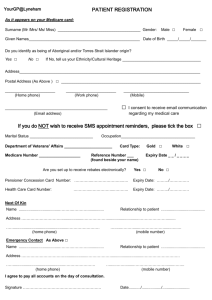
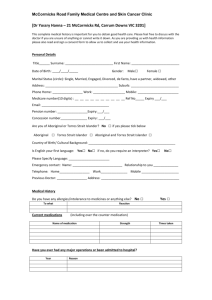
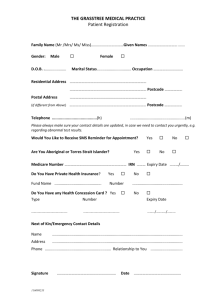
Patient consent paper
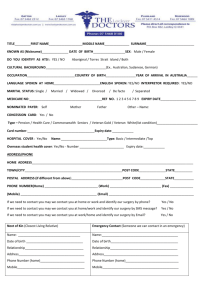
advertisement

Patient Consent Informed Patient Consent Informed patient consent is “a patient's consent to a medical or surgical procedure or to participation in a clinical study after being properly advised of the relevant medical facts and the risks involved” (dictionary.com). This issue occurs almost every day; patients who need a medical procedure done will have the doctors tell them what procedure should happen and will be more affective toward the patients. Patients and doctors are impacted the most; patients receive news that they need a procedure done and the doctors have to explain what they are going to do to the patient and let them decide if they want it done or not. Inform consent implies that there is a responsibility for the physicians to disclose information to the patient so he can make an informed decision. Some describe this as full disclosure. Total discloser is telling the patient everything about the procedure that will occur. It is hard for the patient to understand total disclosure unless they are a doctor. Full disclosure is telling the patient all they want to know about the procedure they are doing. People have different definitions of full disclosure. The federal court sided that the doctors should give full disclosure information to the patient, which means to give them enough information so they know what is about to happen to their body (Beauchamp and Walters, 1984, p. 384). In Canterbury V. Spence, a case in 1972 before the court of appeals, the patient, Canterbury, had a spinal surgery done by Dr. Spence. After the surgery, Canterbury fell and was almost paralyzed. This caused him to have another surgery on the spine. Canterbury sued Dr. Spence and the hospital because he felt that he was neglected by the staff and the doctor didn’t inform him of the risks the surgery brought. The court found the doctor not guilty because the patient did not have adequate information to tell them otherwise (lawnix.com). The pro is that the patient gets to be engaged in their own healthcare by determining what should be done with the body. With this freedom to make a choice, the doctors feel that people could never be in the position to choose unless they are doctors themselves. The patients could get so involved. They start to become fearful of what will come next. This fear could lead to patients making the wrong decisions or, choosing the thing that will only harm them not help them. The cons are that the patients can make wrong decision. The patients begin to fear. They start second guessing themselves. Feeling that even though it could save their lives, it will only make them fall. Fear stands between the patients and the life that they could live. With everything on the computer, anything can happen to files and patient records. Having these computers is a nice way to keep the records of the patient. When deciding what to do with this patient, the doctors have the patients’ records at the palm of their hands. This can be helpful for the doctors, so they can see everything that patient has taken, what may be harmful to them, and what they can handle. In my opinion, this issue rates a 4. I gave it a 4 because it is not an issue that will affect everyday life. With the situation am in, I do not have any medical issues that would cause me to make a choice. For those who are older and have bigger issue like cancer find this issue at an 8. What they choose could change their lives forever. Patient Consent Reference Beauchamp, T., Walters, L. (1989). Contemporary issues in bioethics. Wadsworth, Inc. Dictionary.com (2013). Informed Consent. Dictionary. Retrieved from http://dictionary.reference.com/browse/informed+consent Lawnix (2013). Canterbury v. spence. Lawnix.com. Retrieved from http://www.lawnix.com/cases/canterbury-spence.html