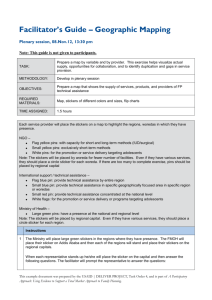
here - Global Family Initiative

B
ASELINE
C
HILD
N
EEDS
A
SSESSMENT
L AFTO S UB -C ITY , A DDIS A BABA
J
ENNIFER
F
OTH
M
ASTERS
C
ANDIDATE
, BUSPH
I
NTERNATIONAL
& E
NVIRONMENTAL
H
EALTH
28 A
UGUST
2012
TABLE OF CONTENTS
LIST OF TABLES and ACRONYMS………………………………………………………iii
INTRODUCTION…………………………………………………………………………….1
P
ROBLEM
S
TATEMENT
………………………………………………………………...1
O BJECTIVES …………………………………………………………………………...1
QUANTITATIVE NEEDS ASSESSMENT SURVEY……………………………………..2
S TUDY S ETTING ……………………………………………………………………....2
S
TUDY
D
ESIGN
, P
OPULATION
,
AND
E
LIGIBILITY
……………………………………..2
S URVEY I NSTRUMENT ………………………………………………………………...2
E THICAL C ONSIDERATIONS …………………………………………………………..3
D
F
ATA
C
OLLECTION
INDINGS
, E
NTRY
,
AND
A
NALYSIS
………………………………………...3
……………………………………………………………………………..4
H OUSEHOLD C HARACTERISTICS …………………………………………….....4
C
AREGIVER
D
EMOGRAPHICS AND
C
ARE
-S
EEKING
B
EHAVIOR
…………………….5
C
C
HILD
HILD
D
H
EMOGRAPHICS
EALTH AND W
………………………………………………………...8
ELL -B EING ………………………………………………9
D
L
ISCUSSION
IMITATIONS
………………………………………………………………………….10
………………………………………………………………………...12
QUALITATIVE INTERVIEWS……………………………………………………………13
C ONCEPTUAL F RAMEWORK ………………………………………………………….13
R
ESEARCH
Q
UESTION
………………………………………………………………..13
R ECRUITMENT AND S AMPLING M ETHODS …………………………………………...13
S TUDY P ARTICIPANTS ……………………………………………………………….13
D
ATA
C
OLLECTION AND
A
NALYSIS
………………………………………………….13
F
INDINGS
……………………………………………………………………………15
I MPORTANCE OF OVC C AREGIVER T RAINING ………………………………….15
I MPORTANCE OF P SYCHOSOCIAL S UPPORT FOR OVC S …………………………15
C
APACITY OF
OVC S
UPPORT
O
RGANIZATIONS
…………………………………16
N ETWORKING AND I NFORMATION -S HARING ……………………………………17
D ISCUSSION …………………………………………………………………………18
L
IMITATIONS
………………………………………………………………………...21
I MPLICATIONS FOR F UTURE I NTERVENTIONS ………………………………………...22
REFERENCES……………………………………………………………………………..24 ii
LIST OF TABLES
Table Number Title Page
Table 1
Table 2
Table 3
ACRONYMS
ARI
CCRDA
CDC
CNA
CSA
DHS
EDHS
HEW
HH
IMCI
NGO
OVC
PPS
TA
UNHABITAT
UNICEF
WHO
INTRODUCTION
Household Characteristics
Caregiver Demographics and Care-Seeking Behavior
Child Demographics, Health, and Well-Being
4
6
8
Acute Respiratory Infection
Consortium of Christian Relief and Development Associations
Centers for Disease Control and Prevention
Child Needs Assessment
Central Statistical Agency of Ethiopia
Demographic and Health Survey
Ethiopia Demographic and Health Survey
Health Extension Worker
Household
Integrated Management of Childhood Illness
Non-governmental organization
Orphaned and vulnerable children
Probability proportional to size
Traditional Authority
United Nations Human Settlements Program
United Nations Children’s Fund
World Health Organization iii
P ROBLEM S TATEMENT
There are nearly five million orphans under age 17 in Ethiopia, constituting 11% of all children in Ethiopia. Of these children, approximately 750,000 have lost either one or both parents to
AIDS (UNICEF 2007). The HIV/AIDS epidemic has significantly increased the number of child-headed households, altered established cultural patterns of child care, and put a considerable strain on social safety nets in Ethiopia (Government of Ethiopia 2007). An estimated 18% of Ethiopian households - 42% of which are female-headed - care for orphaned children (UNICEF 2007). The proportion of female-headed households is much higher in urban than in rural areas, and single-person households are far more common in urban (13%) than rural areas (4%) (CSA and ICF 2012). Accordingly, Addis Ababa boasts the lowest proportion of children living with both parents (52%) in the country (ibid). As a result, orphaned and vulnerable children (OVCs) are at increased risk of abuse and exploitation; loss of educational opportunities; abnormal growth and development; and lack of access to basic health care (ibid).
Moreover, according to a 2007 report by UNICEF Ethiopia, nearly 50% of AIDS orphans and
46% of non-AIDS orphans in Ethiopia lack adequate sources of food and water, forcing many to beg or drop out of school in order to secure a daily meal (Government of Ethiopia 2007).
Unfortunately, child vulnerability in Ethiopia extends beyond the context of HIV/AIDS. The current child mortality rate is 31 deaths per 1,000 children surviving to 12 months of age, while the under-five mortality rate is 88 deaths per 1,000 live births (CSA and ICF 2012). Overall, 67% of all under-five child deaths in Ethiopia occur before a child's first birthday. Forty-four percent of all children in Ethiopia are stunted (short for their age), with stunting rates of 46% and 32% in rural and urban areas, respectively (ibid). Ten percent of all Ethiopian children are wasted (thin for their height), with 10% of rural children wasted compared to 6% of urban children. Twentynine percent of all children in Ethiopia are underweight due to stunting, wasting, or a combination of the two (30% of children in rural areas versus 16% in urban areas) (ibid). Though many of the statistics quoted above represent a decrease from the 2005 EDHS, they are still alarmingly high.
The majority of OVCs are believed to reside in the capital city of Addis Ababa.
Lafto is an emergent and rapidly urbanizing sub-city of Addis Ababa and the programmatic center for
Betasab, a 501(c) 3 non-profit organization that provides education, health care, and a secure family-like environment in a group home setting to OVCs. For this reason, Lafto sub-city has been selected as the geographic area of focus for a baseline child needs assessment that will establish a benchmark for the implementation, monitoring, and evaluation of child sponsorship and community development programs by Betasab.
O BJECTIVES
The overall objective of this study is to determine the needs of households with children age 8 and under in Lafto sub-city through the collection of quantitative and qualitative data that will facilitate the implementation, monitoring, and evaluation of effective child sponsorship and community development programs by Betasab. Specifically, the purpose of this study is:
• To provide information that will help Betasab develop child sponsorship and community
2
development programs that will strengthen the quality of OVC care and support;
• To provide a framework for demonstrating progress toward the achievement of the goals and objectives of Betasab's child sponsorship and community development programs;
• To increase accountability, monitoring, and evaluation within these programs; and
• To contribute to the documentation of lessons learned in OVC programming and the use of participatory research methods.
QUANTITATIVE NEEDS ASSAESSMENT SURVEY
S TUDY S ETTING
Ethiopia is one of the most rapidly urbanizing countries in the world, with approximately
120,000 new residents added each year to Addis Ababa alone (UNHABITAT 2007). Lafto subcity is one of ten sub-city administrations in Addis Ababa and the fastest-growing residential and commercial sub-city in the capital.
According to 2005 data from the Central Statistical Agency of
Ethiopia (CSA), Lafto sub-city has an estimated total population of 228,623 of whom 114,255 were males and 114,368 were females (CSA 2007). Other estimates, however, claim the current population is over 400,000.
S TUDY D ESIGN , P OPULATION , AND E LIGIBILITY
A cross-sectional survey of households in Woredas 2 and 12 of Lafto sub-city was conducted from May 5-15, 2012. The survey was administered by twelve Health Extension Workers
(HEWs) (six per Woreda) to a random sample of 500 households (250 per Woreda). Pre-defined clusters within each Woreda were selected as the sampling areas to ensure extensive and representative coverage of each Woreda. HEWs administered the survey to the first household they encountered, and every third household after that, to ensure randomness.
The study population for this survey was children age 8 and under, their primary caretaker, and their fellow household members. In order to be eligible to participate in the survey, participants were required to be living in Woredas 2 or 12 of Lafto sub-city during the study period and to have at least one child age 8 or under currently living in the household.
S URVEY I NSTRUMENT
The survey instrument is an anonymous survey questionnaire. The survey was derived from the
Child Needs Assessment (CNA) Tool Kit, which was developed by The Task Force for Child
Survival and Development at the request of the World Bank's Early Child Development Team.
