Chemical Burns & Radiation Injuries

Chemical Burns & Radiation
Injuries
Moritz Haager
Dec. 04, 2003
Objectives
Approach to chemical burns
Acids, alkali, HF
Approach to radiation injuries
Chemical & nuclear warfare agents
Perspective
> 65,000 chemicals in use; 60,000 new ones added yearly
Impossible to know each of these
Health effects mostly unknown
Important to have a general approach
Know the common agents
Important to make use of MSDS sheets & Poison Centers
Chemical Exposure
Dermal
Ocular
Inhalation
Ingestion
Systemic effects
Determinants of injury severity
Chemical agent(s)
Duration of exposure / Penetration
Concentration & pH
Type of exposure
Acids vs. Alkali
Acids
Coagulation necrosis
Coagulate proteins forming barrier to further penetration
More superficial burns
Tissues have intrinsic acid buffering capacity
Strong acids have pH < 2
Alkali
Liquefaction necrosis
Combine w/ proteins & saponify lipids
Deep ongoing tissue penetration
Difficult to access with hydrotherapy
Strong bases have pH > 11
General Approach
Prehospital
ED care
Post-ED care
Pre-hospital Management
Scene safety
Remove pt from danger
ABC’s & primary survey
Immediate decontamination
Remove contaminated clothing
Brush off dry chemicals first
Copious low pressure irrigation
Identify agent(s) & obtain MSDS sheets if possible
ED Care
Continue hydrotherapy
Strong acids: 2-3 hrs
Strong alkali: 12 hrs or more!!
Copious amounts to offset any exothermic reaction & maximally dilute
Low pressure to prevent spray contamination
ED Care
Provide analgesia
Antibiotic prophylaxis & Tetanus prn
Identify & Tx Systemic Sx
Poison center consult to guide ongoing management
Case 1
12 mo M spilled “Resolve” multi-purpose cleaner on his leg
Mom did not notice for ~15 min
Presents w/ obvious erythema and areas of excoriation on R ant leg & R wrist
Also lips red & cracked
No stridor, wheeze, or resp distress
Vitals normal, rest of exam normal
Case 1
MSDS sheet:
Ethylene glycol monobutyl ether, trisodium phosphate, nonoxynol-10 pH 12.0
Case 1
Management
Flush, flush, flush
Observe cautiously for airway involvement
IV placed for analgesia & possible airway management
Lytes incl. Mg, Ca
PADIS consult (prior to obtaining MSDS)
Case 2
17 yo M comes in c/o severe pain in all digits of his hand worsening since y/d
Cleaning rusty bicycle chain with rust cleaner y/d
Indurated, tough, whitish finger tips
Hydrofluoric Acid
Found in rust cleaners, metal cleaners
Also used for glass etching & electronics manufacturing
Dilute solutions penetrate deeply & cause delayed Sx onset & more severe burn; pain can last days
14.5% w/v immediate Sx
12% w/v Sx w/in ~ 1hr
< 7% w/v hrs before Sx develop
Hydrofluoric Acid
Mechanism of Injury
Corrosive burn (H + ions)
Chemical burn (Fluoride ions)
Penetrate tissue & form insoluble salts w/
Mg 2+ & Ca 2+
Local (tissue destruction & necrosis) & systemic effects (hypocalcemia, hypomagnesemia, hyperkalemia) arrhythmias
Concentrated HF (>50%) to 2.5% BSA has been fatal
HF: Approach
Determine type & timing of exposure
Concentration & contact time
Rule out co-exposures
Rule out & monitor for systemic effects
Cardiac monitor
Trousseau’s & Chvostek’s signs, tetany
Lytes, Ca 2+ , Mg 2+ , ECG (QT)
Tx for local & systemic toxicity
HF: Local Treatment
Copious irrigation 15-30 min
Persistent pain indicates deep penetration need to eliminate
Fluoride ion
Debride blisters & necrotic tissue
Fluoride chelation
Ocular burns
sterile water or saline irrigation (may need local anesthetic drops)
Persistent pain 1% calcium gluconate irrigation (10% solution in 10x volume of NS)
Inhalation burns
100% oxygen by mask, 2.5% calcium gluconate by nebulizer
Watch for pulmonary edema
Ingestions (Usually fatal)
Consider gastric lavage with calcium chloride (i.e., 20 mmol calcium in
1000 cc NS) if early presentation
Intubate prior to lavage
Fluoride Chelation: Calcium gluconate
*
Topical gel
