Slides: Introduction to Spirituality in Health Care & Medicine
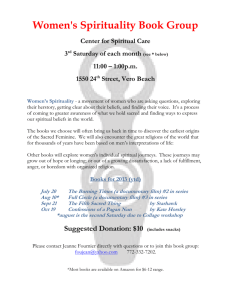
advertisement
SPIRITUALITY IN MEDICINE AND HEALTH CARE Thomas R. McCormick, D.Min. Department of Medical History and Ethics U.W. School of Medicine Health Care in Early Times Medicine & Religion • Few interventions were possible • Application of herbal medicines • Religious concepts of cause and effect included : – punishment for sins – indwelling of evil spirits – separation of the patient from God Ancient medicine & religion • 3000 BCE, early written documents show Egyptian & Mesopotamian healers were priests with magico-religious concepts. • 5th century BCE in Greek medicine, Hippocrates begins a more scientific approach, including natural causes. • By the 3rd century BCE, the Romans were influenced by the Greek’s cult of Asclepius. Greece: The Temple of Asclepius Two views of health care HYGEIA & ASCLEPIUS • HYGEIA: health is the natural order of things, fostered by prudent choices and wise living, the goal is to find balance between a sound body, a sane mind, and a calm spirit-medicine should discover & teach the natural laws, so we might cooperate. • ASCLEPIUS: the chief role of medicine is to treat disease, the heroic intervenor. Nursing care and natural healing processes grow from the approach of Hygeia Interventive medicine has its roots in Aescleplius Theoretical Models Emerge • Biomedical model in the 19th century • Psychobiological model--after Freud – emotional states contribute to illness – relaxation response may reverse illness • 20th century: bio-psycho-social model – 1977, George Engel – Life events & lifestyles affect health Medicine in the Christian era • Healings were attributed to Jesus, who sometimes linked healing with the power to forgive sins. • The Parable of the Good Samaritan became a formative influence on medicine. • By the 5th century AD, virtually all physicians were drawn from clergy in the monastic communities. (Kuhn, Psychiatric Medicine Vol. 6 No. 2) Secular Medicine • Secular medicine emerged in the late middle ages, but was still under control of church. • 1140 AD church granted first medical licenses, conditions, & revocations. • 1789, the French Revolution, marked the break down of religious control over medicine. • Cartesian: separation of mind and body Separation of Medicine from Religion • As science began to discover the etiology of diseases, former religious explanations no longer held. • Science and medicine began to distance themselves from religion. • “God of the gaps. . .” A Current view of health care: A BIO-PSHYO-SOC-SPIRITUAL MODEL • • • • Scientific view of pathophysiology Respect for the psychological Perception of the social environment Attention to the spiritual distress and the spiritual resources of the patient • Described by Division of Behavioral Medicine at the University of Louisville School of Medicine The Spiritual • The patient is not just body and mind, but a spiritual being. --P. Tournier • Spirituality involves the personal quest for meaning & purpose in life and relates to the inner essence of the self • Spirituality: the sense of harmonious interconnectedness with self, others, nature and an Ultimate Other (the integrating factor) Bio-Psycho-Social-Spiritual • Although Schools of Medicine have been slower to recognize & appropriate this model, • The Nursing Profession has long recognized the spiritual aspects of patient care, • Chaplains and clergy have often assisted patients with the spiritual aspects of illness and the search for meaning & purpose. Religion is seen by some to be an impediment to medicine • Jehovah’s Witness who refuses a life saving blood transfusion; • Christian Scientist who refuses allopathic health care in favor of a Reader; • Various religions that may decry contraception or forbid pregnancy termination. Great Diversity of Religions • Especially in the USA, there is a great number of religions so that one can hardly speak of religion in general, without making reference to a particular religion. • It is too much to expect of a physician that s/he be a student of religions, in addition to medicine. • And, what if the physician is non-religious? Question: Should physicians avoid talking about religion or spirituality with patients? • A. yes, because a physician can not be expected to be conversant with all religions. • B. yes,because the physician may be an atheist or non-believer. • C. yes, that would be an unethical intrusion into the privacy of the patient. • D. no, particularly when there are indications of patient interest or need. Distinction: Between Religion and Spirituality • Answer: D; no, there are indications. . . • A particular religion or faith community is one road to spiritual awareness and growth. • Spirituality in this sense, may transcend a particular religion, and resides in that universal human space