The CNA survey instrument has been pilot tested in Zimbabwe for quantitative data collection and consists of both closed and open-ended questions designed to collect the following information from selected households:
• Household demographic information : including age, sex, parental survivorship, individual health status, education level, and activities of individuals;
• Household access to resources : including access to water, toilets, farm land, modes of transportation;
3
• Livelihood activities : including agricultural production and sales, other sources of cash income, borrowing, etc.; and,
• Household livelihood outcomes : including estimates of food consumption per family member and coping strategies for addressing food insecurity.
The survey is broken down into five parts. The first part consists of questions pertaining to the demographic characteristics of all household residents (i.e. age, gender, etc.) and household characteristics such as water sources, toilet facilities, and sources of income. The second part of the survey contains questions relating to sources of external support received by the household
(i.e. food, clothing, money, etc.) and sources of caretaker income. The third part contains questions concerning the health status of the caretaker and his/her ability to care for the children age 8 and under in the household. The fourth part pertains to the material well-being, daily activities, physical and mental health of children age 8 and under in the household. The fifth and final part of the survey involves taking limited growth measurements for each child age 8 and under in the household.
E THICAL C ONSIDERATIONS
Approval was obtained from the offices of both the Ministry of Education and the Ministry of
Health in Lafto sub-city. Informed written consent was obtained from each participant before they were enrolled in the study. Participants were asked to sign a consent form, written in
Amharic, outlining the study's objectives, the nature of the participant's involvement, the risks and benefits of participating in the study, and the confidentiality of their personal information and survey responses. Study participants were informed that their participation in the study was entirely voluntary and that they could refuse to answer questions and/or terminate the survey at any time. Confidentiality was further ensured through the removal of personal identifiers from completed survey questionnaires.
D ATA C OLLECTION , E NTRY AND A NALYSIS
Data was collected from May 5-15, 2012 by trained HEWs administering pre-tested survey questions in Amharic. HEWs were trained by two professionals using the CNA Tool Kit Training
Manual, which covered topics such as interviewing techniques, household selection, and participant confidentiality. For the first two days of data collection, HEWs administered the survey in pairs so that they could get comfortable with the survey procedure and serve as a check to each other. Completed surveys were submitted to the HEW Supervisor from each Woreda at the end of each day and checked for errors.
Data were entered by three professional data entry clerks into CS Pro, cleaned, and then analyzed by the project investigator using SPSS statistical software. During analysis, frequencies, percentages, and means of different variables were determined to provide a baseline understanding of household, caretaker, and child health needs in both Woredas.
F INDINGS
4
H OUSEHOLD C HARACTERISTICS
Mean household size in the study area was 4.11 rooms per household ( n =498), with an average of 3.98 and 4.23 rooms per household for Woredas 2 and 12, respectively. According to the data,
49.8% of all households in the study area get their drinking water from the public tap. However, only 19.7% of Woreda 12 households get their drinking water this way, compared to 79.9% of
Woreda 2 households. 38.8% of households have their drinking water piped into the yard and
10.8% have water piped directly into the home (See Table 1 for breakdown by Woreda). Inter-
Woreda differences were evident in the type of toilet facilities present in the household, particularly in the usage of improved pit latrines (77.2% of Woreda 2 households; 30.5% of
Woreda 12 households) and traditional pit latrines (4.5% of Woreda 2 households; 56.9% of
Woreda 12 households).
Only 0.8% of all households have a toilet that flushes to a sewage system or septic tank. See Table one for detailed information by Woreda.
Table 1. Household Characteristics (n=498)
Category/Variable Number (% w/in Woreda) Missing
W2 W12
0 1 Main Material of Floor
Wood
Dirt
Tile
Concrete
Main Materials of Walls
Brick
Mud
Tin
Cement
Grass/Thatch
Plastic
Main Materials of Roof
Iron/Material sheets
Grass/Thatch
Shingles
Plastic
Wood
Other
Main Source of Drinking Water
Piped into dwelling
Piped into yard/plot
Public tap
Protected spring
Main Toilet Facility
Flush to sewage system/septic
Pour flush latrine
Improved pit latrine (i.e. VIP)
Traditional pit latrine
Open pit
No facilities/bush/field
Sources of Household Income
186 (74.7)
3 (1.2)
5 (2.0)
1 (0.4)
24 (9.6)
30 (12.0)
11 (4.4)
39 (15.7)
199 (79.9)
0 (0.0)
1 (0.4)
38 (15.4)
190 (77.2)
11 (4.5)
6 (2.4)
0 (0.0)
W2
0 (0.0)
163 (65.5)
1 (0.4)
85 (34.1)
9 (3.6)
169 (67.9)
3 (1.2)
66 (26.5)
1 (0.4)
1 (0.4)
240 (96.8)
3 (1.2)
0 (0.0)
5 (2.0)
0 (0.0)
0 (0.0)
43 (17.3)
154 (61.8)
49 (19.7)
3 (1.2)
3 (1.2)
3 (1.2)
75 (30.5)
140 (56.9)
21 (8.5)
4 (1.6)
W12
2 (0.8)
168 (67.7)
5 (2)
73 (29.4)
12 (4.9)
215 (87.0)
4 (1.6)
15 (6.1)
1 (0.4)
0 (0.0)
0
0
0
3
2
1
0
3
5
Salaried work
Casual labor
Gifts/donations
Self-employment
Farming
Vending
Other
Begging
Company
NGO
Property rent
Raising livestock
Relatives abroad
Temp. employment
Meals per Day (Adult HH Members)
Did not eat every day
1 meal/day
2 meals/day
3 meals/day
>3 meals/day
61 (24.7)
150 (60.7)
35 (14.1)
24 (9.6)
2 (0.8)
11 (4.4)
18 (7.3)
5 (2.0)
1 (0.4)
5 (2.0)
0 (0.0)
1 (0.4)
1 (0.4)
1 (0.4)
1 (0.4)
5 (2.0)
137 (55.2)
104 (41.9)
1 (0.4)
96 (38.7)
136 (54.6)
5 (2.0)
36 (14.5)
5 (2.0)
15 (6.0)
2 (0.8)
0 (0.0)
0 (0.0)
0 (0.0)
1 (0.4)
0 (0.0)
1 (0.4)
0 (0.0)
2 (0.8)
3 (1.2)
43 (17.3)
168 (67.5)
33 (13.3)
2
2
1
0
1
0
1
14
1 0
2
0
0
1
0
2
0
2
Casual labor is a major source of household income for
57.7% of all households within the study area.
Only 31.7% of households reported receiving income from salaried work, with a slightly higher percentage of
Woreda 12 households
(38.7%) claiming income from salaried work compared to Woreda 2 households (24.7%). There was a notable difference in the percentage of Woreda 2 and Woreda 12 households that receive income in the form of gifts or donations (14.1% and 2%, respectively).
In addition, 7.3% of Woreda 2 households reported receiving income from other sources, compared to only 0.8% of Woreda 12 households. See Table 1 for detailed information by Woreda.
C AREGIVER D EMOGRAPHICS AND C ARE -S EEKING B EHAVIOR
The overwhelming majority (95.8%) of all caregivers are female, 79.4% of them are married, and 7.1% are widowed. Overall, 42.4% of survey caregivers had no formal education, yet the percentage of Woreda 2 caregivers with no formal education was more than twice that of
Woreda 12 caregivers (59.8% and 24.9%, respectively). Likewise, the percentage of Woreda 12 caregivers who finished 12 th grade was nearly twice that of Woreda 2 caregivers (8.8% and
4.4%, respectively). Nearly two-thirds (64.5%) of caregivers do not earn an income, but among those who do earn an income, 59.1% do so from casual labor. Over 15% of caregivers reported that community organizations were their largest source of external support (19.4% Woreda 2;
10.8% Woreda 12). Of those caregivers receiving support, half received assistance with clothing and over 60% received assistance with education expenses. Again, there was a sharp contrast in the percentage of Woreda 2 and Woreda 12 caregivers receiving assistance through clothing donations (59.2% vs. 33.3%) and with education expenses (60.5% vs. 22.2%).
See Table 2 for detailed information by Woreda.
More than half (55%) of all caregivers reported feeling worried about their responsibilities as caregivers for the children in their household, and a higher percentage of those were from
Woreda 12 (64.7%). Of those who reported feeling worried, the majority (79.4%) cited money for school fees and/or daycare as one of their main concerns. Caregivers also expressed concern
6
over money for food (61.8%), though this appears to be of greater concern to Woreda 12 caregivers (70.8%) than Woreda 2 caregivers (48.6%).