2.5% = 10% Ca gluconate in 3x volume of muco or KY jelly e.g. 25 ml in 75 ml muco) in latex glove – persistent pain after 30 min indicates need for SC or intraarterial Ca 2+
Wear glove for 24 hrs
SC infiltration of 5-10% Ca gluconate at 0.5 ml/cm 2
Consider regional anesthesia b/c severe pain
Intraarterial infusion
10 ml 10% Ca gluconate in 50 ml D5W over 4 hrs into radial or ulnar artery; repeat if pain persists / returns within 4 hrs
20 ml of 20% Ca gluconate in 80 ml D5W; repeat in 12 hrs prn
Watch for pain, arterial spasm, thrombosis tissue necrosis and digit loss have occurred following extravasation of calcium salts
*NB: KCL is more irritating & damaging therefore use Ca gluconate
HF: Systemic Treatment
Evidence of hypocalcemia
10 ml of 10% CaCL IV empirically
Repeat prn
Follow w/ serial lytes & ECG until normalizes
Case 3
24 yo F grad student spilled phenol on her sleeve – brief rinse then continued to work
Presents feeling lightheaded, nauseated, and drowsy
Phenol
Aromatic acidic alcohol
Plasticizer, antiseptic, used for DNA extraction in labs
Dilute solutions less likely to cause papillary necrosis therefore tend to penetrate more quickly
Locally causes acidic burn
Systemic absorption leads to CNS depression coma & resp arrest, as well as hypotension, metabolic acidosis, hypothermia
Phenol: Treatment
Copious irrigation
Polyethylene glycol 200 or 400 or isopropyl alcohol most effective, but can use water (just use LOTS)
PEG can be used for ocular exposures
Physiologic support for systemic Sx
Tx in well ventilated room
Case 4
You are w/ MSF in the jungles of Cambodia
A young boy is brought in w/ severe burns after a friend stepped on unexploded ordinance which then blew up in a brilliant white flash killing his friend and showering him with burning debris
Phosphorus
Waxy yellow solid; spontaneous ignition in air > 34 o C
Used in munitions, insecticides, rodenticides, & pesticides
Will continue to burn on skin
Firebombing of Dresden in WWII
Primarily causes thermal burns
Systemic effects metabolic in nature
Hypocalcemia, hyperphosphatemia bradyarrhythmias
Phosphorus
Treatment
Submerse affected areas in COOL water, or cover in wet towels
Wash off w/ 5% Na bicarb & 3% CuSO
4 in 1% hydroxyethyl cellulose solution
Phosphorus particles turn black
Phosphorus particles fluoresce under UV light
Highlights
Formic acid
Bicarb for acidosis, may need HD or exchange transfusions for systemic toxicity
Anhydrous ammonia
Alkali burns
High danger of inhalational injury
Elemental metals
Na + & K + react w/ water to produce heat & H
2 gas & OH -
Remove metal fragments & place in mineral oil or isopropyl alcohol (Na + ) or terbutyl alcohol (K + )
Part II: Chemical Warfare
Agents
Why we should know this
Increased potential for terrorist use
Relatively easy to make or obtain
Most are simple derivatives of precursor compounds in manufacture of plastics, pesticides, & fabrics
Non-traditional chemical agents can be used as weapons in the right setting
Bhopal – methyl isocynate (2000 dead)
Chemical Warfare Agents
Choking (pulmonary) agents
Chlorine, Phosgene
Vesicants (Blister agents)
Mustards, halogenated oximes
Nerve agents
G agents (Sarin, tabun, soman), VX
Cyanide agents
Improvised agents
Vesicants
3 subclasses
Mustards
Arsenicals
Halogented oximes
Produce cutaneous, ocular, mucous membrane, & pulmonary burns
Less lethal (primarily kill via pulmonary involvement) but highly morbid
Effects tend to be delayed
Easy to manufacture or obtain
Mustard Agents
Sulfur mustard = prototype
Designated H, or HD
Easy & inexpensive to produce
Most dangerous agent in WWI
Low lethality (1-3%) but high morbidity
Most recent use by Iraq in Iran-Iraq war
Low volatility, high persistence
Delayed Sx onset (may take up to 12 hrs) prolonged exposure
Mustard: MOA
“Radiomimetic”
Contaminates environment
Penetrates clothing & skin easily w/o visible or perceptible effects
Precise cellular action unknown but acts similar to alkylating agents
Inhibits glycolysis cellular death
