Parkinsons (Unfolding Case Study) from QSEN in PPTX
advertisement

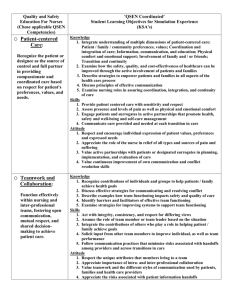
Unfolding Case Study: Applying the QSEN Competencies to the care of Patients with Parkinson’s Disease Gerry Altmiller, EdD, APRN, ACNS-BC From QSEN • Unfolding Case Study (from QSEN): Applying the QSEN Competencies to the Care of Patients with Parkinson’s Disease • Students will be instructed to review information on Parkinson’s Disease prior to class by visiting the National Parkinson’s Disease website http://www.parkinson.org/parkinson-s-disease.aspx. • This unfolding case study powerpoint presentation will be provided in class. • Students will be encouraged to brainstorm to answer the questions as the case study unfolds. • Theory bursts are woven throughout the case study. The presentation includes links to Lee Siverman’s Voice Training (LSVT), which is a proven program to help patients with Parkinson’s Disease speak loudly and walk with a more stable gait. • Following the class session, the case study will be posted for the class to retrieve so that theory content is available to them. You are assigned to care for Mr. Conley, age 70, who was admitted to your unit post-operative yesterday for excision of a strangulated inguinal hernia. His VS are stable, IVF infusing D5.45 NS at 100ml/hr, bowel sounds have returned, and his surgical site is clean, dry, and intact. He is ordered percocet for pain PO PRN and and is currently pain free. He is beginning a clear liquid diet this am. His past medical history includes mild hypertension, benign prostatic hypertrophy, degenerative joint disease, and Parkinson’s Disease. QSEN Competency: Teamwork and Collaboration Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care. During team huddle with the surgeon and medical resident, you report concerns from the AM assessment which include that Mr. Conley’s speech is slurred, soft, and slow and his face is expressionless with some drooling. He has a noticeable tremor of the right hand. His appearance is thin and frail. Theory Burst • Parkinson’s Disease is a chronic, progressive, neurodegenerative disorder characterized by: – Tremor at rest • Pill-rolling, tremor resembles rotary motion; often first sign • Handwriting begins large and trails off – Slowness in initiation of movement (bradykinesia) • arm swing with walking, swallowing saliva, blinking, blank facial expression, stooped posture – Increased muscle tone (rigidity) • Cog-wheel rigidity; jerking quality to purposeful movements • Generalized slowness-loss of dopamine, a neurotransmitter in brain needed to initiate movement • More common in men • Affects 160 per/100,000; Diagnosis increases with age • No specific test; diagnosis based on H & P and positive response to antiparkinson’s medications QSEN Competency: Teamwork and Collaboration Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care. The team determines the plan of care for the day is: Resume PO medications Sinemet 25mg/100mg CR PO three times daily Hytrin 2 mg PO at bedtime Celebrex 100mg PO twice daily Lexapro 10 mg PO daily OOB x 3 Ambulate as tolerated Progress diet as tolerated; assess swallowing function Consult Physical Therapy and Speech Therapy QSEN Competency: Safety Minimize risk of harm to patients and providers through both system effectiveness and individual performance. What immediate safety priorities for the day do you identify and why? • Aspiration risk – Known Parkinson’s Disease– Slurred speech, drooling- control of muscles – Post anesthesia • Falls risk – Known Parkinson’s Disease – – – – • postural instability • Sticky feet-inability to initiate movement Post-operative/post-anesthesia/bed rest IV infusing Frail appearance Medication risks? • Medication Reconciliation Needed QSEN Competency: Safety Minimize risk of harm to patients and providers through both system effectiveness and individual performance. How will you address the safety concerns? To Reduce Risk of Aspiration • • • • • Assess gag reflex OOB to chair for meals Full Fowler’s position when possible Speech/swallowing consult Administer medications on time to improve muscle control To Reduce Risk of Falls • • • • • • • Out of bed with assistance Make position changes slowly Use of walker to increase stability Call bell within reach Use of soled shoes Ask for Physical Therapy consult Administer medications on time to improve muscle control QSEN Competency: Evidence-based Practice Integrate the best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care. Theory Burst • Staff education regarding Parkinson’s Disease medication therapy – Aimed at correcting imbalance of neurotransmitters in brain-dopamine – Must be on time due to end of dose wear-off • When medications work, the patient is “on” and able to initiate movements; Once levels drop, patient experiences “off” time and unable to initiate movements – Medications can cause dyskinesia • Uncontrolled movements of face, eyelids, mouth, tongue, arms, hands, legs, squirming movements Medication Reconciliation What concerns do you have regarding Mr. Conley’s medications? Any interactions? Why these medications for this patient? Interactions/Cautions • Hytrin and Sinemet both cause orthostatic hypotension • Celebrex (NSAID) may decrease effectiveness of hytrin Rationales for use in Mr. Conley • Lexapro-many Parkinson’s Disease patients experience depression • Hytrin-control HTN and decreases symptoms of BPH • Celebrex- Decrease inflammation and pain of degenerative joint disease • Sinemet-Control of Parkinson’s Disease symptoms Theory Burst Medication aimed at Parkinson’s Disease symptom relief: • Sinemet: levodopa with carbidopa crosses the blood-brain barrier & converts to dopamine. Carbidopa inhibits an enzyme that would breakdown the levodopa • MAO-B Inhibitors: (Eldepryl, Azilect) inhibit the breakdown of dopamine • COMT inhibitors: slow the breakdown of levodopa, thus prolonging its action • Amantadine: promotes effects of dopamine ©Altmiller Mrs. Conley arrives to assist with Mr. Conley’s hygiene needs. While speaking with you, she states “He hasn’t gotten his pills yet and he didn’t get them yesterday! I am so upset! When he doesn’t get his pills, this is what happens. He didn’t look like this at home.” How should you respond to Mrs. Conley? What actions can you take as his nurse? QSEN