Schizophrenia

SCHIZOPHRENIA and Other Psychotic Disorders
Kurt Vonnegut
The Eden Express (1995)
Vonnegut
Most diseases can be separated from one’s self and seen as foreign intruding entities. Schizophrenia is very poorly behaved in this respect. Colds, ulcers, flu, and cancer are things we get.
Schizophrenic is something we are. It affects the thing we most identify with – as making us what we are.
Vonnegut continues…
If these weren’t problems enough, schiz comes on slow and comes on fast, stays a minutes or days or years, can be heaven one moment, hell the next, enhances abilities and destroys them, back, and forth several times a day and always weaving itself inextricably into what we call ourselves. It can transform only a small corner of our lives or turn the whole show upside down, always giving few if any clues as to when it came or when it left or what was us and what was schiz.
Schizophrenia is one of the most severe mental disorders
It presents a wide range of disruptive symptoms and leads to a significant loss in ability to function independently
Its prognosis is generally poor and its course tends toward progressively more disabled functioning over time.
Schizophrenia has been observed for more than 3000 years.
Emil Kraepelin (1850-1926)
First identified the symptoms of schizophrenia
Named this cluster of symptoms “Dementia
Praecox” in his 1883 text.
Paul Eugene Bleuler (1857-1939)
Bleuler renamed “Dementia Praecox” as
“Schizophrenia.”
Bleuler, a Swiss psychiatrist, considered Schizophrenia to be a “fundamental disturbance” that split psychic functions and, in extreme cases, led to disorganization of the personality.
He defined Schizophrenia as an inability to maintain goal-directed behavior and integrated thinking.
Demographics for Schizophrenia
Schizophrenia is a relatively rare disorder: 0.2% to
1.0% of world population
However, persons with schizophrenia occupy over 30% of the total number of beds in psychiatric hospitals.
It was thought that the percentage of people worldwide who have schizophrenia is consistent across different cultures, but recent statistics have questioned that belief.
The most common age is between 15 and 35 years old
More Demographics
Generally psychotic symptoms begin after a gradual deterioration of social functioning and personal hygiene, and the development of flat or inappropriate affect.
Persons with slower onset tend to have a more negative prognosis than those in which schizophrenic symptoms develop rapidly.
Gender Issues
Schizophrenia occurs more often in males than females.
Age of onset is often later for women
Men are hospitalized more often than women and show a more deteriorating course
Women are more likely to be married and have children than males with schizophrenia
Women tend to have a higher social and sexual functioning before diagnosis.
Familial Pattern
Some evidence is available that suggests a hereditary predisposition to schizophrenia:
European family studies indicate a lifetime risk of about 6% in the parents of schizophrenic clients; 10% in their brothers and sisters, and 13% in their children, as compared with 1% in the general population.
If one identical twin has schizophrenia, then there is a
50-60% probability that both are.
Risk Factors
There’s a high incidence of social phobia, obsessivecompulsive disorder, and panic attack in persons who later develop schizophrenia
Approximately 45% of those who have schizophrenia also abuse substances
Have a high rate of chronic illnesses in almost every system in the body (partly because of insufficient treatment).
Risk Factors (con’t.)
Approximately 20% of persons with schizophrenia attempt suicide
Approximately 10% complete the act
The suicide rate of the general population is .05%
Attempts generally occur just as symptoms begin to clear, not during psychotic periods
There is no evidence, however, that people with schizophrenia present any significant risk to others.
Persons with schizophrenia tend to commit fewer crimes than general population, although they are more frequently victims of crime.
Essential Features of Schizophrenia
(See p. 312)
A mixture of characteristic signs and symptoms
(both positive and negative) that have been present for a significant portion of time during a 1-month period (or for a shorter time if successfully treated), with some signs of the disorder persisting for at least 6 months. (Criteria A and C)
These sign and symptoms are associated with marked social or occupations dysfunction (Criterion
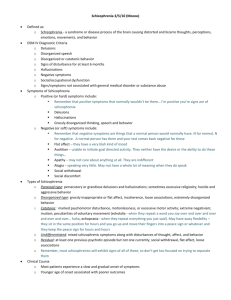
Schizophrenia
Client must be ill for at least 6 months, with at least two of five symptom types:
Delusions
Hallucinations
Disorganized Behavior
Disorganized Speech
Negative Symptoms
Symptoms of Schizophrenia
Delusions
A false belief that cannot be explained by the individual’s culture or education.
The individual cannot be persuaded that the belief is incorrect, despite evidence to the contrary or weight of opinion
Types of delusions: grandeur, guilt, ill health, jealousy, passivity, persecution, poverty, reference, and thought control.
Symptoms (continued)
Hallucinations
A false sensory perception that occurs in the absence of a related sensory stimulus.
Hallucinations are nearly always abnormal
They can affect any of the fix sense, but auditory and visual are most common
Symptoms (continued)
Auditory Hallucinations
The voices will often comment on behavior and, at times, give commands.