Primary tissue irritant
DNA, RNA, & protein damage
Mutagenic, carcinogenic, teratogenic
Poorly soluble in water; dissolves readily in skin oils
Predilection for moist areas of body
(eyes > resp tract > scrotum > face > anus)
Mustard: Clinical Effects
Ocular
Corneal ulceration, iritis, blindness
Respiratory
URT irritation, chemical pneumonitis respiratory failure, death
GI
N &V
Hematologic
Bone marrow suppression, pancytopenia
CVS
CV collapse, shock, death
Immune system
Immunosupression, sepsis
Dermal
Cutaneous burns
Mustard: Treatment
Decontamination
Prior to entry into medical facility
Protect workers
Remove all clothing (contaminated)
0.5% hypochlorite (bleach) irrigation
Debride & decontaminate bullae
US Military kits:
2 sets of paper towels soaked with phenol & hydroxide followed by chloramine
Adsorbents (flour, talcum powder)
Water less ideal b/c poor solubility but may use in large amounts if nothing else available
Ocular exposures should be rinsed w/ 2.5% thiosulfate sol’n & then topical abx, & cycloplegics optho consult
Mustard: Treatment
No antidote; Tx is supportive
Bronchodilators, O
2
, steroids, bronchoscopy, mechanical ventilation
Analgesia
Tx cutaneous injuries like burns
Most pts recover completely
Factors associated w/ poor prognosis
Erythema >50% BSA
Dyspnea w/in 4-6 hrs of exposure
Respiratory failure
Bone marrow suppression
Mustard Burns
Mustard as a terror weapon
Difficult to detect, delayed onset
Potent, w/ significant morbidity
Easy to make, store, transport, & deliver
Bombs, aerosol, vapour, rockets, canisters
9 openly documented manufacturing methods that can be done with high school lab supplies in someone's basement (the MDA of terrorism if you will)
Cheap
Persistent; difficult to clean up
Sig. experience in mid-east due to use in Iran-Iraq war
Halogenated Oximes
Phosgene oxime (CX, dichloroform oxime)
Also known as urticariants or nettle gases
Fair water solubility
Immediate Sx onset; unpleasant odor
No confirmed battlefield use
Penetrates clothing, rubber, & skin rapidly (sec’s)
Enhances penetration of other agents
2 proposed MOA’s
Direct injury due to corrosive effect & enzyme inhibition
Indirect injury due to alveolar macrophage activation & secondary pulmonary injury (delayed)
CX: Clinical effects
Immediate effects & absorption
Mild irritation severe pain
Skin has grayish blanched appearance & surrounding erythema which can go on to blister or form hives & pruritus
Turns brown & into dark eschar over 24h – 1 wk
Also immediate conjunctivitis & ocular pain
CX: Treatment
No antidote
Decontaminate & Supportive Care
US military
M291 decontamination kits
Flush w/ large amounts of water
Improvised Agents
Military & terrorist mission goals differ
Many chemical deemed poor for warfare more than appropriate for terror attacks
Thousands of commercial compounds can potentially become weapons
E.g. 911 – jetliners turned into bombs
CDC threat list
11 categories of diverse potential biological & chemical weapons
Underscores need for generalized approach & disaster planning
General Guidelines
Prehospital decontamination ideal
Assume decontamination has NOT occurred
Protective clothing
No PPC suit can protect against all agents, but Level A suits are best
Latex gloves useless; nitrile much better
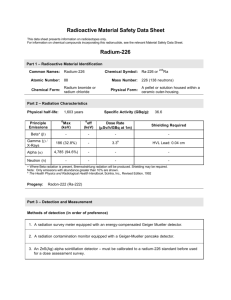
Part III: Radiation Injury
Quiz
How large were the atomic (fission) bombs dropped on Hiroshima &
Nagasaki?
Equivalent to 12,500 & 20,000 tons of TNT respectively
66, 000 people instantly died & 69,000 injured in Hiroshima
Blast radius was 3 miles in diameter
What are modern (fusion) thermonuclear warhead yields?
In the mega ton range (largest ever detonated 100 MT)
What was is the lethal radius of a 10 KT weapon? A 20 MT weapon?
3 miles vs. 35 miles
How many nuclear devices have been detonated?
A: > 2000 tests, >500 above ground
How many nuclear warheads were held at the height of the Cold
War?
Over 69,000 in 1985
How many now?
