Section_3_Recommend_Modifications_Care

Initiation and Modification of
Therapeutic Procedures
Recommend Modifications in the Respiratory
Care Plan
Modifying Respiratory Care Plan
Recommending Changes in Bronchial Hygiene Therapy
Conditions where modifications would be appropriate
Preexisting conditions (e.g. increased ICP)
Recent procedures (e.g. surgery)
Patient demographics (e.g. age)
Adverse reaction to therapy ( e.g. hypoxemia)
Modifications may include
Altering the duration of therapy
Altering the positions used
Using a different bronchial hygiene strategy
Bronchial Hygiene Modification
Shorten the duration for a given postural drainage position for patients who become anxious or otherwise do not tolerate the procedure.
Avoid a head-down position for patients with elevated ICP and instead rotate the patient laterally to approximate the position as closely as possible.
Discourage strenuous coughing for stroke patients or those otherwise predisposed to increased ICP. Instead, instruct these patients to use a “huff cough or sit them up until the cough subsides.
If you think a patient might become hypoxemic during the procedure, provide appropriate supplemental O2 and monitor the SpO2 throughout the procedure.
If bronchospasm occurs, stop therapy, return patient to original position monitor him or her closely, administer supplemental O2, contact physician, and recommend bronchodilators.
If complications or adverse events occur during the therapy
(e.g. hypoxemia, arrhythmias), stop the therapy, return the patient to the original position, monitor him or her closely, administer oxygen as necessary, and promptly contact the physician.
Recommending Changes in Patient Positioning
Proper positioning can optimize patient care by enhancing oxygenation and ventilation, assisting with secretion removal and other therapeutic procedures, as well as facilitating diagnostic procedures.
Recommending Insertion and/or Modifications of Artificial
Airways
Based on patient assessment and the major indications for insertion of the various forms of artificial airways (oro- and nasopharyngeal airways, LMA, oral and nasal ET tubes, cuffed/unfenestrated and uncuffed/fenestrated tracheostomy tubes, tracheostomy button)
Recommending Treatment of a Suspected Pneumothorax
Placing the patient on 100% oxygen therapy
Ordering a stat chest x-ray
Doing a needle decompression in the appropriate side if the patient’s condition becomes life threatening.
Change ventilator settings to minimize peak inspiratory airway pressures and barotrauma (e.g. decrease or eliminate
PEEP, decrease flow, or lower Vt)
Recommending Adjustment in Fluid Balance
Maintaining balance between intake and output is essential to maintain proper metabolic functions.
Recognize signs of and suggest strategies to treat dehydration
(negative I/O) and overhydration (positive I/O)
Recommending Adjustment of Electrolyte Therapy
Know the normal electrolyte values for sodium, potassium, and chloride.
Recognize common causes of low (hypo) and high (hyper) serum levels and be able to suggest actions for treatment
Recommending Initiation and Modification of Pharmacologic Therapy
Know indications for use of respiratory medications
Suggest initiation, modification, or discontinuation of respiratory medications based on patient situation.
Bronchodilators – short and long acting
Beta adrenergics
anticholinergics
Inhaled steroids, systemic inflammatory mediators
Mucolytics
Inhaled alpha adrenergics
Airway anesthetizers
Sedation for patient-ventilator asynchrony, intubation
Recommending Sedation and Neuromuscular Blockade
Know indications for common sedatives, neuroleptics/antipsychotics, analgesics, and paralytics
Recommending Changes in Oxygen Therapy
Changes in input flow, delivery device, or FiO2 to meet patient’s need.
Recommending Changes in Mechanical Ventilation
To improve patient-ventilator synchrony
Identify patient-related causes
Identify ventilator-related causes
Enhancing Oxygenation
During mechanical ventilation
If hyperoxia is present (usually PaO2>100 torr), you should lower the parameter (FiO2 or PEEP) that is potentially most dangerous to the patient at the moment.
If the PaO2 or SaO2 is low (<60 torr or <90%), hypoxemia is present, and either the FiO2, or the PEEP level should be increased.
Determining which parameter to change.
If the PO2 is greater than 60 torr on an FiO2 less than 0.6, the problem is mainly a V/Q imbalance that will respond to a simple increased in FiO2.
If the PO2 is less than 60 torr on an FiO2 greater than 0.6, the problem is shunting and PEEP/CPAP must be added or increased
Recommending Changes in Mechanical Ventilation (cont.)
To improve alveolar ventilation
Estimate changes in minute volume
Current V
E x Current PaCO
2 x Desired PaCO
Rate changes are preferred method to alter minute volume, as long as the patient’s tidal volume is properly set.
= new V
E 2
Adjusting the Inspiratory to Expiratory Time Ratio Settings
Recognize signs of expiratory airflow obstruction and relationship to auto-peep
To treat severe conditions recommend
Administering bronchodilator therapy
Keeping the airway clear/removing secretions
Increasing the ET/trach tube size (if too small)
Decreasing the I:E rato (decrease rate, increase flow, etc.)