The command hallucinations may tell the individual to harm him/herself or others
Therefore, it’s important during examination to ask the client about the content of the auditory hallucinations, as well as any intent to act on them
Hallucinations (continued)
Visual Hallucinations often indicate a substanceinduced psychotic disorder or a psychotic disorder due to a general medical condition (GMC)
Olfactory, tactile, and visual hallucinations are extremely rare, and they generally co-occur with auditory hallucinations.
Hallucinations must occur when the person is fully conscious
Symptoms (continued)
Disorganized Speech
Also called loose association – mental associations are governed not by logic but by rhymes, puns, and other rules not apparent to the observer, or by no clear rules at all
Psychologically disorganized speech must be so badly impaired that it materially interferes with communication.
Symptoms (continued)
Disorganized Behavior
Physical actions that do not appear to be goal-directed (e.g., taking off one’s clothes in public, repeatedly making the sign of the cross, assuming and maintaining postures) may indicate psychosis.
Symptoms (continued)
Negative Symptoms
These symptoms are called “negative” because they give the impression that something has been taken away from the individual, not added, as in the case with hallucinations and delusions.
Negative symptoms reduce the apparent textural richness of an individual’s personality
Symptoms (continued)
Negative Symptoms - lack or are the absence of something, such as:
Inexpressive faces, blank looks, unresponsiveness (flat or blunted affect)
Loss of will, spontaneity, and initiative to do things
(avolition)
Seeming lack of interest in the world and other people, social withdrawal (asociality)
Apparent inability to show or feel pleasure (anhedonia)
Loss of adaptive personal and social skills
Symptoms (continued)
Negative Symptoms
Attention impairment
Markedly reduced amount or fluency of speech, poverty of speech (i.e., speech conveys little information) (alogia),
Increased speech latency (abnormal period of time to respond to another person’s comment)
Negative motor symptoms; e.g., maintaining bizarre postures, passively allowing one’s body to be manipulated by others, catatonic stupor (no response or interaction with external environment)
Definition of Five Types of Schizophrenia
#1 Paranoid Type
These clients have persecutory delusions and auditory hallucinations, but no negative symptoms, disorganized speech, or catatonic behavior.
Paranoid Type (continued)
Often appear the most normal
Better able to take care own day-to-day needs
Relatively late age of onset (average age of 35 years)
Delusions are typically persecutory or grandiose, or both & organized around a coherent theme.
Hallucinations are also related to the delusional theme.
However, the delusion or auditory hallucinations for this diagnosis are not required to have paranoid content.
#2 Disorganized Type
In this subtype, negative symptoms and disorganized speech and behavior are more prominent than delusions and hallucinations
People with this type are frequently the most obviously psychotic of all
They often deteriorate rapidly, talk gibberish, and neglect hygiene and appearance.
#3 Catatonic Type
The cardinal symptoms are excessively retarded or excited activity and bizarre behavior.
May have many of the basic symptoms of
Schizophrenia, but their abnormal physical movements set them apart.
Motor activity may be speeded up
However, behavior is more typically slow or retarded, sometimes to the point of stupor.
#4 Undifferentiated Type
These clients will have some or all of the five basic types of psychotic symptoms.
None of these symptoms dominates the clinical picture.
If the person does not have the paranoid, disorganized, or catatonic type, but still has schizophrenic symptoms, then s/he probably has the
Undifferentiated Type.
#5 Residual Type
This type might be diagnosed in a person whose diagnosis of Schizophrenia is already established, and
Who has either been treated or improved spontaneously - to the point of no longer having enough symptoms for a diagnosis of active
Schizophrenia
After an acute psychosis has markedly improved, these clients usually still seem somewhat unusual, odd, or peculiar.
Classification of Longitudinal Course
Definitions:
Episode. A period of prominent psychotic symptoms
Interepisode. A period between episodes
Continuous. Prominent psychotic symptoms are present throughout the period of observation.
Residual phase. Occurs after remission of prominent psychotic symptoms
Classification of Longitudinal Course (con’t.)
Six Types (applied only after at least 1 year since initial onset of active-phase symptoms):
1. Episodic With Interepisode Residual
Symptoms, also specify if:
With Prominent Negative Symptoms
2. Episodic, also specify if:
With Prominent Negative Symptoms
Classification of Longitudinal Course (con’t.)
3 . Continuous (prominent psychotic symptoms are present throughout the period of observation) also specify if:
With Prominent Negative Symptoms
4. Single Episode in Partial Remission; also specify if: With Prominent Negative Symptoms
5. Single Episode in Full Remission
6. Other or Unspecified Pattern
Treatment of Schizophrenia
Treatment is multi-faceted:
Antipsychotic drugs
Psychological therapy
Social rehabilitation
Family support
Community care
Treatment (continued)
Antipsychotic Drugs
More than two dozen antipsychotic drugs are available.
These drugs reduce days in the hospital and number of hospitalizations
There is some evidence that starting drugs early on may improve (or even “cure”) the severity of the disease.
Treatment (continued)
Psychological Treatment
Individual psychotherapy for people with schizophrenia must be done very carefully, because introspection and selfdisclosure may cause intense emotions and even a psychotic episode
What seems best is practical advice and support, helping the client to distinguish reality from illusion, and setting specific goals
Group therapy can be helpful for it provides an opportunity to be with others in the same situation and learn from them.
