postgraduate medical training in the UK
advertisement

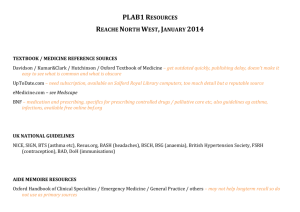
postgraduate medical training in the UK 2011/2012 Lydie Fialová University of Edinburgh medical training • medical school - 5 years (29 med schools) intercalated BSc, MSc - 1 year • foundation training - 2 years - UKFPO full GMC registration after FY1 • GP and specialty training - Royal Colleges • • general practice - 3 years specialty training - 4-7 years institutions involved • General Medical Council • Royal Colleges • NHS Deaneries • Universities (Academic Medicine) • http://www.mmc.nhs.uk/colleges__dean eries/deaneries.aspx points of entry • FY1 (FTAS) • FY2 (GMC registration) • ST/GP entry (CCFT – 3 years) • core training - subspecialty training • run-through training programs • CCT (certificate of completion of training) entry - consultants FY1 entry • • • • • http://www.foundationprogramme.nhs.uk national centralized recruitment process application - October (FTAS) eligibility - August (UKFPO eligibility office) provisional GMC registration http://www.gmcuk.org/doctors/registration_applications/s15a_ p1.asp allocation to FT • • • allocation to foundation schools based on ranking of the application list of foundation schools http://www.foundationprogramme.nhs.uk/page s/medical-students/deaneries-foundationschools provisional GMC registration http://www.gmcuk.org/doctors/registration_applications/s15a_ p1.asp FT application • educational performance measure (EPM) • • • • Medical school performance, providing a decile score - 34 – 43 points Additional degrees (Bachelors, Masters and Doctorates) – maximum of 5 points Publications, presentations and prizes – maximum of 2 points situational judgment tests (SJT) situational judgment tests Situational Judgement Tests are a test of aptitude and are designed to assess the professional attributes expected of a Foundation doctor. There are two question formats: 1. Rank five possible responses in the most appropriate order 2. Select the three most appropriate responses for the situation example 1 You are looking after Mr Kucera who has previously been treated for prostate carcinoma. Preliminary investigations are strongly suggestive of a recurrence. As you finish taking blood from a neighbouring patient, Mr Kucera leans across and says “tell me honestly, is my cancer back?” A Explain to Mr Kucera that it is likely that his cancer has come back B Reassure Mr Kucera that he will be fine C Explain to Mr Kucera that you do not have all the test results, but you will speak to him as soon as you do D Inform Mr Kucera that you will chase up the results of his tests and ask one of your senior colleagues to discuss them with him E Invite Mr Kucera to join you and a senior nurse in a quiet room, get a colleague to hold your ‘bleep’ then explore his fears answer: DCEAB It is not a FY1’s responsibility to break bad news to a patient and the full results are not available yet. It would be most appropriate for a senior colleague to speak to Mr Kucera with regards his diagnosis. Informing Mr Kucera that you will speak to him as soon as you get the test results back would still be appropriate as you are giving him some information, although this may not necessarily mean that you would be providing him with the diagnosis. It may be appropriate to discuss Mr Kucera’s fears with him, but by doing this you may not be attending to other ill patients and are asking a colleague to take on your responsibility by holding your bleep. It may also become a difficult conversation when you do not have full details of the results. It would not necessarily be appropriate to tell Mr Kucera that his cancer is back as this has not been confirmed, however it would be inappropriate to provide false hope to a patient when preliminary investigations are strongly suggestive of a recurrence. example 2 You review a patient on the surgical ward who has had an appendectomy done earlier on the day. You write a prescription for strong painkillers. The staff nurse challenges your decision and refuses to give the medication to the patient. • • • • • • • • A Instruct the nurse to give the medication to the patient B Discuss with the nurse why she disagrees with the prescription C Ask a senior colleague for advice D Complete a clinical incident form E Cancel the prescription on the nurse’s advice F Arrange to speak to the nurse later to discuss your working relationship G Write in the medical notes that the nurse has declined to give the medication H Review the case again answer: BCH Ensuring patient safety is key to this scenario. It is important to discuss the nurse’s decision with her as there may be something that you have missed when first reviewing the patient. Therefore it would also be important to review the patient again. Also relating to this is the importance of respecting the views of colleagues and maintaining working relationships, even if there is disagreement. As there has been a disagreement regarding patient care, it is important to seek advice from a senior colleague. professional attributes • • • • • • • • • Patient Focus Commitment to professionalism Coping with pressure Effective communication Problem solving and decision-making Organisation and planning Working effectively as part of a team Self-awareness and insight Learning and Professional Development FT resources • http://www.foundationprogramme.nhs.u k/pages/home • academic programmes http://www.foundationprogramme.nhs.u k/pages/academic-programmes • selection for FT http://www.isfp.org.uk/ GMC resources • Trainee Doctor http://www.gmcuk.org/Trainee_Doctor.pdf_39274940.pdf • Good Medical Practice (2006) http://www.gmcuk.org/guidance/good_medical_practice.a sp • GMC interactive cases http://www.gmcuk.org/guidance/case_studies.asp FY 2 entry • must hold GMC full registration and licence • • • • http://www.gmcuk.org/doctors/registration_applications/s3_p1. asp stand-alone FY2 jobs - rare and competitive ‘locum appointment’ jobs - LAT (training) or LAS (service); portfolio advertised through http://www.jobs.nhs.uk; http://www.jobs.scot.nhs.uk and other national websites specialty training • run-through specialties - ST • GP, paediatrics, OG, opthalmology, microbiology, pathology, public health... • core training and specialties - CT + ST • acute care, surgical specialties, medical specialties, psychiatry • Royal Colleges and GMC ST/CCT entry • GMC registration • Royal Colleges - individual specialties • certificate of eligibility for ST/GP registration - http://www.gmcuk.org/doctors/registration_applications/ certification_college_contacts.asp • ST application - November ST selection • application - person specification • interview / situational judgment • portfolios and certificates • appraisals and recommendation letters • certificate confirming eligibility for specialty registration • academic medicine specialty training • England http://www.mmc.nhs.uk/ • Wales http://specialty.walesdeanery.org/ • Scotland http://www.scotmt.scot.nhs.uk/ • Northern Ireland http://www.nimdta.gov.uk/ • http://www.gprecruitment.org.uk/ STx entry • fixed term specialty training appointments • FTSTA and locums advertised through • http://www.jobs.nhs.uk • http://www.jobs.scot.nhs.uk • http://careers.bmj.com/careers/hosp ital-medical-healthcare-doctorsjobs.html GMC registration • provisional/full registration and license to practice • specialist registration • GP registration GMC registration • documents • ID documents • medical training • certificate of good standing • fee • identity check - London GMC registration info • http://www.gmcuk.org/doctors/medical_register.asp • http://www.gmcuk.org/doctors/applications.asp • http://www.gmcuk.org/doctors/registration_applications/ s3_p1.asp key links • http://www.gmc-uk.org/ • http://www.medicalcareers.nhs.uk/ • http://aomrc.org.uk/ • http://careers.bmj.com • http://www.jobs.ac.uk/