Table 2. Caregiver Demographics and Care-Seeking Behavior (n=498)
Category/Variable Number (% w/in
Woreda)
W2 W12
Missing
W2 W12
Gender
Female
Male
241 (96.8)
8 (3.2)
236 (94.8)
13 (5.2)
0 0
1 3 Marital Status
Married
Never married
Divorced
Separated
Widowed
Health Status
Very Good
Good
Fair
Poor
Education Status
No school
1
2 st nd
grade
grade
3 rd grade
4
5
6
7 th th th th
grade
grade
grade
8
9 th th
10
11
grade
grade
grade th th
grade
12 th
grade
grade
College diploma
Other
Sources of Caregiver Income
(among those who earn income, n=177)
Salaried work
Casual labor
Gifts/donations
Self-employment
Vending
Other
Location of Caregiver Work (n=177)
At home
189 (76.2)
17 (6.9)
12 (4.8)
8 (3.2)
22 (8.9)
65 (26.2)
122 (49.2)
47 (19.0)
14 (5.6)
149 (59.8)
2 (0.8)
5 (2.0)
4 (1.6)
17 (6.8)
8 (3.2)
7 (2.8)
9 (3.6)
8 (3.2)
10 (4.0)
15 (6.0)
1 (0.4)
11 (4.4)
3 (1.2)
0 (0.0)
26 (27.4)
58 (61.1)
2 (2.1)
2 (2.1)
5 (5.3)
2 (2.1)
40 (42.1)
203 (82.5)
7 (2.8)
5 (2.0)
18 (7.3)
13 (5.3)
66 (26.7)
139 (56.3)
24 (9.7)
18 (7.3)
62 (24.9)
2 (0.8)
11 (4.4)
23 (9.2)
24 (9.6)
17 (6.8)
22 (8.8)
16 (6.4)
19 (7.6)
14 (5.6)
11 (4.4)
3 (1.2)
22 (8.8)
1 (0.4)
2 (0.8)
19 (23.5)
46 (56.8)
0 (0.0)
10 (12.3)
5 (6.2)
1 (1.2)
21 (26.6)
1
0
0
0
2
0
1
3
7
When asked what symptoms would prompt them to seek treatment for a sick child, 72.3% of all caregivers said that a high fever would cause them to seek medical care. However, less than 20% of all caregivers indicated that they would seek treatment if a child was not able to drink or breastfeed (16.3%); if a sick child became sicker (15.5%); if a child has fast breathing
(4.6%); if a child has difficulty breathing
(8.6%); or if a child had blood in their stool
(4.6%). Over 80% of caregivers indicated that they would first seek treatment for a sick child at a health center. Over 55.3% of caregivers reported seeking medication at a pharmacy or dispensary the last time a child in the household was sick, though there was a significant gap in the percentage of Woreda 2
(68.3%) and Woreda 12 caregivers (42%) who reported doing so. See
Table 2 for detailed information by Woreda.
Away from home
Home and away equally
Sources of concern re
Responsibilities (among those w/ concerns, n=274)
Sending children to school
Money for food
Money for clothes
Housing/money for housing
Other financial concerns
Sick child
Old age/physical limitations
Other
Symptoms in Children Prompting
Care-Seeking Behavior
Unable to drink/breastfeed
Becomes sicker
Fever
Fast breathing
Difficult breathing
Blood in stool
Drinking poorly
Other
Don’t know
Location of Seeking Care for
Children
Hospital
Health center
Dispensary/pharmacy
CHW
MCH Clinic
Private physician
Other
Don’t know
Location of Seeking Medicine for
Children
Hospital
Health center
Dispensary/pharmacy
Private physician
Other
Don’t know
56 (70.9)
2 (2.5)
37 (14.9)
22 (8.8)
77 (30.9)
3 (1.2)
9 (3.6)
199 (80.6)
0 (0.0)
0 (0.0)
5 (2.0)
25 (10.1)
3 (1.2)
6 (2.4)
126 (78.3)
114 (70.8)
63 (39.1)
42 (26.1)
53 (32.9)
29 (18.0)
5 (3.1)
4 (2.5)
33 (13.3)
55 (22.1)
177 (71.1)
4 (1.6)
5 (2.0)
52 (54.7)
3 (3.2)
6 (2.4)
1 (0.4)
16 (6.4)
0 (0.0)
15 (6.0)
213 (85.5)
2 (0.8)
1 (0.4)
0 (0.0)
15 (6.0)
0 (0.0)
3 (1.2)
90 (81.1)
54 (48.6)
48 (43.2)
28 (25.2)
26 (23.4)
5 (4.5)
5 (4.5)
3 (2.7)
48 (19.3)
22 (8.8)
183 (73.5)
19 (7.6)
23 (9.2)
11 (4.4)
64 (25.7)
170 (68.3)
1 (0.4)
1 (0.4)
2 (0.8)
2 (0.8)
133 (54.7)
102 (42.0)
1 (0.4)
0 (0.0)
5 (2.1)
2
0
0
0
0
0
2
6
8
C HILD D EMOGRAPHICS
Nine hundred and fifty-nine children age 0-17 were recorded as living in the surveyed households – 482 from Woreda 2 and 477 from Woreda 12. The mean age of child household members in the study area was 7.15 years, with a mean age of 8.02 years for Woreda 2 and 6.26 years for Woreda 12. Within the surveyed households, 51.6% of all children were female and
48.4% were male. (See Table 3 for breakdown by Woreda ) According to caregivers, 63.5% of all children in the survey area have both biological parents still alive. 9.6% of all children in the survey area have only their biological mothers still alive, with over 90% of those living in
Woreda 2. Only 1.1% of all children in the survey area have only their biological fathers still alive, with 63.6% of those living in Woreda 2. Approximately 15% of all children in the surveyed households are orphans, though the percentage is significantly higher among Woreda 2 households (26.6%) than those in Woreda 12 (2.9%). See Table 3 for detailed information by
Woreda.
Table 3. Child Demographics, Health, and Well-Being
Category/Variable
Gender (n=959)
Female
Male
Orphan Status
Both parents alive (n=609)
Live w/ both parents (n=281)
Live w/ one parent (n=28)
Only biological mother alive (n=92)
Live w/ mother (n=16)
Do not live w/ mother (n=4)
Only biological father alive (n=11)
Live w/ father (n=2)
Do not live w/ father (n=3)
Orphan (n=142)
Health Status (n=449)
Very Good
Good
Fair
Poor
Not enough to eat over past month (n=445)
Every day
2-6 times/week
Few times/month
Once
Never
Reasons for not getting enough to eat
Number (% w/in
Woreda)
W2 W12
255 (52.9)
227 (47.1)
240 (50.3)
237 (49.7)
316 (51.9)
12 (4.3)
10 (35.7)
84 (91.3)
8 (50.0)
3 (75.0)
7 (63.6)
0 (0.0)
1 (33.3)
128 (26.6)
293 (48.1)
269 (95.7)
18 (64.3)
8 (8.7)
8 (50.0)
1 (25.0)
4 (36.3)
2 (100.0)
2 (66.6)
14 (2.9)
62 (30.5)
112 (55.2)
25 (12.3)
4 (2.0)
10 (5.0)
76 (37.6)
27 (13.4)
75 (37.1)
14 (6.9)
78 (31.7)
150 (61.0)
14 (5.7)
4 (1.6)
40 (16.5)
35 (14.4)
39 (16.0)
11 (4.5)
118 (48.6)
9
(n=314)
Money
No one to prepare food
No water/wood/electricity
Other
Material well-being (n=453)
Does not sleep on mattress
Does not have a blanket
Does not have >1 set of clothes
Does not have pair of shoes
Alternate Caregivers (n=448)
Someone living in HH
Family member not living in HH
Friend/neighbor
Day care/Pre-school/School
No one/Child stays alone
Other
Unmet Health Service Needs (n=82)
Healthcare
Medicines
Immunizations
Other
Reason for Unmet Health Service Needs
(n=82)
Time
Money
Transportation/Too far
Other
159 (84.6)
2 (1.1)
2 (1.1)
3 (1.6)
98 (48.0)
126 (61.8)
64 (31.4)
72 (35.3)
119 (58.6)
12 (5.9)
54 (26.7)
2 (1.0)
10 (5.0)
6 (3.0)
58 (87.9)
28 (42.4)
6 (9.1)
1 (1.5)
6 (9.4)
50 (78.1)
6 (9.4)
2 (3.1)
106 (84.1)
6 (4.8)
9 (7.1)
2 (1.6)
74 (29.7)
71 (28.5)
39 (15.7)
56 (22.6)
132 (53.7)
29 (11.8)
67 (27.2)
3 (1.2)
2 (0.8)
19 (7.7)
9 (52.9)
6 (33.3)
6 (33.3)
3 (16.7)
6 (33.3)
4 (22.2)
2 (11.1)
3 (16.7)
Approximately 95% of school-age children, defined by the CNA
Toolkit as those aged 6-
17, and 88% of orphans living in surveyed households from both
Woredas are currently attending school.
