CHAPTER 4 PRENATAL DEVELOPMENT AND BIRTH
advertisement

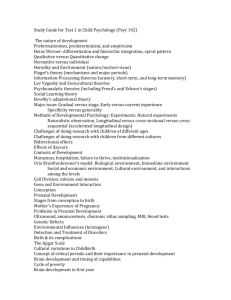
CHAPTER 4 PRENATAL DEVELOPMENT AND BIRTH Learning Objectives • How does development unfold during the prenatal period from conception until the time of birth? • How does prenatal behavior of the fetus relate to postnatal behavior of the infant? Prenatal Development • Time of fastest development in life span • Environment extremely important • Conception – Ova travels from ovary to uterus – Penetration by 1 of 300-500 sperm – Outcome: Single-celled ZYGOTE Prenatal Stages • Germinal period: Days 1-14 – Implantation: One-half are successful – Miscarriage: 15% to 50% • Embryonic period: 3rd to 8th week – Organogenesis, Sexual differentiation • Fetal period: 9th week – birth – Proliferation, Migration – Differentiation of stem cells – Ends in tremendous brain development Learning Objectives • How and when do various teratogens affect the developing fetus? • How can you summarize the effects of teratogens during the prenatal period? • How do maternal age, emotional state, and nutrition affect prenatal and neonatal development? • What about the father’s state - can this influence development? Prenatal Environment • Reciprocal influence – Person and environment – Good and bad influences important • Teratogen: Environmental agent – Harms the developing fetus – Critical Period: Organogenesis – Dosage and duration – Genetic make-up: Susceptibility • The critical periods of prenatal development. Teratogens are more likely to produce major structural abnormalities during the third through the eighth prenatal week. Note, however, that many organs and body parts remain sensitive to teratogenic agents throughout the nine-month prenatal period Teratogens: Drugs • Thalidomide (for morning sickness) – All or parts of limbs missing • Tobacco: Miscarriage, low birth weight, SIDS, slows fetal growth • Alcohol: FAS – Small, facial deformities, retardation • Cocaine: Processing difficulties • (A) Characteristic features of a child with fetal alcohol syndrome (FAS). • (B) Child with FAS, illustrating many features in the drawing. Such children may also have cardiovascular and limb defects. Teratogens - Diseases • Rubella (German Measles) – Blind, deaf, heart, brain • Syphilis: Miscarriage, blind, deaf, heart, brain – After 18th week • AIDS: Mothers transmit to babies (15%-35%) – Prenatally, perinatally, postnatally Teratogens: Environmental Hazards • Radiation: MR, leukemia, cancer, mutations, spontaneous abortions, etc. – Avoid X-rays when pregnant • Pollutants – In air and water – Lead: MR (also postnatally) The Mother’s State • Age: Typically age 16-35 – 15 or younger don’t seek prenatal care • Birth complications, low birth weight – Over 35:Miscarriage, Down Syndrome (father’s age also) • Emotion: Stress can stunt fetal growth – Positive outlook most helpful • Nutrition: 25-35 lb weight gain – Malnutrition: Smaller neurons, brain, child The Father’s State • Research limited except for genetic contribution • Father’s age can also be influential – Over 35: Increased number miscarriages, heart defects, Down Syndrome – Over 50: Higher risk for schizophrenia • Exposure to environmental toxins – Radiation, anesthetic gases, pesticides – Damage to genetic material in sperm Postnatal Depression • Baby Blues: mild, common • Clinical depression: 1/10 – Previous depression common • Children of Depressed Mothers – Insecurely attached, less responsive – Negative to other children The Father’s Experience • Accepted, expected in delivery rooms • Attend prenatal classes with wife • Experience described as a significant event • Anxiety, stress common during delivery • Relief, pride, joy when baby is born The Neonatal Environment • Culture, early socialization, health status – E.g., low birth-weight babies (8% in US) • Less than 5½ lbs • Strongly linked to low SES • Environment: Neonatal intensive care • Risk: Blindness, deafness, CP, autism, cognitive, and later academic problems • Parenting must be attentive, responsive • Modern technology permits survival of younger and smaller babies, but many experts believe we have reached the lowest limits of viability at 23-24 weeks gestation. Learning Objectives • • • • What are the advantages of breast feeding? Are there disadvantages of breast feeding? How can at-risk newborns be identified? What treatments are available to optimize development of at-risk babies? • To what extent are the effects of the prenatal and perinatal environments long lasting? • What factors influence whether effects are lasting? Breast or Bottle? • Breast feeding most natural nutrition • Practices vary across cultures • Health benefits great for breast-fed infants – At least first 6 months recommended • More likely to bottle feed: Factors – Younger, low SES, less education, employed, African American • US values toward breast feeding ambivalent Low Birth-Weight Babies • < 5½ pounds: “Small for date” or “preterm” – Leading cause of infant mortality – 8% of all births, 65% of all infant deaths • Factors: Low SES, smoking, stress, multiples • Worse for minority, poverty, single-parent children • For most, significant catch-up growth Low Birth-Weight Infants • Greater risk for blindness, deafness, CP, autism, health problems - especially respiratory problems Factors Helpful for LBW Infants • Breastfeeding, skin-to-skin contact, massage • Responsive parenting, intellectual stimulation • Early intervention programs work with parents – Childcare education and support – Growth-enhancing home environment • Consistently attentive, responsive parenting Risk and Resilience • Not all high-risk infants have problems • Werner: Kauai Longitudinal study (40 yrs) • Findings: – Effects decrease over time – Outcomes depend on postnatal environment – Protective factors • Personal resources • Supportive postnatal environment