/ fellowship 30 Increase the Accreditation Emphasis on Educational Outcomes Specialty Specific Teams Board PD Association College RRC Residents Milestones & Core Evaluation Requirements ACGME Specialty Specific Competency Evaluation Program Requirements for reporting (Outcomes) Thomas J. Nasca, MD, MACP Modified by T. Brigham Expectations for Milestones When and where possible, identification of appropriate assessment tools/methods/systems Creation of a summary reporting document to be used by a Clinical Competence Committee in each program to report to the ACGME and Specialty Board Not to you Not for you With you! Clinical Competency 34 Clinical Competency Milestones: Observable developmental steps moving from Novice to Expert/Master Organized under the rubric of the 6 domains of clinical competency Describe a trajectory of progress from neophyte towards independent practice Articulate a shared understanding of expectations Set aspirational goals of excellence Provide a framework and language for discussions across the continuum General Competences 1) Patient Care and Technical Skill Compassionate, appropriate, effective 2) Medical Knowledge Know and can apply Can do and apply 3) Practice-Based Learning and Improvement Assessment of own patient care, evidence-based approaches, improvement 4) Interpersonal and Communication Skills Effective exchange of information and collaboration with patients, their families, and health professionals 5) Professionalism Committed to professional responsibilities, ethical principles and sensitivity to diversity 6) Systems-Based Practice Awareness and utilization of the larger context and system of healthcare in providing optimal patient care The Six Competencies, and the Continuum of Clinical Medical Education – Dreyfus (modified) Model1 Medical Knowledge Patient Care and Procedural Skills2 Interpersonal and Communication Skills Professionalism Novice Advanced Beginner Competent Proficient Expert Master Practice Based Learning and Improvement Systems Based Practice Undergraduate Graduate Continuing 1 as presented by Leach, D., modified by Nasca, T.J. American Board of Internal Medicine Summer Retreat, August, 1999. 2 Patient Care Competency modified 9/2010 by ACGME and ABMS 37 Miller’s Pyramid of Clinical Competence1 1Miller, GE. Assessment of Clinical Skills/Competence/Performance. Academic Medicine (Supplement) 1990. 65. (S63-S67 ) 38 Key Elements of Miller’s Pyramid Trained Observers Common understanding of the expectations Sensitive “eye” to key elements Consistent evaluation of a given level of performance Minimum Numbers of Quality Observations Interpreter/Synthesizer Experts Clinical Competency Committee (Resident Evaluation Committee) 39 Trajectory of Milestones 40 Clinical Professional Development 41 The Goal of the Continuum of Clinical Professional Development 42 Reporting Template Milestone of Competency Development Level 1 Level 2 Level 3 Level 4 Entry – Baseline, expected level at time of entry into residency Mid-Program Developmental levels of performance Offers road map and assurance that residents are attaining appropriate educational goals Mid-Program Developmental levels of performance Offers road map and assurance that residents are attaining appropriate educational goals Graduation – Expected level of performance at entry into unsupervised practice Level required to gain eligibility for ABMS certification Level 5 Stretch Goals – Exceeds expectations Comments: 43 Milestones: Guiding Principles Feasibility Quality Reporting • Balance costs with benefits • Manageable number of milestones • Improvement over current approaches • Meaningful & substantive • “Measurable” • Specialty-wide use of 5-level template for milestones reporting • Central data repository 44 Next Steps in the Outcomes Project Milestone definitions: Descriptions (in specific behavioral terms) of the performance level expected of a resident by a particular time during their residency Aggregation of resident performance on milestones as an indicator of overall programmatic educational effectiveness Board use as part of eligibility for certification 45 “Somebody has to do something, and it’s just incredibly pathetic fantastic that it has gets to be us.” Jerry Garcia The Grateful Dead edits, TJ Nasca Gratefully Not Dead 46 ACGME Milestone Project Team Department of Education Department of Accreditation Activities Susan Swing, PhD Vice President, Outcomes Assessment Eileen Anthony, MS Steve Nestler, PhD Senior Milestone Consultant Pamela Derstine, PhD Laura Edgar, EdD