Overall, 46.2% of those attending school are male and 53.8% are female, with similar gender ratios present in both Woreda 2 (47.1% male; 52.9% female) and Woreda 12 (44.6% male; 55.4% female) households.
C
W
HILD
ELL
-B
H EALTH AND
EING
Over 30% of caregivers reported that the health of the children in their household is “very good”, and over 55% reported child health to be “good”. Though only 8.7% of caregivers indicated that child health in their household was
“fair”, the percentage of Woreda 2 caregivers reporting fair health (12.3%) was more than double that of Woreda 12 caregivers (5.7%). 24.9% of caregivers reported that children in the household were not getting enough to eat 2-6 times per week over the past month, with the percentage of
Woreda 2 caregivers (37.6%) more than double those of Woreda 12 (14.4%). When asked why children were not getting enough to eat, over 84% of caregivers cited lack of money as a the primary reason.
Nearly 40% of caregivers said that children in their household do not sleep on a mattress, though the percentage was closer to 50% among Woreda 2 households. Woreda 2 households also reported higher percentages of children in the household not having a blanket, more than one set of clothes, or a pair of shoes (See Table 3 for a breakdown by Woreda). Over 50% of caregivers from both Woredas report that there is someone living in the household who generally takes care of the children. However, 5% of Woreda 2 caregivers report that children often stay home alone or have no one to care for them, as compared to only 0.8% of Woreda 12 households.
Overall, 18.4% of all caregivers claim children in their household are not receiving all the health services they need, with the prevalence of unmet needs much higher among Woreda 2
10
households. Among those households reporting unmet child health needs, the most frequently mentioned needs were greater access to healthcare (80.7%); medications (40.5%); and immunizations (14.3%). Again, there were marked differences in the prevalence of unmet needs between the Woredas, particularly regarding access to healthcare and immunizations (See Table
3 for a breakdown by Woreda). When asked why children are not able to access these needed health services, money (65.9%) and time (14.6%) were the two factors cited most frequently by all caregivers. Money was a more prevalent factor for Woreda 2 caregivers, while time was more frequently mentioned by Woreda 12 caregivers. (See Table 3) Unfortunately, these inter-Woreda differences in the type and reason for unmet child health needs cannot entirely be explained by distance from those services, as the average distance traveled to access treatment for sick children was approximately two kilometers for both Woreda 2 and Woreda 12 households.
D ISCUSSION
In general, the survey results indicate that Woreda 2 households are in greater need of assistance across a number of areas. Improved drinking water sources are defined by the WHO as (1) piped water into the dwelling; (2) piped water into the yard/plot; (3) public taps/standpipes; (4) tubewells/boreholes; (5) protected dug wells; (6) protected springs; (7) rainwater collection; or
(8) bottled water (WHO/UNICEF 2010). One hundred percent of households in both Woredas reported having access to either protected springs or piped water into the house/yard. Yet, the percentage of Woreda 12 households that have access to piped water is over three times that of
Woreda 2 households, which fall well below the national average of 95% and the national urban average of 87% (CSA AND ICF 2012).
In comparison to their Woreda 12 counterparts, Woreda 2 households are more dependent on gifts, donations, NGO support, and begging as sources of income, and the percentage of Woreda
2 households receiving support from community organizations, particularly with clothing and educational expenses, is nearly double that of Woreda 12 households. Caregivers in Woreda 2 report lower levels of formal education. Nearly 60% of Woreda 2 caregivers have received no formal education, compared to the national urban average of 28% of all females and 23% of females living in Addis Ababa (CSA and ICF 2012). However, this could be confounded by the age of the caregiver, which, due to data collection errors, we were unable to capture accurately.
Woreda 2 caregivers also report greater concern over money for food than their Woreda 12 counterparts.
These concerns regarding money for food are reflected in the comparative well-being of children from Woreda 2 households, where the percentage of children not getting enough to eat 2-6 times per week over the past month (37.6%) was more than double that of Woreda 12. Children who do not receive adequate nutrition are at greater risk for many health problems, including anemia and Vitamin A deficiency. Anemia is caused by an inadequate dietary intake of iron, folate, and vitamins B and B12, and is associated with impaired mental and physical development and increased morbidity and mortality in children (CSA and ICF 2012). Over 40% of all Ethiopian children, as well as 33% of children living in Addis Ababa, have anemia (ibid). Inadequate consumption of foods such as milk, eggs, fish, and dark green leafy vegetables among children can also lead to a Vitamin A deficiency, which can cause eye damage and increase the severity of measles and diarrheal diseases (ibid).
A higher percentage of Woreda 2 children do not sleep on a mattress or have a blanket, a pair of
11
shoes, or more than one set of clothes, while the percentage of Woreda 2 children who stay home along or have no one to care for them is more than five times that of Woreda 12 children.
Children from Woreda 2 also report a significantly higher percentage of unmet health needs than children from Woreda 12, particularly concerning access to healthcare and immunizations, due largely to a lack of money to pay for these services.
The percentage of households in Woreda 2 (26.6%) caring for orphans is nearly nine times that of Woreda 12 households and significantly higher than the national average (1%) (CSA and ICF
2012). Though Woreda 2 and 12 households report similar percentages of children with both parents still alive, a much smaller percentage of those from Woreda 2 (4.3%) actually live with both parents, well below the national average of 72% (ibid). Additionally, the percentage of children with both parents still alive from Woreda 2 who live with only one biological parent
(35.7%) is almost twice that of children from Woreda 12 and nearly double the national average
(ibid). It is important to note, however, that there was a great deal of missing data on the live-in status of parents, so these statistics should be interpreted with caution.
In certain areas, though, the inter-Woreda differences were minimal.
This was the case with health-seeking behavior among caretakers from both Woredas, with less than 20% of all caregivers indicating that they would seek treatment if a child was unable to drink or breastfeed, if a child had difficulty breathing, or if a child had blood in their stool. This statistic is important given that acute respiratory infection (ARI) and diarrheal diseases are among the leading causes of child morbidity and mortality in Ethiopia and around the world (CSA and ICF 2012).
According to the 2011 Ethiopia DHS, seven percent of children showed symptoms of ARI in the two weeks prior to the survey and only 27% of caretakers of children who had ARI symptoms sought treatment from a health facility, more than double the percentage of caretakers from
Woredas 2 and 12 who said they would seek treatment for symptoms of fast or difficult breathing
(ibid). In terms of diarrhea, 13% of children under age 5 had diarrhea, and 3% had diarrhoea with blood, in the two-week period before the 2011 Ethiopia DHS (ibid). Diarrhea with blood in the stool is often indicative of cholera and other diseases, so it is significant that only 2.4% of
Woreda 2 caretakers and 14.9% of Woreda 12 caretakers, compared to 32% of all caretakers surveyed by the DHS, would seek treatment at a health facility for children with that symptom
(ibid).
Household sanitation was an area in which inter-Woreda differences contradicted the expected outcome.
Improved sanitation is defined by the WHO as either (1) flush toilet; (2) piped sewer system; (3) septic tank; (4) flush/pour flush to pit latrine; (5) ventilated improved pit latrine
(VIP); (6) pit latrine with slab; or (7) composting toilet (WHO/UNICEF 2010). Interestingly, the data show that the percentage of Woreda 2 households using improved pit latrines is more than double that of Woreda 12 households. Traditional pit latrines are the primary method of excreta disposal for more than half of Woreda 12 households, compared to less than 5% of Woreda 2 households. 8.5% of Woreda 12 households use an open pit, well below the national urban average (37%) but almost four times that of Woreda 2 households (CSA and ICF 2012).
L IMITATIONS
There are several limitations to this study. The data are self-reported by the caregivers, and thus the authenticity and accuracy of their responses cannot be externally validated. As evidenced in
12
the extant literature, it is reasonable to assume that statements regarding personal and child health-related quality of life may have been overstated (Theunissen et al. 1998; Agnihotri et al.
2010). Issues pertaining to survey question translation, data collection, and data quality may also have affected the results of the survey. The survey was translated into Amharic from the original
English by general translators in Addis Ababa who were unfamiliar with many of the medical and public health terms mentioned in the survey. Inconsistencies and misinterpretations of certain words and questions were pointed out by HEWs during their training and all possible efforts were made to fix any errors before they were sent out into the field. However, confusion as to the meaning of questions and certain formatting issues undoubtedly contributed to recording errors, which affected the overall quality of the data. For example, many HEWs did not understand that the child module questions should be asked about children in the household age 8 or under only . As a result, some data from the child module, including an entire section on anthropomorphic measurements, had to be thrown out due to uncertainty regarding data quality.