32, 000 = > 10,000 MT TNT
Basics
Ionizing radiation
Short wavelength, high frequency
High energy: 1 billion x that of non-ionizing
UV, X, & γ rays; α & β particles; neutrons
Released by unstable atomic particle decay = radioactivity
Ability to knock electrons out of orbit of other atoms (ionize them)
Ionizing Radiation
Units
SI Units
Sievert (Sv) = exposed dose or dose equivalent
1 Sv = 1 Gy
Gray (Gy) = absorbed dose
1 Gy = 1 joule energy absorbed / Kg tissue
Becquerel (Bq) = activity
Older Units
Rem = radiation equivalent man
1 rem = 0.01 Gy
Rad = radiation absorbed dose
1 rad = 0.01 Sv
Roentgen (R) = exposure
1 R = 0.01 Gy
Curie (Ci) = activity
1 Bq = 27 pCi
Real Life Examples
1 CXR = 0.02 mSv
Background radiation ~3 mSv / yr (150
CXR’s)
AXR 1.5 mSv (75 CXR’s)
Abdominal CT 6 – 8 mSv (300-400 CXR’s)
Background radiation in affected parts of
Belarus, Ukraine, & Russia 6 -11 mSv / yr
(300 – 550 CXR’s)
Firefighters in Chernobyl 0.7 – 13 Sv
(35,000 – 650,000 CXR’s)
Types of exposure
External radiation
E.g. X-rays
Only neutrons can produce radioactivity
I.e. a pt exposed to other radiation is NOT radioactive & poses no risk to others
External contamination
E.g. radioactive spill in lab
Incorporation & internal contamination
Ingestion, inhalation, open wounds
Radiation MOA
Direct effects
Ionization & damage of molecules (e.g. cross-linking of DNA)
100 mGy -- get ssDNA damage (reparable)
0.5 - 5 Gy -- dsDNA damage (irreparable)
Indirect effects
Ionization of H
2
O to H
2
O + radical decays to free radicals which react with & damage other molecules
Determinants of severity
Dose rate
How fast a given dose is delivered
Energy
Total dose
Total vs. partial exposure
Tissue(s) exposed (radiosensitivity)
Radiosensitivity
Three laws of radiosensitivity
Bergonie & Tribondeau, 1906
Varies directly w/ rate of cell proliferation
Varies directly w/ # of future divisions
Varies inversely w/ degree of morphologic & functional differentiation
Lymphocyte is the exception = most radiation-sensitive cell in body
Human Radiation Effects
Deterministic (nonstochastic)
Threshold dose
Effect is not seen if threshold dose is not exceeded
See dose-response curve
Effects manifest w/in mins – wks
E.g. ARS
Stochastic
No threshold dose
Controversial
Not all exposed individuals manifest the effect
No clear dose-response curve
Effect less pronounced at high exposures
E.g. = radiationinduced carcinogenesis
Radiation Injury Scenarios
Nuclear device detonation
Military use (e.g. Hiroshima, Nagasaki)
Terrorist use
“Dirty” bombs
RDD (radiation dispersal device)
Industrial accidents / spills
Chernobyl, Three mile island
Medical & Research
Radiation Tx, Radioisotope spills
Nuclear Detonation
Blast & thermal effects
Most significant injuries acutely therefore Tx conventional injuries first
Megaton yield weapons lethal radius from blast & thermal effect larger than that for radiation effect Radiation effects
Radiation effects
Intense neutron & gamma ray release
Fallout
Radioactive particulate matter (soil etc) following significant radiation release or nuclear explosion
Can poison food chain & render area uninhabitable for yrs
Can travel great distances (e.g. Chernobyl)
Acute Radiation Syndrome
Most common cause of death in 1 st 60d following external whole body irradiation
Divided into sequential subsyndromes:
Hematopoietic (1- 5 Gy)
Gastrointestinal (6-30 Gy)
CVS / CNS (>30 Gy)
4 separate stages
Prodromal, latent, manifest illness, recovery
Timing of stages & subsyndromes inversely related to dose received
LD
50 for radiation is estimated to be 4.1 Gy (95%CI
2.55 – 5.5)
ARS: Prodromal & Latent
Phase
Dose
(Gy)
0.5 – 2
2.1 – 3.5
3.6 – 5.5
> 5.6
Onset
(h)
≥ 6
2 – 6
1 – 2
Mins – 1
Duration
(h)
< 24
Latency
≥ 3 wks
12 – 24 2 – 3 wks
24 1 – 2.5 wks
48 2 – 4 days
ARS: Prodromal Phase
1 o Sx are N &V, diarrhea (occ bloody)
Anorexia, weakness, fatigability
