Guest lecture - UEMS
advertisement

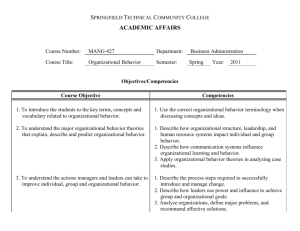
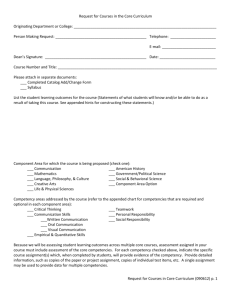
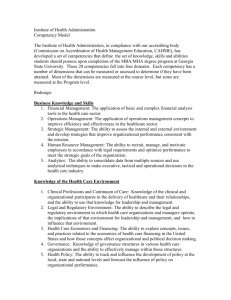
Medical specialty training in Croatia Nada Cikes, University of Zagreb School of Medicine National Authority for Specialty Training of Medical Doctors in Croatia UEMS ORL Section and Board, Dubrovnik, 4. October 2014. Medical education in Croatia • 4 medical schools • 2004 new harmonised core curriculum was introduced in all four schools • 2007 medical schools invited in specialty training programmes developments • 2007- 2011 new competency based specialty training programme was developed for all specialties • from 2011 implementation Introduction of new specialty programes • Need for competency and learning outcomes based programmes • Harmonisation with European documents: – European commission (EU Directive 2005/36 EC)* – UEMS (Charter on specialty training ..... Ch. 6) – Recommendation of intrnl. scientific societies • New specialties proposals: - new specialties - common trunks - reforms of old specialties • Proposal for a new Ordinance on specialty training of medical doctors in Croatia * qualification recognition: subject of negotiation with Croatia for EU accetion Development of specialist training programmes in Croatia • New competency based programmes for 46 specialties • Common trunk for internistic and surgical specialties • For all specialty programmes – duration – training plan – required level of competencies - generic - specific – list and number of procedures – logbook Croatian medical schools and other institutions in training programme development Agreement on collaboration in development of specialty education program between: • all four medical schools • Croatian Medical Association • Croatian Medical Chamber • Croatian Academy for Medical Sciences Development of programmes of specialists education in Croatia 46 task forces: • Programme of specialist education defining competences • Requirements for training institution • Requirements for mentor • Requirements for trainee and logbook Goals Objectives of training programme – generic competences - all physicians in training in all medical specialties – specific competences: knowledge, skills and attitudes – competence-based education, focused on learner performance - learning outcomes in reaching specific objectives of the curriculum Outcome of training programme – specialist able to practice in a professional, ethical and patient-focused way COMPETENCIES skills knowledge competencies professional behaviour Competencies in specialty training programmes • Characeristic for each specialty – common trunk – “main” program of the specialty • All educational units in the programme • Also the number of interventios • Evaluation of comparable competencies in groups of specialties (surgical, internistic) • Determine teaching methods • Determine assessment methods Important: generic competencies for all specialists DESCRIPTION OF THE LEVEL OF COMPETENCIES 1 2 3 Trainee is informed about thematic area on basic level, needs support and supervision in work and problem solving in the thematic area Trainee is partially competent, able to work and solve problems with support and partial supervision Trainee is fully competent, familiar with relevant literature, able to work and solve all problems in the thematic area Specific competencies – goals* • • • • • • Medical knowledge Patient care Practice based learning and improvement Systems based practice Professionalism Interpersonal and communication skills *ACGME Outcome Project 2006 Generic competencies in medicine • Tomorrow’s Doctor (GMC, UK) – generic and specific • The Scottish Doctor – generic and specific • Generic Curriculum for the Medical Specialties Federation of the Royal Colleges of Physicians • The Royal College of Physicians and Surgeons of Canada Physicians Competency Framework • European Board of Internal Medicine Core Competencies • Etc......... Generic competencies in specialty training The CanMEDS 2005 Framework: The Physician Roles • • • • • • • Medical Expert Role Communicator Role Collaborator Role Manager Role Health Advocate Role Scholar Role Professional Role Definitions of 7 roles of physicians • As Medical Experts, physicians integrate all of the CanMEDS Roles, applying medical knowledge, clinical skills, and professional attitudes in their provision of patient-centered care. Medical Expert is the central physician Role in the CanMEDS framework. • As Communicators, physicians effectively facilitate the doctorpatient relationship and the dynamic exchanges that occur before, during, and after the medical encounter. • As Collaborators, physicians effectively work within a healthcare team to achieve optimal patient care. • As Managers, physicians are integral participants in healthcare organizations, organizing sustainable practices, making decisions about allocating resources, and contributing to the effectiveness of the healthcare system. • As Health Advocates, physicians responsibly use their expertise and influence to advance the health and well-being of individual patients, communities, and populations. • As Scholars, physicians demonstrate a lifelong commitment to reflective learning, as well as the creation, dissemination, application and translation of medical knowledge. • As Professionals, physicians are committed to the health and wellbeing of individuals and society through ethical practice, professionled regulation, and high personal standards of behaviour. Implementation • The CanMEDS framework accepted, incorporated in the training programme: – as a teaching module obligatory for all specialties – parts of clinical teaching programmes – content in the logbook • Evaluation: – At the end of the module – Continuous evaluation by mentor – Multisource feedback - 360 degrees Introductory teaching module on generic competencies • Two weeks programme • Each competency: two half – days • Trainees participate with case studies from personal experience • Discussion between participants • Supporting documents and teaching materials (manual, e-learning...), additional reading Competency teaching in the module • Definition • Description • Elements (communicator: empathy, effective listening..... collaborator: respect for others in the team, constructive negotiations.....) • Key competencies • Specific training requirements Teachers in the generic module • 2 coordinators for each competency • Group of experienced and younger teacher in the group - clinicians ( family medicine, pediatrics, internal medicine, psychiatry...) - experts from public health • Workhops organised – for each competency - for the whole module Results of teachers’evaluation and general observation • Teachers’ positive attitude for generic skills increased • Educating students and understanding the teaching process motivated them to be good