There were also issues with the data entry process. In cases where households had more than one child age 8 or under, HEWs were instructed to record responses to the child module questions for each child age 8 or under. However, the data entry clerks said they could not record multiple responses to the same question for each individual respondent in SPSS. As a result, for households with more than one child age 8 or under, the most extreme responses to the child module questions were entered in order to capture the most “severe” cases. This meant, however, that responses to questions in the child module could not necessarily be synced with other questions in that module or the household identification section of the survey.
Due to the limited availability and public health expertise of the Betasab staff, I was the sole project investigator responsible for organizing and overseeing the process of survey development and translation, HEW training, data collection and data entry. Resource and personnel constraints prohibited me from having the survey thoroughly back-translated and validated to ensure accuracy. Furthermore, national holidays and bureaucratic issues delayed the HEW training so that by the time it was complete, there were only three weeks in which to collect and enter the data. With more time, resources, and personnel, the majority of the aforementioned limitations would have been avoided. Future quantitative research by Betasab should take into account and correct these limitations to facilitate a more in-depth examination of relationships and multivariable associations between certain study variables.
QUALITATIVE INTERVIEWS
C ONCEPTUAL F RAMEWORK
13
The research question and methodology is informed by phenomenology, a theoretical framework that focuses on the exploration of how human beings make sense of experience and transform experience into consciousness, both individually and as shared meaning (Patton 2002).
Phenomenology requires that the researcher thoroughly capture and describe how individuals who have experienced the phenomenon of interest perceive that phenomenon, describe it, judge it, make sense of it, and communicate it to others (ibid). Phenomenological methods are useful for bringing individual perceptions and perspectives to the forefront, thereby challenging structural or normative assumptions concerning the phenomenon of interest (ibid). For these reasons, phenomenology was selected as the theoretical framework for this research.
R ESEARCH Q UESTION
The purpose of this research is to better understand the physical and psychosocial issues facing
OVCs in Addis Ababa, as well as the overarching structural factors that affect their ability to access physical and mental health services.
R ECRUITMENT AND S AMPLING M ETHODS
The sample for this research was determined using the method of selective sampling. Selective sampling is a process in which individuals are selected according to the goals of the research and typically involves a calculated decision on the part of the researcher to sample a specific location or group according to preconceived and predetermined dimensions (i.e. time, space, identity, or power) (Coyne 1997). Potential interviewee organizations were identified through online searches and the directory of the Consortium of Christian Relief and Development Associations
(CCRDA), an indigenous, non-profit umbrella organization. Organizations were contacted via email and one-on-one interviews were set up with appropriate staff members from those organizations that responded.
S TUDY P ARTICIPANTS
Semi-structured, individual in-person interviews were conducted with two clinicians; three staff members from large, international OVC support organizations; and two staff members from local
OVC support organizations. Three interviewees were organization directors, two were program managers, one was a doctor, and one a nurse. All interviewees were male with the exception of the director of one local organization. Interviewee ages ranged from early-thirties to mid-sixties.
Interviewees working in different positions and from different organizational backgrounds were selected in order to obtain the diverse perspectives of individuals who interact with OVCs in different contexts.
D ATA C OLLECTION AND A NALYSIS
Data were collected from March to May 2012. Interviewees were asked questions concerning the physical and psychosocial health issues affecting OVCs in Addis Ababa, as well as any barriers that exist to providing and accessing OVC support services. Interviews were recorded in realtime by hand or on a computer. All interviewees were informed that their names and other identifying information would not be attributed to their responses and would not be used for purposes other than this research. Interviews were both recorded and transcribed on the computer, and recordings were reviewed immediately following the interview to correct spelling errors, improve transcript readability, and fill in any information missed during transcription.
Once the data collection was complete, data were organized by interview for coding. Three codes
14
were determined prior to the start of data collection: the lack of adequate nutrition among OVCs
(NUTR), the lack of hygienic practices among OVCs (HYG), and the lack of coordination among OVC support organizations (COORD). These codes were determined based upon a review of the extant literature (i.e. Andrews et al. 2005) and reports from international organizations including UNICEF, Save the Children, and CARE.
Transcripts were analyzed using the process of conventional content analysis (Hsieh and
Shannon 2005). Each interview transcript was reviewed three times. The first review was conducted to familiarize the researcher with the interviewee’s responses. During the second review, key phrases, words, and ideas were highlighted that were either (a) particularly powerful or well-spoken; (b) very descriptive of a particular theme; (c) recurrent throughout multiple interviews; or (d) unrelated to a particular theme but very interesting and deserving of recognition (Jabson 2011). Themes that emerged during the second transcript review were developed further and included as emergent codes. Predetermined and emergent codes were then assigned during the third review of each interview transcript. Themes, patterns, and relationships between coded categories were identified during the third transcript review and codes were adjusted, refined, and merged to better reflect those patterns and relationships.
Six emergent codes were identified during the transcript review process. ABUSE was a code used to identify and capture all references to caregiver abuse of OVCs. The manifestations of this abuse were included as code subcategories and consisted of sexual abuse of OVCs (SEX); conscious neglect of OVCs by caregivers (NEGL); and the inability to care for OVCs due to caregiver economic circumstances (ECON). The TRAIN code was used to encapsulate statements regarding the importance of, and need for, training for both caregivers and OVCs themselves. The three subcategories of this code included the need to increase caregiver awareness of OVC health issues and services (AWARE); the need to increase overall caregiver capacity (CAP); and the need for vocational and other skills training among OVCs (SKILL). The
PSYCH code was used to capture all references made to the need to better address the psychosocial issues affecting OVCs. Difficulty integrating into a new environment
(INTEGRATE) and the effect of separating OVCs from their siblings, parents, extended family and community (SEP) were identified as important factors contributing to the psychosocial problems of OVCs, and were thus included under the PSYCH code.
The GOVT code was created for references made to the lack of government support or prioritization of OVC programming, with subcategories addressing the lack of a national child policy and/or child-friendly courts (LEGAL); the lack of national-level OVC statistics (DATA); the lack of monitoring and evaluation of OVC support organizations by the government (M&E).
Related to that, the CAPACITY code was used to encapsulate statements regarding the lack of organizational capacity among OVC support organizations in Ethiopia, with lack of resources for
OVC programming (MONEY) and the lack of psychological professionals in Ethiopia (PROF) comprising the most referenced code subcategories. Finally, the ALTCARE code was created to identify references to the need for alternative childcare options in lieu of adoption. Three subcategories for the COORD code were also identified during the transcript review process: the redundancy of OVC services (REDUN), the need for networking and information-sharing among
OVC support organizations (NETWORK), and the tendency for OVC support organizations to prioritize daily operations over networking and program coordination (PRIORITIES).
15
F INDINGS
In reviewing the coded data, four distinct yet often overlapping themes emerged as significant factors affecting the health of OVCs in Addis and their access to support services: (1) the importance of, and need for, caregiver training; (2) the importance, and lack of, psychosocial support for OVCs; (3) the lack of professional and financial capacity among OVC support organizations; and (4) the need for increased networking and information-sharing among those organizations. The following sections provide an analysis of interrelationships among these four themes across interviewee responses.
I
MPORTANCE OF
OVC C
AREGIVER
T
RAINING
Of all the predetermined and emergent codes, the importance of training caregivers in order to increase their awareness of OVC health issues and services was the one most frequently mentioned. Almost every interviewee highlighted the role that lack of awareness among OVC caregivers plays in the high levels of malnutrition and poor hygiene commonly observed among
OVCs. As one interviewee bluntly observed, “they [caregivers] don’t know what is important for the development of a child.” In discussing a nutrition program run by their organization, one interviewee described how OVC food packages were “being shared among the family. So the impact of all…food support on that specific child [was] very low.” Another interviewee highlighted the problem of hygienic practices related to food, as well as personal care:
Most of them we see for hygiene, especially the small kids. You try to tell them [about being hygienic], but they forget it. Without cleaning their hands, they eat and they get different parasites… [Also] when you prepare food, it's common to keep leftover food until next day because there is not enough food in Ethiopia. But without refrigeration, it can make them [the kids] sick.
Though poverty was often cited as an explanation for this lack of personal and food hygiene, the problem is by no means limited to low-income households. As one interviewee explained, many young children in middle- and high-income households in Addis Ababa “are being attended by a servant or a house maid and these type of individuals come from rural areas so they don’t have the awareness of how to keep sanitary conditions in the home.” Though rural caregivers were also criticized for not knowing “the area of the clinic, or how to bring the child to the clinic,” they are not the only ones at fault. Even caregivers from high-income households “don’t bring the kids to the clinic. They usually prescribe medications by themselves. They buy syrups from the pharmacy so by the time they come to the clinic, the kid is so weak that they may need an IV or a referral.” The need for caregiver training on child nutrition, hygiene, and health service availability thus extends across socioeconomic status.
