Historical and current practice with regards
advertisement
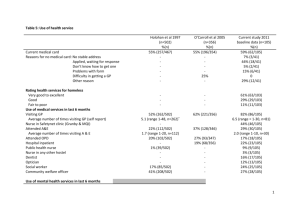
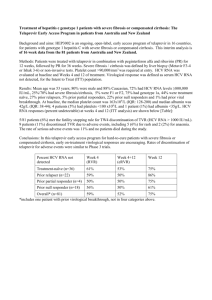
Historical and current practice with regards alcohol misuse and dependence, Opiate Replacement Therapy and hepatitis C Dr Iain Smith, Consultant Addiction Psychiatrist, NHS Greater Glasgow & Clyde Addiction Services And Committee Member, SHAAP The Kershaw Unit The Most Drunken Nation on Earth? MAJOR BURDEN OF DISEASE IN DEVELOPED COUNTRIES-RISK FACTORS AND DISEASES (source:The World Health report,2002) SCOTLAND’S OUT OF STEP Liver Cirrhosis Death Rates 1950 - 2006 Alcohol related deaths in the UK, by local area, 1998-2004 Source: Office for National Statistics • 15 of the 20 UK areas with the highest male death rates are in Scotland • Dundee ranks 5th highest in the UK for men • For women, the alcohol related death rate in Dundee ranks 2nd highest in the UK WHO GLOBAL ALCOHOL STRATEGY 2010 ACTIONS IN SCOTLAND Public Education to mobilise support for effective policies Consistent messages from health , police and welfare organisations Early Identification and brief advice National programme established in 2009 Effective specialist treatment Additional investment and national guidance Community action with media advocacy Drink driving action Range of local “Focus on Alcohol” projects Effective licensing of alcohol sales Public health principle in Licensing. Preventing overprovision. Regulation of marketing Ban on multi-buy discounts and regulation of shop displays Price controls (cheapest alcohol) Minimum unit price law passed. Legal challenge from industry. At ECJ Server training and monitoring Now compulsory. Consistent enforcement. Limit reduced to 50mg Dec 2014 How Do Things Look in 2015? Jan 06 Lancet paper Jun 06 SHAAP set up. May 07 Scottish Parliament elections Sep 07 SHAAP MUP Rpt Apr 2009 ABI Programme Sept 2009 Licensing Act. (Server training, Test purchasing,) April 2011. Waiting Times target Oct 2011 Multibuy ban, Happy hour ban, Challenge 25, May 2012 MUP Bill Passed. Source: ISD Scotland SMR 99 MESAS Report2014. Quantifying the Fraction of Cirrhosis Attributable to Alcohol Among Chronic Hepatitis C Virus Patients: Implications for Treatment Cost-Effectiveness Hamish A. Innes,1,2 Sharon J. Hutchinson,1,2 Stephen Barclay,3 Elaine Cadzow,3,4,5 John F. Dillon,6 Andrew Fraser,7 David J. Goldberg,2 Peter R. Mills,4 Scott A. McDonald,1,2 Judith Morris,5 Adrian Stanley,3 and Peter Hayes8; on behalf of the Hepatitis C Clinical Database Monitoring Committee Innes et al-Conclusions • A substantial proportion of patients with chronic HCV develop liver cirrhosis as a consequence of heavy alcohol use. • This has not been adequately acknowledged by cost utility analyses (CUAs). As such, estimates of cost-effectiveness may be exaggerated. • Thus, thesedata are important to guide forthcoming CUAs in terms of taking better account of the factorsleading to cirrhosis among patients with chronic HCV. (HEPATOLOGY 2013;57:451-46 NHS GGC-OST Services Some Challenges • Key data on HCV epidemiology, care and disease burden among PWID in Europe are sparse but suggest many undiagnosed infections and poor treatment uptake. Stronger efforts are needed to improve data availability to guide an increase in HCV treatment among PWID.(Weissing et al.2014) • There is a high prevalence of alcohol use, abuse, and dependence in methadone maintenance treatment (MMT) programs. The Good Habits A) Screen-Ask the questions as part of the initial assessment B) Intervene-Prevent or manage withdrawal C) Advise-Tailored brief interventions have an effect. D)Refer On-Particularly in those with dependency or recurring harmful use Treatment-1 TREATMENT-2 • Assistance for withdrawal-home detox. ; daypatient detox.; inpatient detox: benzodiazepines and vitamin replacement • Psychological therapies based on motivational and cognitive models have definite success-individual and group • Treatment goal varies with misuse and dependence and associated comorbidity : controlled drinking vs. abstinence; opportunistic brief intervention • Non –statutory agencies e.g. Alcoholics anonymous • Pharmacotherapy- disulfiram , acamprosate, naltrexone • Treatment of physical and psychiatric comorbidity Potential Interactions Among Medications Used to Treat Chronic Hepatitis and Behavioral Health Conditions • Prescription Medication Indication Potential Interaction With Hepatitis Medications Buprenorphine Opioid dependence The use of boceprevir could result in an increase or decrease in buprenorphine levels. However, the combination of buprenorphine and boceprevir has not been studied. Clinical monitoring for dose adjustment is recommended. • Clozapine Schizophrenia; psychosis Clozapine might cause marrow disorders, neuroleptic malignant syndrome, and increased seizure risk. When taken with interferon, the risks of these might increase. • Disulfiram Alcohol use disorders peripheral neuropathy. Disulfiram might cause or worsen hepatitis. When taken with interferon alpha 2a, there is increased risk of • Escitalopram recommended. The use of telaprevir can result in decreased escitalopram concentration. Clinical monitoring for dose adjustment is • Methadone Opioid dependence The use of telaprevir is associated with decreased methadone concentration. Clinical monitoring for dose adjustment is recommended.The use of boceprevir could result in an increase or decrease in methadone levels. However, the combination of methadone and boceprevir has not been studied. Clinical monitoring for dose adjustment is recommended. • Naltrexone • Trazodone Depression The use of telaprevir or boceprevir can result in an increase in trazodone concentration, which might lead to adverse events (e.g., nausea, dizziness). The combination of telaprevir or boceprevir and trazodone should be used with caution and a lower dose of trazodone should be considered. . • Depression Opioid and alcohol use disorders When taken with interferon alpha 2a, naltrexone might exacerbate liver damage. Zolpidem Insomnia The use of telaprevir can result in decreased zolpidem concentration. Clinical monitoring and dose adjustment of zolpidem is recommended to achieve the desired response. CONCLUSIONS • Challenges ahead in better integrating services for alcohol,drugs,mental health and hepatitis C • One stop shop model seems best where this can be achieved with some allowance for severity of problem and intensity of treatment required.