Decreasing tidal volume/minute volume, within safe limits
Allowing the patient to breath spontaneously
Applying extrinsic PEEP, pressures up to 80% of auto-
PEEP level
Recommending Changes in Mechanical Ventilation (cont.)
Modify Ventilator Techniques
Appropriate changes of mode of ventilation based on changes in patient’s condition.
Monitoring and Adjusting Alarm Settings
Ensure patient safety
Remove the patient from the ventilator
Manually ventilate the patient
Ask for help if necessary
Assess and monitor the patient
If patient-related problem, treat and/or recommend treatment:
Suction airway
Administer bronchodilators
Check artificial airway and recommend reintubation if necessary
Troubleshoot ventilator-related problems
Fix circuit leak
Readjust alarm parameters to correct level
Once patient is stabilized and/or ventilator problem fixed, reconnect patient
Monitor patient-ventilator interface to ensure no repeat of episode.
Recommending Changes in Mechanical Ventilation (cont.)
Adjusting ventilator settings based on graphics
Recognize clinical situation as seen on waveform (patient-ventilator asynchrony, auto-PEEP, overdistention, airway leaks)
Independently initiate or recommend changes to physician
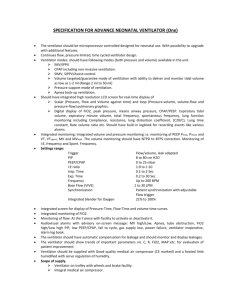
Changing type of ventilator and breathing circuit
Selecting and changing ventilators should be based on patient variables, application settings, and needed capabilities.
Selecting and changing ventilator circuits appropriate to compatibility with ventilator, soiled or malfunctioning circuit, meeting patient care objectives.
Use low-compliance circuit for neonates and young pediatric patients to minimize volume loss.
Changing or modifying a single-limb circuit by adding PEEP capabilities to the exhalation valve
Adding an additional exhalation port to a bi-level pressure ventilator circuit (e.g. whisper swivel valve) for patients at risk for
CO2 retention.
Adding 50-100 mL mechanical deadspace between the ventilator circuit’s Y-connector and the patient’s airway to raise the PaCO2 and manage acute respiratory alkalosis(generally limited to ventilator modes that do not include spontaneous breaths)
Recommending Changes in Mechanical Ventilation (cont.)
Other recommendations related to ventilator settings
Minimize ventilator-induced lung injury
Volume-targeted ventilation with low tidal volumes (4-6 mL/kg of IBW)
Volume-targeted ventilation with low plateau pressures
(< 30 cm H2O)
Pressure controlled ventilation with PIP less than 30 cm
H2O
“Dual-mode” ventilation (e.g. pressure-regulated volume control)
Airway pressure release ventilation (APRV)
Permissive hypercapnea
Appropriate clinical situations for high-frequency oscillation or jet ventilation
Lung recruitment maneuvers
Recommending Weaning From Mechanical Ventilation and Extubation
Assess patient readiness
Evidence for some reversal of the underlying cause of respiratory failure
Adequate oxygenation, e.g.
1.
PaO2/FiO2 > 150 – 200
2.
PEEP </= 5 – 8 cm H2O
3.
FIO2 </= 0.4 – 0.5
pH >/= 7.25
Hemodynamic stability (no myocardial ischemia or significant hypotension)
The capability to initiate an inspiratory effort
Interpret weaning parameters
Assess parameters collectively; if most or all of them are favorable, weaning should be recommended
A variety of weaning methods have been deemed effective in a clinical setting
One of the most widely accepted methods involves using pressure support ventilation (PSV) to obtain a VT, as tolerated by the patient, decreased to a minimum level of 5-6 cm H2O
Unwanted physiological changes, such as a respiratory rate greater than 30 or a heart rate greater than 120-140, may signal that the patient is not tolerating the weaning process and should be returned to full ventilatory support
If the patient tolerates a “T-piece trial” and has good airway protective reflexes, you should recommend that the patient also be extubated
Once a patient is extubated, you should recommend that the patient be placed on an oxygen-delivery device with an FiO2 slightly higher (10% increase in FiO2) than that which he or she was on during mechanical ventilation.
Recommending Weaning From Mechanical Ventilation and
Extubation
Post-extubation monitoring for need for reintubation / mechanical ventilation
Unstable vital signs (significant increase in respiratory rate and/or heart rate, hypo/hypertension)
Stridor
Decrease in SpO2
PaO2 less than 60 torr or PCO2 greater than 50 torr
Prolonged accessory muscle use or paradoxical breathing
Altered mental status
Hemodynamic instability
Common Errors to Avoid on the Exam
When performing postural drainage, avoid recommending a head-down position for patients with increased ICP and instead rotate the patient laterally to approximate the desired position.