Time of onset inversely related to dose
Duration & severity directly related to dose
Mild Sx occurring ≥ 2 hrs post-exposure
& lasting < 24 h usually imply dose < 2
Gy
ARS: Latent Phase
Duration inversely related to dose
Hrs - wks
May be asymptomatic w/ lower doses
More at risk for infection
Delayed wound healing
Critical to monitor closely
ARS: Illness Phase
Hematopoetic (1 – 5 Gy)
Delayed onset of pancytopenia due to stem cell irradiation
Death due to sepsis +/- hemorrhage
Takes mos – yrs to recover
Lymphocyte & platelet counts can be used to estimate exposure & guide mgmt
Lymphocyte count 24-48 h post-exposure
(x1000 / mm 3)
3.0
1.2 – 3.0
0.4 – 1.2
0.1 -0.4
< 0.1
Estimated Dose (Gy)
≤ 0.25
1 – 2
2 – 3.5
3.5 – 5.5
> 5.5
ARS: Illness Phase
Gastrointestinal (6 -30 Gy)
GI stem cell death breakdown of intestinal mucosa w/ hemorrhages, fluid
& electrolyte shifts, & bacterial translocation
Sepsis
Malnutrition
Paralytic ileus
Hypovolemia & electrolyte imbalances
ARS: Illness Phase
CVS / CNS (> 30 Gy)
Direct damage to CNS & CVS tissues
C/o burning pain of skin w/in mins
Pyrexia, ataxia, elevated ICP & coma, hypotension w/in mins - hrs
Other Radiation Injuries
Skin burns
Transient erythema w/in hrs
Secondary erythema w/in 5 – 21d
Timing inversely proportional to dose
Low doses progress to dry desquamation
High doses wet epidermitis & blisters
Tx same as thermal burns +/- steroid creams
Acute radiation pulmonitis
Severe dyspnea, “thundering” creps
High dose exposure – almost universally fatal
Psychological Impact
Chronic Health effects
Radiation Injuries:
Management
Triage
Radiation injury unlikely
Absence of prodromal N & V & D
Probable radiation injury (survivable)
Group most likely to benefit from intensive medical care
Severe radiation injury (usually fatal)
Analgesics, comfort measures
Radiation Injuries:
Management
External Decontamination
Should occur ASAP & prehospital if possible
Showering or washing w/ soap & water achieves
~95% decontamination
Debride & clean open wounds
Risk to medical personnel exposed to contaminated persons appears to be minimal
Monitor w/ whole body radiation counters,
Geiger counters, thyroid scanners & bioassay sampling
Radiation Injuries:
Management
Internal Decontamination
Knowledge of radioisotope important to guide management
Decrease absorption
Cathartics, SBL, charcoal, BAL for severe inhalation
Increase elimination
Chelation
Block uptake / incorporation
Antidotes E.g. potassium iodide (need to start w/in 12-
24h at latest)
Bioassay & Geiger counts on urine & feces to guide ongoing Tx
Chelators + Radioactive isotope (from D. Watt’s talk)
Prussian blue
Penicillamine
Chlorthalidone
Deimercaprol
Deferoxamine
Ca-EDTA
Zn-DTPA
Cesium
Cu, Co, Ag, Pb, Hg
Rubidium
Polonium
Iron
Cd, Cr, Pb, Zn
All the weird ones ±
American names
Radiation Injuries:
Management
Medical Tx
Largely supportive
Symptomatic Tx
Infection control
Serial CBC’s
Transfuse if plts < 20
CSF may be useful
Bone marrow transplant may be necessary
Any necessary surgery should occur either w/in
36 hrs; otherwise wait at least 3 mos
Fibroblasts & osteoblasts radiosensitive -- impaired wound healing
Radiation Injury: Chronic Risk
Stochastic effects
Highly controversial topic
While exposure to radiation appears to increase risk of CA, birth defects, and other health problems we still don’t know what a
“safe” dose is
Most people think risk of exposure is cumulative but even this is not clear-cut
One very large single dose likely more harmful than same dose over long time period
Mutation rate in crops of contaminated regions in Europe 6x higher than elsewhere
Increased incidence of thyroid CA
Increased incidence of various CA’s in atomic bomb survivors & aftermath of Chernobyl w/ exposures > 50 - 100 mSv
Studied hindered by methodological flaws -- difficult to determine precise risk for an individual exposed to increased radiation