Scottish Prison Service rep - Health Protection Scotland
advertisement

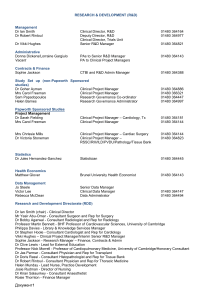
Hepatitis C Needs Assessment Findings from focus groups Methods • Views of service providers sought using focus groups and one-to-one interviews • Participants asked to consider the patient journey from testing to treatment and to discuss: – Needs of their clients – Barriers to progression along patient pathway – Solutions to overcoming the barriers Recruitment • 9 key informant groups identified • 43 service providers identified and invited to participate • 29 (67%) of those invited took part in the study (25 in focus groups, 4 in individual interviews) • 8 health board areas represented by those providing local services Data collection and analysis • 5 focus groups and 4 interviews conducted over two week period • Focus groups multidisciplinary • Focus groups lasted 90 – 120 mins • Sessions recorded and transcribed • Transcriptions and tapes analysed for recurring themes Composition of focus groups &interviews Participants in each focus group / interview Informant group Focus Group 1 Addictions / Harm Reduction 1 Focus Group 2 1 1 1 GP Lab Services 1 Tel 2 Tel 3 Face to face 2 1 2 1 1 1 4 5 1 4 2 1 1 4 1 2 Scottish Prison Service Social Care 1 Total 1 1 3 Tel 1 2 1 Voluntary Sector Focus Group 5 2 Public Health / MCN Total Focus Group 4 1 Clinical Nurse Specialist Consultant Physician Focus Group 3 4 1 3 2 1 7 5 3 1 6 1 1 1 1 29 Findings • • • • Identified many barriers to retention and progression of clients along care pathway Recommendations made as to how these might be overcome Participants found process of focus groups useful Findings can be categorised into 7 main areas: 1. 2. 3. 4. 5. 6. 7. Testing and diagnosis Knowledge of HCV Partnership working Specialist services Support services Prison services Resources Testing & Diagnosis: Barriers • Need for venepuncture – Poor venous access – Lack of trained staff • The testing site – Limited access – Not appropriate for client • Lab delays – Up to 4 weeks – Difficulties getting result back to client • “..one of the worries we all have is the patient not getting the result, because we all know that this isn’t a group of patients who hang around the system for too long. In hospital services, maybe if they are in-patients they will be out-patients by the time the results come back and then they don’t come back to the clinic” Consultant physician • “It’s not acceptable to the patient waiting for four weeks to get an answer. I can tell you from that point of view, definitely it’s not!” Voluntary sector rep Testing & Diagnosis: Barriers • Hard to reach populations – New / Chaotic drug users – Ex drug users – Never drug users • Stigma – Similar to HIV • Perceived need for specialist counselling “..we need to break down this stigmatising view of HIV and I think that we need to try and bring that to bear on hep C as well, because there are very many similarities about it: it’s stigmatising, it says something about someone’s lifestyle etc etc. But we don’t want to have the barriers to testing that were previously associated with HIV and that we’re now trying to break down.” Consultant physician “I think they [health professionals] do get hung up on the counselling side of things. It is important to get the relevant information across, but sometimes it does frighten practitioners away from wanting to test, you know, because they don’t feel they have the skills.” Scottish Prison Service rep Testing & Diagnosis: Solutions • Increase access – Provide more and varied test sites – Train more staff in venepuncture – Introduce oral fluid testing • Normalise testing – Bring into the mainstream – Become part of standard GP or nurse consultation – Move away from concept of pre-test counselling towards pre-test discussion Testing & Diagnosis: Solutions • Primary care key role – Opportunistic testing – GP may be only contact with health services • Target hard to reach populations – Outreach testing – Use GP and addiction services’ patient records • Reduce laboratory delays – Good computer links – Local PCR testing Knowledge of HCV • Lack of knowledge (clients and services) – Acts as barrier at all stages of pathway – About the disease, the risks, the test and the treatments available • Misinformation (clients and services) – What hep C diagnosis means – Who will get treatment • “I don’t think that there is a general awareness that there are effective treatments around. I think that people would be more motivated to come forward for testing if they thought there was some possibility of a cure.” Social care rep • “..an important barrier to testing is, whether it’s GPs or whoever else that is considering testing an individual, that they fail to offer them a test or they discourage them from being tested because their perception is it’s not in their best interests to know their hep C status…..if it is positive you’re better off not knowing…you’re not going to get treatment because of your lifestyle.” Consultant physician Knowledge: Areas to address • Improve health professionals understanding of: – Who to test – How to interpret results – When to refer to specialist services – The role of addictions, social care services, and the voluntary services Knowledge: Areas to address • Increase awareness about risk factors “..there are several thousand individuals in Scotland with undiagnosed hep C who have never had a history of drug injecting or sexual contact with drug injectors, who would never, ever consider themselves to be at risk of hepatitis C. And I think that’s a particularly difficult to reach group when it comes to testing.” Consultant physician Knowledge: Areas to address • Improve clients’ understanding of HCV – Not a death sentence – Effective treatments available – Ongoing drug / alcohol use not absolute contraindication to treatment “..we certainly see a lot of people who come and they say ‘I know I’ve got hep C’. They’ve never been tested, they’ve just got this fatalistic attitude, so they don’t come forward for the test. It seems sensible, if you’ve got a group of people who believe they are infected with a virus and a lot of them think it carries a death sentence, if you tell them ‘you’re not infected with it, and here are ways of preventing it’ then they might take that on board. And whenever people are discussing the treatment, then they should be emphasising that there is a way out of this and the diagnosis of hep C is not a terminal diagnosis” Consultant physician Partnership working • Crucial at every stage of pathway • Services often work in isolation – Duplication of effort – Clients fall out of care pathway • Need improved communication and clear referral routes between services Specialist services: Barriers to attending • Up to 50% clients fail to attend first appointment, others drop out later • Barriers to attending – Chaotic lifestyles / competing priorities – Referral and appointment systems – Lack of incentive to attend • “I think [to keep clients in the system until treatment] there is something about trying to meet as many as possible of the diverse needs that the individual has got in the one place. The more needs people are getting met, the more incentive they’re going to feel to come along there. Whereas if people are feeling, well they’re just getting their blood monitored and it’s more or less the same every time they may not feel that motivated to appear.” Social care rep Specialist services: Barriers to attending • Access problems “..I mean this really is a disease of poverty, everything is geared around having a car, and a lot of them don’t have a car. And the problem with transport in someplace like [name of health board], to come to our unit by bus - you could easily spend two hours doing that.” Consultant physician • Prisoner transport arrangements limit number who can attend at any one time Specialist services: Solutions • Good links into drug, alcohol & social care services • Increase accessibility – Patient transport service – Satellite clinics e.g. GP surgeries and prisons • More flexible approach to referrals and appointments – Multiple inward referral routes – Telephone / text-based appointment systems Specialist service: Solutions • Specialist nurse outreach services – Already introduced / being piloted – Lots of support for this model of care – Allows client and nurse to build up relationship / trust – Can monitor in community until ready to see consultant – Facilitates relationship between specialist services and other agencies • “…they [the clients] can’t get themselves together to come to a clinic at a certain time and a certain place. And we have them turning up a week later or a week beforehand; wrong clinic, wrong hospital. So they’ve attempted to come along but not made it, but the system then kicks them out because we’re not allowed to have such flexibility in the service. So I think that has been helped by the outreach service, and trying to get people up to speed before they even come along to the clinics.” Consultant physician Specialist services: Barriers to treatment • Starting treatment: – Chaotic lifestyles – Fear of side-effects – Access to pre-treatment psychiatric assessment • Completing treatment – Drop-out rate historically low, but likely to increase – Principal reason, at present, is side-effects “It’s certainly been my experience so far, that by the time someone gets to start on treatment, their level of commitment – to see that treatment succeed – is enormous. Now, it may be that patient selection plays a huge part in that” Consultant physician “we are now treating a lot more difficult to engage people than before and the numbers the nurses can actually run through the system has reduced. They’re becoming more and more time consuming because they do have social issues, they do have other dependency issues. Whereas previously we had a 98% attendance rate that has gone way down as we’ve expanded the criteria for people to come into treatment.” Consultant physician Specialist services: solutions • Peer support / buddy systems “What the patient really benefits