Never recommend sedatives, such as benzodiazepines, to relieve pain. These drugs are often helpful in decreasing anxiety but don’t alleviate pain.
Never recommend weaning a patient from mechancal ventilation who is hemodynamically compromised, has unstable vital signs, or requires FiO2s in excess of 0.50. – 0.60 or
PEEP level greater than 10 cm H2O
Never attempt to perform CPR on a patient who is in a bed unless a “compression board” is placed under their back or the bed is in “CPR” mode
More Common Errors to Avoid on the
Exam
Never recommend prophylactic or maintenance medications such as chromolyn sodium or long acting beta-agonist bronchodilators such as salmeterol for patients experiencing a severe asthmatic episode or in status asthmaticus.
To prevent oxygen-induced hypoventilation, never recommend FiO2 much above 0.28 for COPD patients suspected of also being CO2 retainers.
Never recommend PEEP levels in excess of 5 cm H2O for ventilator patients who are hemodynamically unstable or at risk for developing a pneumothorax.
Never recommend 1:1 or inverse I:E ratios for mechanically ventilated patients who are not sedated or who are hemodynamically unstable.
More Common Errors to Avoid on the
Exam
Never initiate low inspiratory flows or short expiratory times on ventilator patients who are at risk for air trapping and auto-PEEP.
Never recommend a conventional ventilator with iron-based metals and microprocessors for use in an MRI room. Instead, recommend a pneumatically powered and controlled ventilator.
Never simply recommend sedation for patient-ventilator asynchrony before ruling out other patient causes such as bronchospasm, airway obstruction and pneumothorax, or ventilator-related causes such as insufficient inspiratory air flow or inappropriate pressure support.
Never set a low-pressure (disconnect) alarm much below 5-8 cm
H2O.
Never use a standard high-compliance circuit for neonates or young pediatric patients.
Exam Sure Bets
Always stop postural drainage in the head-down position if the patient begins to cough vigorously. Sit up and stabilize the patient before continuing with therapy.
To facilitate a difficult intubation, always consider recommending a depolarizing paralyzing agent such as succinylcholine (Anectine), which has a rapid onset and short duration.
Always recommend rapid-sequence intubation for patients with clinical signs of impending respiratory failure or inadequate airway protection.
Always consider a laryngeal mask airway (LMA) when an immediate intubation is indicated but not easily achievable or in the presence of a difficult airway.
More Exam Sure Bets
Always recommend the use of the correct-size ET tube when assisting with intubation. In general, recommend the following tube sizes: average adult male: 8.0 – 9.0; average 16-year-old: 7.0; 3-year-old: 4.5 mm (uncuffed).
Always recommend placing a spontaneous-breathing patient who is dyspneic in a Fowler’s or high-Fowler’s position, to help promote chest excursion and lung expansion.
Always recommend a fast-acting adrenergic bronchodilator for a patient with severe bronchospasm associated with asthma or a similar condition.
For patients with unstable or high minute ventilation who need a low to moderate FiO2 (0.24 – 0.50), always recommend a high-flow device such as an airentrainment mask.
More Exam Sure Bets
For patient-ventilator asynchrony, always consider and recommend measures to address both patient-related causes, such as airway obstruction and anxiety, as well as machine-related causes, such as inappropriate trigger sensitivity or inspiratory flow.
Always recommend increasing PEEP above 5-10 cm H2O for ventilator patients who are hemodynamically stable but hypoxemic despite an FiO2 in excess of 0.50 – 0.60.
Always recommend increasing either the P (IPAP-EPAP) or the respiratory rate when seeking to increase the minute ventilation for a patient on BiPAP.
Always ensure that there is appropriate full ventilatory support backup before recommending that a patient be placed on a weaning mode, such as SIMV with pressure support, CPAP or pressure support alone.
More Exam Sure Bets
Always consider recommending pressure-targeted mode or dual mode of ventilation when attempting to reduce a ventilator patient’s peak and/or mean airway pressure.
When a patient with ARDS does not respond well to conventional volume and pressure modes of ventilation, consider recommending high-frequency oscillation or jet ventilation.
When responding to a ventilator alarm, always start by checking patient causes such as disconnect or airway leak
(low pressure) or bronchospasm or secretions (high pressure).
Always disconnect a patient from the ventilator and manually ventilate him or her with 100% oxygen if a ventilator alarm can not be fixed within 15 – 30 seconds, especially if the patient is in distress.
Always insert an oropharyngeal airway if you are unable to ventilate a patient with any bag-valve-mask device.
Reference:
Certified Respiratory Therapist Exam Review Guide, Craig Scanlon,
Albert Heuer, and Louis Sinopoli
Jones and Bartlett Publishers