Senior Milestone Consultant Caroline Fischer, MBA Erin Axley Milestone Project Administrator Louise King, MS Erin Berryhill Milestone Project Administrator Patricia Levenberg, PhD Lynne Meyer, PhD, MPH Peggy Simpson, EdD Patricia Surdyk, PhD Linda Thorsen, MA Jerry Vasilias, PhD Clinical Competence Committee 48 Six Month Evaluations Determined by the CC Committee Grouped by Core Competency Established by Professional Consensus Part of Programmatic Self-Evaluation and Accreditation Measureable and Meaningful 49 Expert Panels Assembled by the ACGME for: Systems-based Practice Practice-based Learning and Improvement Communication Skills Professionalism Assessment ACGME EXPERT PANEL ON MILESTONES DRAFT VERSION 9-11-11 PROFESSIONALISM INTERPERSONAL AND COMMUNICATION SKILLS PRACTICE-BASED LEARNING AND IMPROVEMENT SYSTEMS-BASED PRACTICE Charge to the Panel: Develop milestones in Professionalism, Interpersonal and Communications Skills, Practice-Based Learning and Improvement, and Systems-Based Practice for adoption and/or adaptation by specialty milestone groups. Milestones were created to reflect the following expected levels of performance: Level 1 – Typical graduating medical student; Levels 2 and 3: Resident during the program; Level 4: Graduating resident; Level 5: Advanced, specialist resident or practicing physician This document is for ACGME milestone use only. Do not disseminate. Professionalism Elements of Professionalism in Internal Medicine Adheres to basic ethical principles Demonstrates compassion and respect for Patients Provides timely, constructive feedback to colleagues Maintains accessibility Recognizes conflicts of interest Demonstrates personal accountability Practices individual patient advocacy Milestones of Training Demonstrates empathy and compassion to all patients (3rd month) Demonstrates a commitment to relieve pain and suffering (3rd month) Provides support (physical, psychological, social, and spiritual) for dying patient and their families (24th month) Provides leadership for a team that respects patient dignity and autonomy (24th month) Green, et.al. Journal of Graduate Medical Education. 1(1). 5-20. 2009 Milestone Framework Competency Subcompetency (approximately 6) Developmental Milestones Narratives (approximately 5 narratives of a Dreyfus or equivalent trajectory) “If you think you’re too small to be effective, you have never been in bed with a mosquito.” Betty Reese (American officer and pilot) The “Envelope of Expectations” Professionalism: Accepts responsibility and follows through on tasks Medical School Expert Proficient Competent Advanced Beginner PGY 1 PGY 2 PGY 3 PGY 4 effectively PGY 5manages MOC Resident multiple competing tasks, and effortlessly manages complex Resident alwayscircumstances. prioritizes and willingly Is clearly identified works on multiple bycompeting peers andcomplex subordinates as and routine cases in a timely manner by support in source of guidance and directly providingdifficult patientorcare or by circumstances. unfamiliar overseeing it. In difficult circumstances appropriately seeks guidance. Is Resident frequently prioritizes regularly soughtmultiple out by peers and competing demands and completes thethem guidance. subordinates to provide vast majority of his/her responsibilities in a timely manner. Self identifies circumstances and actively seeks guidancecompletes in unfamiliar circumstances. Resident routinely most assigned tasks in a timely manner in accordance with local practice and/or policy, but still requires guidance in circumstances. Resident completesunfamiliar many assigned tasks on time but needs extensive Novice guidance on local practice and/or © 2012 Accreditation Council for policy for patient care. Graduate Medical Education (ACGME) Resident frequently fails to Professionalism recognize or actively avoids opportunities for compassion or empathy. On occasion demonstrates lack of respect, or overt disrespect for patients, family members, or other members of the health care team Resident seeks out opportunities to demonstrate compassion and empathy in the care of all patients; and demonstrates respect and is sensitive to the needs and concerns of all patients, family members, and members of the health care team. Resident demonstrates compassion and empathy in care of some patients, but lacks the skills to apply them in more complex clinical situations or settings. Occasionally requires guidance in how to show respect for patients, family members, or other members of the health care team. Thank You!