I MPORTANCE OF P SYCHOSOCIAL S UPPORT FOR OVC S
The importance of psychosocial support for OVCs was a major theme that arose during the interviews, particularly those with OVC support organization staff. One of the most commonly cited sources of psychosocial problems among OVCs was difficulty integrating into a new environment. More than half of the interviewees worked for organizations that provide OVC care and services in a group home model in which seven to nine children are placed in homes with
16
“mothers” and “aunties”, group-home staff who provide around-the-clock care for the OVC and his new “brothers” and “sisters.” As one interviewee explained:
When the child first comes…because this is completely new family, new environment, the common experience is that the child fears to integrate. So you may see some psychosocial disturbances like crying, sadness, instability… Even sometimes bedwetting is common also. This is expected.
Feelings of loneliness, depression, and shyness among OVCs were frequently linked to the difficulty, or fear of, integrating into a new environment, with a new family and a new home.
Moreover, many OVCs have experienced abuse or trauma, either at the hands family members or while living on the street. As a result, “they might be very reserved to get to know other people, to express themselves. They might have their own fears to trust other people.”
In addition to the difficulties and fear of integration, many interviewees highlighted the adverse psychological effects that may occur when OVCs are separated from their siblings, parent(s), extended family and community. As one interviewee explained:
[When admitting OVCs into a group home] it’s better to admit children from that specific area, where the village is located…just to keep the intimacy with their extended families…just so that it’s easy for them to get access… They cannot also forget the language, they cannot forget their religion and everything.
A number of interviewees also emphasized the efforts being made by their respective organizations to keep OVCs connected to their families and communities, whenever possible, in the interest of “their psychosocial development, their well-being.” In cases where OVCs are found to have extended family, one interviewee described how his organization is “trying to keep the children wherever they are, instead of admitting them to our children’s home…we [are] trying to convince their extended families to keep them.” Even in cases where the extended family is unable to keep the OVC in their home, efforts are made to maintain familial and community ties, such as “Family Day”, during which the OVCs’ extended family members are allowed visit them at the group home.
C APACITY OF OVC S UPPORT O RGANIZATIONS
The neglect of OVC psychosocial issues frequently overlapped with statements regarding a lack of capacity among OVC support organizations to address all the needs of OVCs. Even the large budgets of many international OVC support organizations are “like a drop in the ocean...[The] gap between the need and the available resources is one of the problems which is really hindering the OVCs not getting the required services.” This lack of financial capacity was attributed to difficulties mobilizing resources, both domestically and internationally. One interviewee from a local OVC support organization lamented his inability to raise more funds
For young leaders like me, it is not easy… You know, connections and international exposures are very, very limited in Ethiopia for most local organizations… [L]ocally emergent organizations face problem with resource mobilization, grant writing, capacity building, and, you know, securing funds to do more things. They may have good ideas –
17
brilliant ideas – but it is very, very difficult to meet the needs of these children by raising funds locally.
Though international OVC support organizations may have greater access to funding, resource mobilization still presents a problem for many organizations due to the influence international donors have in determining the focus of OVC support programs. As one interviewee explained, many programs “come with already determined or prescribed criteria from the donors… based on what they may think is appropriate for the OVC.” As a result, donor-driven OVC programs often ignore the diverse needs of OVCs, some of whom are “disabled, some of them are abandoned, some of them are orphans, some of them are with their parents but their parents are unable to provide their needs.” These diverse needs - particularly psychosocial needs - are often overshadowed by the preconceived ideas and personal interests of donors.
However, it is not only a lack of financial capacity that prevents many OVC support organizations from providing much-needed psychosocial support.
We need to have more professionals. We need to have more child psychologists. We need to have counselors and we need to have more very trained and skillful social workers, psychologists specifically, available in all OVC centers…There is a shortage of professionals in this country and where there are, they are very few and they are also very expensive. So we need to have more.
The combined effect of inadequate financial and professional capacity renders OVC support organizations incapable of addressing one the crucial but often neglected psychosocial needs of
OVCs.
N ETWORKING AND I NFORMATION -S HARING
The lack of networking and information-sharing among OVC support organizations was a major theme that frequently overlapped with the broader theme of organizational capacity. In a country and sector with many financial and personnel constraints, “in order to have effective and efficient utilization of resources,…you need to have a strong network and knowing each other better, performing activities together.” Establishing such a network would allow OVC support organizations to learn from “model OVC centers who have served in this country…for more than thirty years,” while helping to “avoid the duplication…of support and overlaps and not to miss those that are really in need of services.” Moreover, a network foster “a conducive environment…so that everybody knows what is going on with others, and creating a sense of responsibility, a sense of everybody working together, sense of collaboration.”
Though attempts have been made to establish a network of OVC support organizations, “it doesn’t function to its best capacity.” One interviewee offered a cultural explanation for the state of current networking attempts, saying “We are very good culture of eating together, everybody comes together, enjoys the coffee ceremony… When you come to the point where people need to work together, …it is not that much satisfactory.” According to many interviewees, this reluctance to work together often boils down to the competing priorities of the network and the organizations themselves.
18
We usually try to have a good coordination mechanism… without clarifying and making its objective role clear. We may come together and start working on coordination for about 2-3 months, and after then they start questioning, "Oh, a big part of this coordination mechanism is not really rewarding, why should I waste my time?” So they may drop out…and they start doing business as usual… There is also role confusion and it seems that this coordination mechanism is competing for fundraisers. So some of the members may start to sabotage the activities of the coordination body.
Given their aforementioned lack of financial capacity, it is easy to understand why many OVC support organizations would be hesitant to devote their time, energy, and personnel to a network or forum that they may perceive as a source of competition for local and international funding.
Instead of coordinating their efforts, these organizations are more likely to devote their time to performing “their own duties and responsibilities” and “trying to be smart at the expense of the other organizations.”
D ISCUSSION
This research identified the importance of caregiver training; the importance, and lack of, psychosocial support for OVCs; gaps in professional and financial capacity; and the need for increased networking and information-sharing among OVC support organizations as significant factors affecting OVC health and access to support services.
In 2001, the Ethiopian government adopted the WHO Integrated Management of Childhood Illness (IMCI) as their primary strategy for reducing disease and mortality rates among children less than 5 years of age (Federal
Ministry of Health 2001). The IMCI approach aims to improve the case-management skills of health workers, promote appropriate care-seeking behavior among caregivers, and improve preventive practices at the household and community levels (ibid). Several studies, including the
WHO’s Multi-Country Evaluation of IMCI, have shown that this approach can increase health care quality and improve health outcomes for children less than 5 years of age (Arifeen et al.
2009; Armstrong Schellenberg et al. 2004; Bryce et al. 2005). Indeed, a 2002 intervention trial conducted in two Woredas in the Tigray region of Ethiopia found that training communities in
IMCI can result in significantly higher rates of childhood survival at the community level (Ali et al. 2005). However, the study authors warned that “further attention needs to be paid to sensitizing crucial target groups within communities, such as unmarried parents and older fathers in this case, in order to maximize the potential overall benefits of health messages” (ibid).
This lack of attention to target groups was observed in a 2011 literature review of journal publications on IMCI, which found no specific studies on the IMCI strategy with a focus on the caregivers (Paranhos et al. 2011). Though IMCI can improve the knowledge and practices of caregivers (Zaman et al. 2008; Pelto et al. 2004; Santos et al. 2001; Cunha et al. 2005) it can only do so when there is strong, detailed communication between caregivers and health professionals
(Paranhos et al. 2011). The importance of caregiver-health professional communication was emphasized by one interviewee, who said “it’s easy to tell to a nurse [like me] about the disease.
If you say to person who is sick, it's more difficult. And you have to translate into Amharic because when you learn them, diseases are translated into English.” While it is encouraging to see OVC support organizations focusing on training for caregivers, these organizations must also consider the manner in which that information is being communicated. An attitude that is
“communicative and empathetic…contributes significantly to an effective integration between
19
practical and technical-scientific knowledge” and trainings that fail to consider this may have a limited impact as a result (ibid).