role models for students • Communication between teachers increased • Good relationship between students and young clinicians • Improvement of working environment in academic hospital was initiated • The generic skills in medical community are promoted Difficulties in teaching generic competences • Teaching environment in the training institution • Lack of understanding generic competencies • Need for education of mentors in teaching and evaluating generic competencies • Need for education of other physicians and other medical professionals in generic competencies Requirements • Training institution • Mentor • Trainee Requirements for training institution • Learning environment • General requirements • High level of educational and professional expertise, informatic technology, research • Requirements relevant for particular specialty fulfilling the conditions for study program (no. of relevant patients, procedures etc..) • Preparedness for regular visitation • Adaptation of Croatian regulations on health institutions! Mentor • Experienced specialist • Experienced teacher • Need to define time protected for teaching (hospital burden!) • Need to define relevant regulations • Number of trainees per mentor • Mentor’s education and evaluation • Important: employment policy (medical school and university hospital Trainee • General requirements • Logbook for particular specialty • Trainee follow up through training – progression of competence • Definition of evaluation methods • Requirements for final examinations • Special attention: trainees doctoral students Dual role of trainee: student and health care provider • • • • • Work in health care is part of education Patient care is the integral part of learning Every contact with patient is educational experience Supervision is integral part of learning experience Responsibility of all – trainee’s progress: education, competency, responsibility, patient safety.... • Goal of the advencement of specialty training process: enhancement of patient care Follow up of trainee progress THEME LEVEL OF PROGRESS 1 GENERIC/ SPECIFIC COMPETENCIES 2 Date and signature MENTOR 3 Date and signature Follow up of interventions Part of the training programme Name of the intervention Number of inte rve ntio ns Level of progress 2 MENTOR 3 Date and signature Date and signatue National authority responsible for specialty training • • • • • • • definition of national standards supervision of training programmes developments of assessment methods accreditations for institutions quality assurance institution visitation planing strategy Task force for evaluation and methods of assessment • Assessment is part of the educational programme • Base: UEMS Policy Statement on Assessment during Postgraduate Medical Training (2006): – – – – Selfevaluation (trainee) Continuous follow up (mentor) Test 360˚ Final exam – written and practical • UEMS CESMA: – European exam Evaluation of mentor Evaluation of training institution Training programmes were presented: • Association of Medical Schools in Europe 2009. • International Association for Medical Education (AMEE) – 2010 Glasgow – 2014 Milano • Policy dialogues, Investing in Europe’s health workforce of tomorrow: scope for innovation and collaboration . Follow up to the Green Paper on Europe’s health workforce, Leuven, Belgium, 2010 • Education for Physicians: A Comparison of Slovenia, Croatia and Italy, Brioni, 14 May 2011 • Various meetings and congresses in Croatia Zagreb Declaration, 2009 The Role of the Medical School in Postgraduate Education Conclusion Largest project in medical education in Croatia (600 MD specialists involved in programme development) Involvement and responsibility of – – – – – – – – Medical schools Health institutions Mentors Trainees Professional societies (Croatian Medical Association) Croatian Medical Chamber Other organisations Ministry of Health Teaching generic competencies Fundamentals of Medical Skills - longitudinal course • two parallel tracks: Clinical practical skills and Communication skills • emphasis on teaching communication skills, gradually developing medical students' competence from basic to specific communication associated with clinical courses in higher grades of medical study • expected: greater effectiveness of a longitudinal, integrated communication approach in teaching medical students compared with concentrated courses Study year Teaching content in longitudinal course in communication skills 1st Basic communication skills. Communication with colleagues, teachers, administrators and other members of the school and hospital staff 2nd Medical interview 3rd Informed consent. Written communication in medicine. Working in team 4th Giving information and counselling. Communication in clinical setting. Communication with severely ill patients. Breaking bad news. Palliative medicine. Aggressive patient 5th Communication with children. Breaking bad news to children. Communication with parents and family members. Pregnancy and childbirth. Elderly patients. Psychiatric patient 6th Communication in family and community. Communication as a part of professionalism. Communication with other professions. Communication with media. Workshops for teachers education • Role-playing • Simulated patient • Analysing specific videotapes of: – Real patient cases in health care – Pateint cases scenarios filmed by students of University of Zagreb Drama Academy • Observation and constructive feedback discussions with peers and facilitator • Organisation and training for OSCE OSCE After 15 weeks of traning: • Standardised patients in simple clinical situations • Opening and closing the interview • Some stations: combined practical skills with communicational task Reasons why clinicians can be good teachers in communication • Good understanding of communication theories • Positive attitude towards communication based on personal clinical experience • Understanding of patients’ centeredness in communication process • Additional impact: teachers became highly competent in communication with patients, colleagues and others • Influence on communication climate in health care environment • Students appreciate colleagues being their teacher in communication Generic competencies in internship • Internship is organised in rotations • Competencies included in the programme: – communication skills – team work – professionalism • Elements of each competencies defined • Tasks recorded during whole programme Conclusion • Continuous enhancement of generic competences through the graduate and postgraduate education is essential for professional development • Continuous reinforcement and longitudinal development of skills is critical for their retention and expansion • Teaching generic skills on all levels of medical education exerts influence on development of professionalism in hospital environment • Influence on health care