from is having a sort of buddy system. Someone outwith the medical or nursing profession who they can rely on to turn to and be there during the day or during the night or the weekends. And we’ve found people who have got a good social network, or who’ve got some buddy identified, they do a lot better through treatment.” Consultant physician Specialist services: solutions • Improve access to pre-treatment psychiatric assessment • Improve access to other specialists during treatment to manage side-effects “[Hepatitis C] impinges on so many specialities that you can’t have everybody at your clinic – you can’t have an ophthalmologist for the once a year you’re going to use them. But perhaps there should be some fast track ways in and if, as a group, we could make some recommendations out to those groups – that might be beneficial.” Consultant physician Support services • Many clients chaotic lifestyles – Major barrier to entering and remaining on pathway • Require significant social support – Provide from early stage – Social work input important • Currently limited • Support for development of dedicated services – Voluntary agencies • Major role in supporting patients • Peer support and information outside clinical setting • Limited provision outside major cities • “But we also know that their treatment depends on getting their physical environment much improved. It depends on getting re-housed, it depends on getting help and support services and a whole bunch of stuff – if they’ve not got that they are not going to comply with treatment.” Addiction services rep • “I mean, if we could have that [social work input to specialist clinics] it would be excellent to actually be able to follow these things up. Cos if we have a problem, we have to go all round the houses and by that stage the person’s pissed off and they’ve decided they’re not having any more of this and they’re out the door.” Consultant physician Prison services: Barriers • Short sentences / remand prisoners – Released before result available or patient seen be a specialist – Difficult to follow-up • Move to another area • No GP – Some prisons wont test if < 6 months to serve • “What we have got to do better is get people established who stay a shorter and shorter time. At the moment we are only really trying to cut into the burden of care for people who stay long enough to stabilise, get the offer, get tested, onto specialist services, get established – that takes a long time. We are shrinking the time, but I think we’ve got to shrink the time now to testing and give them some assurance that when they go out after a short time they will get seen and attended to.” Scottish Prison Service rep Prison services: Barriers • Movement of inmates – Transfer between prisons common – often related to security / overcrowding – Health not seen as priority – Across health board boundaries / at short notice • “Our difficulty is that we will get patients worked up from the prisons and then we find out, either the day we start their treatment, or within two or three weeks of starting up, they’re moved somewhere else. And so mobility of patients within the prison service is a major issue for us. They are totally disadvantaged by the rapid movement circling around the prison system.” Consultant physician • “Sometimes it can just go totally pear-shaped. And even with the best will and the best planning in the world, things change, and they can change so quickly, and people move for security reasons.” Scottish Prison Service rep Prison services • Solutions – Better links / improved communication between short stay prisons and primary / secondary care – Place short-stay prisoners in their own community – Better communication between prisons themselves – Undertaking from prisons not to move patients on treatment / give adequate notice • Progress being made – Health higher up prison service agenda – Introduction of IT system across prisons “We are in the early days, but health is more and more on the map in terms of prisons and, hopefully, more and more a feature or a factor in the decision to move people around the estate. The other thing we are trying to do for people staying less long with us is locate them in their community prison. But overcrowding, it’s one of the worst effects, overcrowding, in terms of the health care of the people. You cannot say to the prison service to keep them there because ‘I’ve got a very good reason’ – because they have a much better reason: that person needs a bed tonight and if it’s not this, it’s a mattress in the gym. They’ve go to do their job, and we’ve got to influence their decisions, especially when they matter.” Scottish Prison Service rep Resource • Need to match resource with any plans to increase testing – Specialist services already at capacity – Patients with more complex health and social care needs entering care pathway – Voluntary agencies already limited capacity to support those known to have hepatitis C – Further development of dedicated HCV social work / prison services will require adequate funding