The centrality of the caregiver and extended family to the psychosocial well-being of OVCs was cited extensively in this research and in the scientific literature as well (Nyamukapa and Gregson
2005; Nyamukapa et al. 2008). Many interviewees emphasized the importance of maintaining ties between OVCs, the extended family, and community in preserving the psychosocial health and individual identity of the OVC. However, interviewee responses also suggest that sustained
OVC contact with the family and community may be somewhat of a Catch-22, given that the extended family and community are often the main source of OVC physical and psychological abuse. In Ethiopia, it is usually the “close relatives or their neighbors who will declare as if they are the right person to protect the children” when their parents die. Yet, if these new caregivers abuse the child, “no one [in the community] will ask him or her, especially if he or she is her relative, [to stop]. So the perspective of the community itself towards the child is they are taking as a property, not as a human being.” OVC abuse at the hands of caregivers and the community may also take a more subtle form.
[W]hen their [OVCs’] parents are terminally sick and bedridden, then their relatives will not allow them to see their parents when they are sick. Even after their death, children…they are not allowed to go with the other people and bury their parents… [I]f they sometimes cry because of the death of their parents, the community will discourage them not to behave that way. So they have aborted grief.
According to a 2001 study on care arrangements for Ethiopian AIDS orphans, children taken in by extended family members were subject to “extensive” abuse and exploitation, including having inherited property stolen by extended family members under the guise of “kinship,” a practice referenced by one interviewee as causing depression among OVCs (Varnis 2001). The potential for abuse at the hands of the community has also been documented. A 2006 study of
Rwandan OVCs found that 86% of the caregivers felt rejected by the community after being orphaned, while 57% believed the community would rather hurt them than support them
(Thurman et al. 2006). These findings suggest that maintaining contact with extended family and community may, in some cases, adversely affect the psychosocial well-being of OVCs by reminding them of, or forcing them to relive, incidents of past abuse. OVC support organizations must be aware of this adverse effect of sustained familial and community contact to avoid any further physical or psychological damage to OVCs in their care.
The combined effect of physical and emotional abuse of OVCs highlights the importance of addressing their psychosocial needs, or what one interviewee called “the softer side of children.”
Unfortunately, though, “this is an area which is also really neglected by many organizations” in favor of more tangible support like food, clothing, and shelter. The lack of funding for psychosocial interventions in particular and the dearth of trained mental health professionals was a major theme that emerged from this research, and is supported by scientific literature (Kutcher et al. 2005; Patel et al. 2008; Remschmidt and Belfer 2005). Regarding the limited financial capacity of organizations to address the psychosocial needs of OVCs, a 2008 report on the WHO
Atlas Project, which provides information on mental health services around the world, found
“substantial gaps in resources for child mental health” in the 66 countries – including Ethiopia –
20
for which data was available. The report found that there has been “a universal failure to provide the needed financial resources” for child mental health and that “there continues to be a reliance on ‘soft money’…from largely temporary and vulnerable sources [read: international donors] rather than by more stable government allocations” (Belfer 2008). Due to this lack of stable, government funding, out of pocket expenditures for child mental health services in African countries run as high as 71%, versus 12.5% in European countries (WHO 2005). Though many interviewees mentioned limited financial resources in connection with a lack of psychosocial services, one interviewee from a local OVC support organization was particularly fixated on financial constraints more generally. This may be due to the size and youth of his organization, which was founded in 2008, and the fact that “I can't get visa to go to US to do fundraising because I am young, I am single”, a reference to the suspicion with which US embassy employees look upon single, male Ethiopian visa applicants.
In terms of professional capacity, the 2005 WHO Atlas Project report confirmed that child mental health professionals are relatively rare outside of developed countries, with a ratio of 1 to 4 child psychiatrists per one million people in most African countries (WHO 2005). Only South Africa and Tunisia have more than one psychiatrist per 100,000 population, and only Namibia and
South Africa have more than one psychologist per 100,000 population (Robertson et al. 2004).
What is worse, the 2005 Atlas report identified fewer than 10 psychiatrists outside of South
Africa who are trained to work with children (WHO 2005). The results of a recent 2011 study of more than 1,200 orphaned and abandoned children across five low- and middle-income countries confirm that increased levels of funding and support are still needed for OVC psychosocial services, and that “food, water, shelter, educational support, and health care services are necessary, but…not sufficient for the orphan population” (Sanford 2011).
A lack of effective networking mechanisms among OVC support organizations was identified as a significant barrier to OVC service provision and efficient resource utilization. Several interviewees highlighted cases of service redundancy, with individual OVCs receiving support from three or more different organizations at the same time. Stronger networking and information-sharing mechanisms were thus seen as critical to the efficient use of already limited financial and professional resources. Given the failure of previous networking attempts and the tendency for organizations to view such networks as competition (see above), many interviewees proposed a larger role for the government in coordinating the activities and information-sharing among OVC support organizations. As one interviewee suggested, “there should be… [a] controlling or monitoring government body who follow up the OVC centers so that they can take immediate solution from them. A data system should be available at any time.” If the government “was also involved in this activity, the government can send to us, we can exchange information easily.”
These interviewee recommendations are supported by a 2008 study of nine government-NGO collaborations on OVC programs in southern Africa, which found strong evidence of the importance of government partnership for program sustainability and advocating for OVC rights
(Rosenberg et al. 2008). According to one interviewee, though, the government has its own incentive to remain inactive on the issue of networking.
21
[F]or coordination and taking the lead, that is what the government is expected to do.
[But] if you request them to take the lead, they will not be active on that aspect because that is not the issue for them to be evaluated [on]. They will be evaluated on what they deliver on the political line. So that’s another agenda for them.
This relates back to comments made by several interviewees regarding the lack of a strong child policy in Ethiopia. As one interviewee explained, even though Ethiopia is a signatory to the
Convention on the Rights of the Child, “that’s not how it is in Ethiopia. It’s what’s in the best interest of the parents and relatives. So we have to reinforce the rules and regulatory framework… [to] protect these interests of children.” Without a stronger, national-level child policy to which the government can be held accountable, it is unlikely that the government will take an active role in coordinating the efforts of the numerous OVC support organizations working in Ethiopia.
L IMITATIONS
Given the scale of the OVC problem in Ethiopia (UNICEF 2007), understanding the gaps in provision and coordination of OVC support services is critical. However, there are several limitations of this research that should be considered. The goal of this research was not to identify broadly generalizable findings, but to identify gaps in OVC support services that can be used to improve existing programs and inform the development of future programming for
OVCs in Addis Ababa, Ethiopia.
Qualitative research methods and analysis techniques often elicit concerns regarding the validity and reliability of data (Giacomini & Cook 2000; Bergman
& Coxon 2005). The data analysis strategy employed in this research involved a systematic process of code development and modification. Some perspectives were inevitably lost in the data coding, analysis, and reporting process, as certain themes were only mentioned by one interviewee or did not relate to the research question. Although the coding, analysis, and reporting procedures captured the strongest and most prevalent themes, some unique perspectives voiced by a few interviewees were omitted in the process. In addition, the major themes that emerged from this research may not be comprehensive or fully indicative of all OVC support organizations and care providers in Addis Ababa. The sampling procedures employed biased the pool of interviewees toward those working for organizations listed in the directory of the CCRDA and those with a website.
Finally, the influence of the “interviewer effect” on the research findings cannot be overlooked
(O’Muircheartaigh & Campanelli 1998). In semi-structured in-person interviews, the presence and behavior of the researcher inevitably affects participant responses, thereby influencing the ultimate findings of the research (Finlay 2002). As a young, white, female, American public health graduate student, my background and presence may have influenced the content and depth of interviewee responses. This “interviewer effect” could have potentially been mitigated through investigator triangulation utilizing Ethiopian male researchers, but time and limited financial and human resources did not allow for that in this research.
I MPLICATIONS FOR F UTURE I NTERVENTIONS
22
The findings of this research suggest a number of potential interventions for Betasab to pursue.
Both the qualitative and quantitative analysis confirm a lack of caregiver knowledge pertaining to child health and appropriate health-seeking behaviors. To increase child health-related knowledge among caregivers, Betasab should partner with local clinics to provide easily accessible and comprehensible trainings that will bridge the communication gap between caregivers and clinicians. These trainings should go beyond the usual topics of hygiene and symptom recognition to address the psychosocial needs of OVCs. International and domestic volunteers and/or staff members with backgrounds in mental health and social work should be recruited to develop trainings and best practices related to the psychosocial care of OVCs.
Improving the quality of caregiver training will simultaneously address the issue of limited financial capacity faced by many OVC support organizations. The more high quality child health training provided to caregivers:
The more we build the capacity of the guardian, the more they can do…[The] focus should be on strengthening the capabilities of families’ resilience…rather than implementing resource-intensive approaches for a limited number of beneficiary
[children].
( Abebe and Aase 2007)
Building the capacity of the caregivers builds the capacity of the OVC support organization.
Targeting the problem at its source – the caregivers – will allow organizations such as Betasab to create a sustainable solution that will help them conserve financial and human resources further down the line.