where individuals seek to understand the meaning & purpose of their lives, and what they most value. • Spirituality implies self-conscious living. Spirituality • Thousands of alcoholic patients who found little help from traditional medicine were able to become sober and remain abstinent by relying on “a power greater than themselves” and through the support of a twelve step program. A Shift of focus: from the biomedical to the psycho-social-spiritual • For many patients facing serious illness or the end of life, the focus shifts from the biomedical to the spiritual. • When symptom management and pain control are appropriately provided, patients are set free to address their “final agenda.” • This may be seen as the last chapter in one’s spiritual journey. (Mary Levine) R.M. Mack, MD “Occasional notes: Lessons learned from living with cancer.” NEJM 311:1642, 1984 • “Simply accepting this prognosis was completely intolerable for me. I felt I was not yet ready to be finished. I still had not seen and done and shared with the people I love. . . I could sit back and let my disease and my treatment take their course, or I could pause and look at my life and ask, What are my priorities? Dr. Mack, a Seattle surgeon’s reflections. . . • How do I want to spend the time that is left? I began to focus on choosing to do things every day that promote laughter, joy, and satisfaction. . . I began to make choices to do the things that felt good to me.” • One person, opening to the meaning of life in the face of imminent death. . . What do patients nearing the end of life say? • • • • • fear of uncontrolled pain & neg. symptoms worry about becoming a burden on family concern about financial costs of care uncertainty about the dying process anxious anticipation of surrendering the known for the unknown • Concern for the “unfinished business of life” Patients raise spiritual questions • Who am I, now that I am sick or dying? • What is the meaning of my life when I am no longer productive and independent? • Where am I connected to others who value me and see me as a person of worth? • What is my relationship to the Ultimate? • What do I now value most in the time that is left to me? Epictetus: a question of meaning • “It is not as important what happens to a person, as to the meaning that the person gives to what has happened.” • Assignment of meaning is a spiritual function. Lipowski: how we view illness • • • • • • • Illness a challenge Illness as enemy Illness as punishment Illness as weakness Illness as relief Illness as strategy Illness as having value Meaning is related to purpose, therefore questions might be: • Why do you think you have become ill now • Has this illness changed any attitudes you might have about the future? • Is there anything more important to you than regaining your health? • How does this illness interfere with your goals in life? • What purpose is served in regaining health? Where does spirituality fit? • Patients may have coping mechanisms related to their belief • May be supported by a community of caring others. • May feel themselves to be in the company of the Divine. Man’s Search for Meaning Victor Frankl • Sometimes external circumstances in our life situation are beyond our control. • Frankl maintains that the attitude we choose to take toward our life situation is within our control. • The spiritual journey relates to our inner struggle to shape our attitude toward illness and even death itself. Frankl: the will to meaning. . . • Aesthetic: one may find meaning in the beauty of the sunrise, the sunset, the symphony. . . • Relational: one may find meaning in relationships, be they family or friends • Creative: one may find meaning in creative activity, work, profession, homemaking • Attitudinal: one may find meaning in shaping the attitude taken toward illness or death. A Spiritual Inventory might include questions about: • • • • • • • • patient’s perception of what is going on what gives meaning and purpose to life how, or whether belief and faith enter in love: by whom do you feel loved-accepted? forgiveness--need it? grant it to others? prayer--for what do you pray? quiet and meditation--what is off center? worship--what restores you to center? Taking a spiritual history. . . • • • • • • S Spiritual Belief System P Personal Spirituality I Integration in a Spiritual Community R Ritualized Practices and Restrictions I Implications for Health Care T Terminal Events Planning (advance directives, DNR wishes, DPOA etc..) S Spiritual Belief System • How would you describe your spiritual belief system? • Do you find comfort in this current illness from your beliefs and practices? • What in particular is helpful to you? – Internal: private belief system – External: participant in a community P Personal Spirituality • What are your most important personal beliefs? • The professional need not believe