Competency: Patient Centered Care Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient preferences, values, and needs. • Acknowledge concerns • Identify current plan of care for the day – Ask Mr. & Mrs. Conley to contribute to plan and goal development • Ascertain positive gag reflex • Notify pharmacy that Sinemet dose is high priority QSEN Competency: Teamwork and Collaboration Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decisionmaking to achieve quality patient care. Mr. Conley’s Sinemet CR (sustained release) arrives on the unit. What important nursing considerations are associated with this medication administration? QSEN Competency: Safety Minimize risk of harm to patients and providers through both system effectiveness and individual performance. • Sustained release meds cannot be crushed or chewed. • Observe for therapeutic effect – dose adjustments are based on patient tolerance. • Observe for “on-off” phenomenon- – Unpredictable loss of drug effectiveness which lasts 1 min-1 hour, followed by equally abrupt return of function; may occur with end of dose wear-off. • Observe for dyskinesia – Facial grimacing, tongue protrusion, bobbing of head, jerky movements of the arms, legs, torso, extra squirming movements. • Make position changes slowly – can cause postural hypotension. QSEN Competency: Teamwork and Collaboration Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decisionmaking to achieve quality patient care. The speech therapist arrives and evaluates Mr. Conley with you. She determines that Mr. Conley’s swallowing allows for safe feeding. As she asks him questions, he is slow to answer and Mrs. Conley frequently answers questions for him. What interventions can you suggest to help improve Mr. Conley’s communication? To Improve Communication with Parkinson’s Disease Patients • Be patient-give the patient time to answer even though speech is slow. • Do not finish sentences for the patient. • Assist family to understand need to allow patient to speak for him/herself. • Intentional effort to be loud – Being loud has trickle down effect; requires patient to open mouth more and articulate more – http://lsvtglobal.com/loud-certification Click and scroll down to view Featured Video QSEN Competency: Teamwork and Collaboration Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care. The physical therapist arrives to evaluate Mr. Conley with you. It is determined that he can transfer from the bed to the chair with assistance and he should begin chair exercises. Mrs. Conley questions why he has to do this. What would be the best explanation to provide Mrs. Conley? QSEN Competency: Evidence-based Practice Integrate the best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care. Theory Burst Exercise slows progression of the disease (It is neuroprotective) • • • • May need brace to raise front of foot Isotonic exercises build strength Provide pictures of exercises to include at home Gait training is essential-take big steps – LSVT Big Training http://lsvtglobal.com/news/video Scroll down to Pre & Post Treatment Example Video and click A regular house diet is delivered for Mr. Conley for lunch. Mr. Conley attempts to eat with assistance from his wife but complains that it is too much work and he is not hungry. QSEN Competency: Informatics Use information and technology to communicate, manage knowledge, mitigate error, and support decision making. You document the poor intake for lunch in the electronic health record and decide to search for diet information regarding Parkinson’s Disease patients. What dietary accommodations would be most appropriate for Mr. Conley? QSEN Competency: Evidence-based Practice Integrate the best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care. • Redistributive Diet the negative impact protein has on levodopa precurser of dopamine – Protein impairs levadopa absorption – More protein at the end of day when patient is going to bed; less protein in the day to enhance daytime motor performance • High Fiber (to prevent constipation) • Concerns with caffeine – Can aggravate symptoms but may help with apathy/drowsiness • Small bites; food that is easy to chew • Adequate hydration (to prevent constipation and orthostatic hypotension) • Allow food from home to improve appetite ©Altmiller After a few days, Mr. Conley is ready for discharge to home. What important teaching should be included in his discharge instructions? Parkinson’s Disease homecare • Post-operative care regarding surgical incision site • Arrangement of post-discharge office visit • Promote exercise as neuroprotective; refer to http://lsvtglobal.com • Encourage loud speaking and big movements • Promote independence • Chairs with arms, raise back legs if needed to assist rising • Evaluate side effects of meds – Dyskinesia-squirming movements, protrusion of tongue – “on-off” effect QSEN Competency: Quality Improvement Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems. After caring for Mr. Conley, what improvements can you suggest for the care of hospitalized Parkinson’s Disease patients? QSEN Competency: Quality Improvement Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems. Take new information to the Falls Prevention Committee to include that Parkinson’s Disease medications must be given on time to prevent “off” times as a falls prevention measure. Suggest identifying information on chart to ensure hand-off includes falls and aspiration risk for Parkinson’s Disease patients. Provide staff education on Parkinson’s Disease; as population ages, there is increasing prevalence. The QSEN Competencies 1. QSEN Competency: Patient Centered Care Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient preferences, values, and needs. 2. QSEN Competency: Teamwork and Collaboration Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care. 3. QSEN Competency: Evidence-based Practice Integrate the best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care. 4. QSEN Competency: Quality Improvement Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems. 5. QSEN Competency: Safety Minimize risk of harm to patients and providers through both system effectiveness and individual performance. 6. QSEN Competency: Informatics Use information and technology to communicate, manage knowledge, mitigate error, and support decision making.