Based on the results of the quantitative survey, the emphasis of Betasab’s child sponsorship and community development programs should be on Woreda 2 of Lafto sub-city. According to the survey, a higher percentage of Woreda 2 households care for orphans, care for children living with only one biological parent, and are more dependent on donations, NGO support, and begging for their household income. Possible interventions for Betasab to pursue include:
Increasing household access to piped water – to reduce risk of children contracting diarrheal diseases, which are one of the leading causes of childhood morbidity and mortality in Ethiopia
Income generating activities for caregivers – to increase the capacity of Woreda 2 caregivers – 60% of whom have had no formal education – to pay for food, child health services
Material support for children – to ensure that children have basic items such as clothes, shoes, and bedding
Supplementary food program – to ensure that children are receiving adequate nutrition to support their mental and physical development
Help (financial, other) accessing child health services and immunizations – to ensure that children have access to medical services to support their growth and development
23
However, given that many Woreda 2 households already receive support from other NGOs,
Betasab should work collaboratively with other organizations to avoid service overlap and redundancy.
Finally, Betasab should partner with other OVC support organizations to advocate for stronger policies and greater accountability when it comes to the rights and protection of OVCs. As one interviewee noted:
Can you imagine, can you believe, in a country like Ethiopia – 80 million population, especially – about close to half of the population is child population. But we have
Ministry of Women , Youth, and Children’s Affairs. Why don’t we have – if half of the population is child population - …a ministry for children. It has been taken as a sideline activity…
Advocating for the establishment of child-friendly courts, a stronger regulatory framework, and adherence to the principles of the Convention on the Rights of the Child will increase government accountability for the physical and mental well-being of OVCs, thereby creating a more conducive and collaborative environment for OVC service provision.
R
EFERENCES
24
Abebe T. and A. Aase. (2007). Children, AIDS and the politics of orphan care in Ethiopia: The extended family revisited. Social Science & Medicine 64(10): 2058–2069.
Agnihotri K. et al. (2010). A study of concordance between adolescent self-report and parentproxy report of health-related quality of life in school-going adolescents. J Psychosom Res 69:
525–532.
Ali, M. et al. (2005). Helping northern Ethiopian communities reduce childhood mortality:
Population-based intervention trial. Bull World Health Organ 83(1).
Andrews, G. et al. (2005). Epidemiology of health and vulnerability among children orphaned and made vulnerable by HIV/AIDS in sub-Saharan Africa. AIDS Care 18(3): 269-276.
Arifeen, S.E. et al. (2009). Effect of the Integrated Management of Childhood Illness strategy on childhood mortality and nutrition in a rural area in Bangladesh: a cluster randomised trial. Lancet
374(9687): 393-403.
Armstrong Schellenberg J.R.M. et al. (2004). Effectiveness and cost of facility-based Integrated
Management of Child Illness (IMCI) in Tanzania. Lancet 364: 1583-94.
Belfer M.L. (2008). Child and adolescent mental disorders: the magnitude of the problem across the globe. Journal of Child Psychology and Psychiatry 49(3): 226-236.
Bergman, M.M. and A. Coxon. (2005). The Quality in Qualitative Methods. Qualitative Social
Research 6(2), Art. 34.
Bryce, J. et al. (2005). Programmatic pathways to child survival: results of a multi-country evaluation of Integrated Management of Childhood Illness. Health Policy Plan 20: Suppl 1 i5– i17.
Coyne, I.T. (1997). Sampling in qualitative research. Purposeful and theoretical sampling: merging or clear boundaries? Journal of Advanced Nursing 26: 623-630.
CSA (2007). Summary and Statistical Report of the 2007 Population and Housing Census.
UNFPA. Addis Ababa. Online at: http://www.csa.gov.et/pdf/Cen2007_firstdraft.pdf
CSA – Central Statistical Agency (Ethiopia) - and ICF International (2012). Ethiopia
Demographic and Health Survey 2011. Addis Ababa, Ethiopia and Calverton, Maryland: CSA and ICF International.
Cunha A.J.L.A. et al. (2005). Integrated care of childhood disease in Brazil: Mothers' response to the recommendations of health workers. Acta Paediatr 94(8):1116-21.
25
Federal Ministry of Health (2001). Implementation strategy for the household and community components of IMCI in Ethiopia.
Ministry of Health: Addis Ababa, Ethiopia.
Giacomini, M.K. and D.J. Cook. (2000). Users’ Guides to the Medical Literature: XXIII.
Qualitative Research in Health Care—Are the results of the study valid? Journal of the American
Medical Association 284(3): 357-362.
Government of Ethiopia (2007). Report on Progress in Implementing the World Fit for Children
Plan of Action in Ethiopia. Online at: http://www.unicef.org/worldfitforchildren/files/Ethiopia_WFFC5_Report.pdf
Hsiu-Fang, H. and S.E. Shannon. (2005). Three Approaches to Qualitative Content Analysis.
Qualitative Health Research.
15 (9): 1277-1288.
Jabson, J. (2011). Content Analysis: Steps in Analyzing Qualitative Interviews. SB818. Boston
University School of Public Health.
Kutcher S. et al. (2005). A competencies-based mental health training model for health professionals in low and middle income countries. World Psychiatry 4(3): 177-180.
Nyamukapa, C. and S. Gregson. (2005). Extended family's and women's roles in safeguarding orphans' education in AIDS-afflicted rural Zimbabwe. Social Science and Medicine 60(10):
2155-2167.
Nyamukapa C.A. et al. (2008). HIV-Associated Orphanhood and Children’s Psychosocial
Distress: Theoretical Framework Tested With Data From Zimbabwe. American Journal of
Public Health 98(1): 133-141.
O’Muircheartaigh, C. and P. Campanelli. (1998). The relative impact of interviewer effects and sample design effects on survey precision. Journal of the Royal Statistical Society 161(1): 63-77.
Paranhos, V.D. et al. (2011). Integrated management of childhood illness with the focus on caregivers: An integrative literature review. Rev. Latino-Am. Enfermagem 19(1).
Patel V. et al. (2008). Promoting child and adolescent mental health in low and middle income countries. Journal of Child Psychology and Psychiatry 49(3): 313-334.
Patton, M. (2002). Qualitative Research & Evaluation Methods . 3 ed. Sage Publications:
Thousand Oaks, CA.
Pelto G.H. et al. (2004). Nutrition counseling training changes physician behavior and improves caregiver knowledge acquisition. J Nutr 134(2):357-62.
Remschmidt H. and M. Belfer. (2005). Mental health care for children and adolescents worldwide: a review. World Psychiatry 4(3): 147-153.
Robertson B.A. et al. (2004). Systems of care in Africa. In: Remschmidt H, Belfer ML, Goodyer
26
I, eds. Berlin, Springer: 70-88.
Rosenberg A. et al. (2008). Government-NGO collaboration and sustainability of orphans and vulnerable children projects in southern Africa. Eval Program Plann 31(1): 51-60.
Sanford School of Public Policy. “Protective and Mental Health Services Critical for Orphans
Worldwide.” 25 March 2011. Accessed 20 June 2012. Online at: http://news.sanford.duke.edu/news-type/news/2011/protective-and-mental-health-servicescritical-orphans-worldwide
Santos I. et al. (2001). Nutrition counseling increases weight gain among Brazilian children. J
Nutr 131(11):2866-73.
Theunissen N.C. et al. (1998). The proxy problem: child report versus parent report in healthrelated quality of life research. Qual Life Res 7: 387–397.
Thurman, T.R. et al. (2006). Psychosocial support and marginalization of youth-headed households in Rwanda. AIDS Care 18(3).
UNICEF (2007). Ethiopia: Country Programme Document 2007-2011. Online at: http://www.unicef.org/about/execboard/files/Ethiopia_final_approved_CPD_19_Jan2007.pdf
UNHABITAT (2007). Situation Analysis of Informal Settlements in Addis Ababa. UNHABITAT.
Nairobi.
Varnis, S.L. (2001). Promoting child protection through community resources: Care arrangements for Ethiopian AIDS orphans. Northeast African Studies 8(1), 143–158.
Zaman S. et al. (2008). Training in complementary feeding counseling of healthcare workers and its influence on maternal behaviours and child growth: a cluster randomized controlled trial in
Lahore, Pakistan. J Health Popul Nutr 26(2):210-22.
WHO. (2005). Atlas: Child and adolescent mental health resources: Global concerns, implications for the future. WHO Press: Geneva. Online at: http://www.who.int/mental_health/resources/Child_ado_atlas.pdf
WHO/UNICEF. (2010). “Types of drinking water sources and sanitation.” WHO/UNICEF Joint
Monitoring Programme (JMP) for Water Supply and Sanitation. Accessed 18 August 2012.
Online at: http://www.wssinfo.org/definitions-methods/watsan-categories/
27