Treatment (continued)
Social Rehabilitation
Social skills training has been very helpful, for it teaches (through role-playing sessions) how to live in the community.
Treatment (continued)
Family Support
In working with families, a new approach is family crisis management, which gives information to family members about schizophrenia, teaches them to communicate better with one another, and trains them in identifying and solving specific problems that arise within the family.
Treatment (continued)
Community Care
Although government funding is inadequate, people with schizophrenia need much community support, such as shelter, care, companionship, job counseling, and rehabilitation.
A whole team, including family members, social workers, physicians, nurses, psychotherapists, vocational counseling, and others are essential.
Case managers are essential, because they serve as advocates, monitor treatment (including taking medication), represent clients at welfare hearings, and accompany them to appointments.
Prognosis
Remember the recovery from schizophrenia by
Nobel Prize-winning scientist, John Nash, as told in the biography and film, A Beautiful Mind.
Five long-term studies in the last twenty years have shown improvement even among those who seemed hopelessly ill.
According to Grinsponn & Bakalar (1990), people with schizophrenia show a fairly high rate of recovery
– usual partial, sometimes complete.
About 10% require permanent hospitalization
About 25% require a high degree of supervision and care for most of their lives
50-75% recover some capacity to care for themselves, work, and participate in society
15% are able to live independently without medications or other treatment
Schizophrenia is a terrible burden to those who suffer from it. However, it is important that those, who care for people with schizophrenia, show by their words, actions, and attitudes that they believe recovery is possible. To deny that reality, either explicitly and implicitly, betrays hope and discourages healing.
Other Psychotic Disorders
Schizophrenia-Like Disorders (3 types)
1.
Schizophreniform Disorder (p. 317)
This category is for clients who have
all the symptoms of schizophrenia, but for only one to six months – less than the time specified for Schizophrenia and more than the time for Brief
Psychotic Disorder.
Impaired social or occupational functioning is not required.
Schizophreniform Disorder (con’t.)
Specifiers
With Good Prognostic Features – if two of the following are present:
Onset of psychotic symptoms are within 4 weeks of the first noticeable change in usual behavior or functioning
Confusion or perplexity at height of psychotic episode
Good premorbid social and occupational functioning
Absence of blunted or flat affect
Without Good Prognostic Features
Schizophreniform Disorder (con’t.)
Course
About 1/3 recover within the 6-month period and receive Schizophreniform as a final diagnosis
Remaining 2/3 progress to a diagnosis of
Schizophrenia or Schizoaffective Disorder
Other Psychotic Disorders
Schizophrenia-Like Disorders
2. Schizoaffective Disorder
For at least one month, these clients have had symptoms of Schizophrenia; at the same time, they have prominent symptoms of depression, mania, or mixed episode.
The depression symptoms must meet Criterion A1, p. 312
A hard diagnosis – requires observation over time and multiple sources of information
Specifiers
Bipolar Type
Depressive Type
Other Psychotic Disorders
Schizophrenia-Like Disorders
3.
Brief Psychotic Disorder
These clients have at least one of the basic psychotic symptoms for less than one month.
Specifiers
With Marked Stressor(s): Symptoms occur in response to events
Without Marked Stressor(s): Symptoms do are not in response to events
With Postpartum Onset: Symptoms occur within 4 weeks of birth
Three Psychotic Disorders form a Continuum: Based on duration of episode
Brief Psychotic Disorder (duration 1 day to 1 month)
Schizophreniform Disorder (duration 1 month to 6 months)
Schizophrenia (duration more than 6 months)
Disorders with Delusions
Delusional Disorder. Although these clients have delusions (which are not bizarre), they have none of the other symptoms of Schizophrenia
Shared Psychotic Disorder (Folie a Deux)
This condition is diagnosed when a client develops delusions similar to those held by a relative or other close associate(s).
Other Psychotic Disorders
Psychotic disorder Due to a GMC
A variety of medical and neurological conditions can produce psychotic symptoms.
Substance-Induced Psychotic Disorder
Alcohol or other substances can cause psychotic symptom
Psychotic Disorder NOS
This is for clients with symptoms that do not seem to fit any of the specified categories.
Disorders with Psychosis as a Symptom
Mood disorder with psychosis. Clients with severe
Major Depressive Episode or Manic Episode can have hallucinations and mood-congruent delusions.
Cognitive disorder with psychosis. Many demented clients have hallucinations or delusions
Personality Disorders. Clients with Borderline
Personality Disorder may have transient periods
(minutes or hours) when they appear delusional.
Disorders that Masquerade as Psychosis but are not
Specific Phobia. Some phobic avoidance behaviors can appear quite strange without being psychotic.
Mental Retardation. These clients may at times speak or act bizarrely.
Somatization Disorder. Sometimes these clients will report pseudo-hallucinations or pseudo-delusions.
Factitious Disorder. May feign delusions or hallucinations to obtain hospital/medical care
Malingering. May feign delusions or hallucinations to obtain money (insurance of disability payments), avoid work (such as military), or avoid punishment.