what the patient believes, but must acknowledge that the patient’s beliefs are important. • An individual may have a profound spirituality, but may not be overtly religious. I Integration in a Spiritual Community • National Institute for Healthcare Research report studies claiming: • regular church attenders live longer. • risk of diastolic hypertension ranked 40% lower among people who actively participate in spiritual practices. • 93% female cancer patients said their beliefs helped them sustain hope. R Ritualized Practices and Restrictions • Patients may especially value the rituals of their faith community: • Baptism for a critically ill newborn • Anointing (last rites) of a dying person • Scripture • Prayer • Communion, or Eucharist Service I Implications for Health Care • What does the patient understand about his/her medical condition & prognosis? • What are the patient’s beliefs about suffering, about pain control? • Does the patient understand the principle of double effect? • What are the patient’s goals in the time that is left? T Terminal Events Planning • • • • Does the patient have an advance directive? Attorney in fact: Durable Power of Atty.? Curative - Palliative -Comfort Care? How does the patient view dying? – Is it the final end? – Is it the beginning of life eternal? – What is the patient’s final agenda? Mentoring, and teaching by example, is perhaps the most effective approach. UWSOM is featured for teaching end of life care to medical students Students in preceptorships or RUOP’s in the pre-clinical years, or in the clerkships, may gain a deeper appreciation of the spiritual needs and resources of patients. Hospice Student Different cultures may have ceremonies and rituals of special importance in coping with illness or preparing for death.(Navaho) Choice in Dying Study • Education in spirituality should be interdisciplinary (med/nrsng/pastoral), expose students to dying patients, and to caregiver mentors who model ideal knowledge, skills and attitudes. • Preclinical years: patient interview, hospice elective, preceptorships • Clinical years: Clerkships, Hospice rotation, Simulated Patient Interviews, Patient care. Persons with major illness or debilitating disease find strength and support from religious or spiritual sources. • Measures of religious coping can predict outcomes of life crises, vs. non-religious. • Use of religious coping skills by older patients is associated with diminished risk of depression, or of recovery from depr. • Spiritual intervention needs a (CPT) code. Recent surveys by NIHR find: • 43% of physicians pray for their patients, • 90% of doctors at the American Academy of Family Physicians 1996 meeting agreed that “a patient’s spiritual beliefs can be helpful in his or her medical treatment” • 58% have actively pursued information on spirituality and healing. 5 requirements for physicians to meet the spiritual needs of patient • • • • • Be trustworthy, treat the patient as a person, be kind, maintain hope, assist the patient in determining what it means to live. Foster,DW in Religion and Medicine: the physician’s perspective. Fortress Press, 1982 American Psychiatric Association • Physicians should maintain respect for their patient’s beliefs. It is useful for physicians to obtain information on the religious or ideologic orientation and beliefs of their patients. . . • Physicians should not impose their own religious, anti-religious, or ideologic systems of belief on their patients. . . Spirituality in Medicine (1 credit) UW School of Medicine • A multidisciplinary med school elective • Provides a framework for students to communicate with patients about the patient’s spiritual connections • Allows each student to make visitations with a hospital chaplain--seeing patients with serious illness or life threatening illness Goals of this Course: • Heighten awareness and enhance the role of spirituality in our own lives; • Foster respect and appreciation for the diversity of patient beliefs and values; • Strengthen commitment to relationshipcentered approach to health care; • Develop a better understanding of the role of the hospital chaplain and clergy as partners in caring for patients. Spirituality Education at the UW • Year 1: ICM, Human Behavior • Year 2: ICM II, “Terminal Illness Seminar” • Electives: – – – – – SPIRITUALITY IN HEALTH CARE HOSPICE ELECTIVE ETHICAL ISSUES SURROUNDING DYING PRECEPTORSHIPS & RUOP INDEPENDENT RESEARCH PROJECTS Contact Information • Dr. Thomas R. McCormick • email: mccormic@u.washington.edu • http://eduserv.hscer.washingnton.edu/bioethics/ • • • • Box 357120 School of Medicine University of Washington Seattle, WA 98195 Case examples of spiritual issues: • • • • • a disturbing visit from the daughter the professor’s inoperable cancer medical student with an astrocytoma what will my dying be like? a patient’s lament, “please help my parents”