Nursing Assessment & Diagnosis: Chapter 13 Summary
advertisement

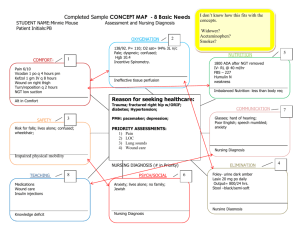
Potter & Perry: Chapter 13 (159-176): Nursing Assessment and Diagnosis (dirk) The nursing process is a problem-solving approach to identifying, diagnosing, and treating the health issues of clients. Figure 13-1: Five step nursing process; circular process, after 5 repeat to 1 1. Assess: Gather information about client’s condition (Ms Devine, 52 year old woman fell 2 months ago and ruptured a lumbar disc, she is scheduled for a laminectomy this afternoon; has limited mobility and acute back pain) 2. Diagnose: identify the client’s problem (acute pain related to pressure on spinal nerves) 3. Plan: set goals of care desired outcomes and identify appropriate nursing actions (to relieve discomfort nurse will order analgesic, repositions and if that offers no solace discuss how Ms Devine can practice relaxation exercises) 4. Implement: Perform the nursing actions identified in planning (administer drugs) 5. Evaluate: determine if goals met and outcomes achieved (check 40 min later to see if analgesic relieving pain, and offer to try relaxation exercises) The nursing process is a variation of scientific reasoning because you organize, systematize and draw inferences. Critical Thinking Approach to Assessment Assessment: gather info about client’s condition (two steps) 1. Collection and verification of data from primary source (client) and secondary sources (family, health professionals, patient record) 2. The analysis of data as a basis for developing nursing diagnoses, identifying collaborative problems, and developing a plan of individualized care Purpose of assessment: to create a database for what is believed the client needs, their health problems, and responses to these problems. What you do during an assessment: -See client’s that present an initial health problem to you -you observe client’s behaviour -ask questions about the nature of the problem -listen to cues the client provides, conduct a physical examination -interview family members who are familiar with the client’s health problem -review existing medical data Figure 13-2 Critical thinking and the assessment process During the Assessment of the nursing process, a nurse synthesizes data from 4 areas: 1. Knowledge: -underlying disease process -normal growth and development 1 -normal physiology and psychology -normal assessment findings -health promotion -assessment skills -communication skills 2. Standards: -CNA -Specialty standards of practice -Intellectual Standards of measurement 3. Qualities: -Perseverance -Fairness -Integrity -Confidence -Creativity 4. Experience -Previous client care experience -Validation of assessment findings -Observation of assessment techniques Experience is the most important because of similarities between past and future clients (back pain normally disabling and limits motion for all); also allows you to see other professionals at work, also allows you to realize what counts as normal standards of practice Data Collection Box 13-1: Guidelines for Documenting a Comprehensive Nursing History (note: don’t get bogged down on the examples, focus on the headings) When a client comes in, acquire as full a health history as possible along such criteria as: A. Identifying Data: Name, age, sex, date, and place of birth B. Reason for health History interview: Explain why you are interviewing the client at the present time (e.g., the client has just been admitted to an inpatient unit or clinic C. Current State of Health: General state of health and health goals (i.e. if illness present collect data about illness through a system analysis) D. Developmental Variables: -Marital Status: single married, separated, widowed, divorced -Number of Children -Development stage -Current job 2 -Significant life experiences (education, previous jobs, financial situation, retirement, coping or stress tolerance, and measures normally used to reduce stress) -Safety hazards (biological, chem., ergonomic, physical, psychosocial, reproductive) -Housing, environmental hazards (type of housing, location, living arrangements; specific hazards in home or community -Safety measures (seatbelts, fire extinguishers, and such in work, community or home) E. Psychological Variables: Mental processes, relationships, support systems, statements regarding client’s feelings about self F. Spiritual Variables: Rituals, religious practices, life beliefs G. Sociocultural Variables: -Culture: beliefs and practices related to health -Primary language and languages spoken -Recreation -Family: composition, interaction, support? H. Physiological Variables (Body Structure and Function) -History of past illnesses and Injuries, including dates -Current medications: legal, non legal, prescribed, effects, side effects, adverse rxns, attempts to quit -Review of systems (body systems), continuation of H: -General manifestations of symptoms: fevers chills, malaise, pain, sleep patterns, fatigue, weight -Integumentary: itching, colour or texture changes, lesions, dryness, hair texture and changes; any lotions or creams used -Ocular: visual acuity, blurring, eye pain, change in vision, discharge, excessive tearing, dryness, date of last exam -Auditory: hearing loss, pain, discharge, dizziness, ringing, wax -Upper respiratory: nosebleeds, nasal discharge, nasal allergies, sinus problems, colds, sore throat, hoarseness, voice changes -Lower respiratory: tobacco use, exposure to airborne pollutants, tuberculosis, last chest x-ray -Breast and axillae: rashes, lumps, discharge, pain, breast self exam practices -Lymphatic: pain, swelling -Cardiovascular: chest pain or distress; possible causes, duration; exercise tolerance, hypertension, dyspnea, edema, circulatory problems -Gastrointestinal: appetite, digestion, food intolerance, abdominal pain, vomiting, stool, dietary patterns (restrictions, special diets, alcohol consumption) -Urinary: painful, blood, stones, puss, past infections to kidneyor bladder, stream style (dribbling, stopping, constant), night visits -Genital and reproductive: Male: puberty onset, erections, testicular pain, libido, infertility, discharge, STDs, self exam, sexual preference Female: menses (onset, duration, regularity, flow, discomfort, last time), menopause, pap test, pregnancies (number, complications), BC, sexual preference -Muscuoloskeletal: pain, joint (stiffness, swelling, limited mobility), muscle wasting, weakness, general mobility 3 -Neurological: injury, headaches, dizziness, fainting, abnormalities of sensation or coordination, tremors, seizures -Endocrine: excessive sweating, thirst, hunger, urination, heat/cold intolerance, changes in distribution of facial hair, thyroid enlargement, change in weight, change in glove or shoe size -Hemotological: anemia, bruise or bleed easily, transfusions -Psychiatric: depression, mood changes, difficulty concentrating, nervousness, anxiety, suicidal thoughts, irritability -Immunological: communicable diseases (onset, age), immunizations (year), allergies Definitions: Cue: information obtained through senses Inference: judgement or interpretations of cues When collecting data you group cues then, inferences and patterns arise then you can anticipate potential problems and solutions. Figure 13-3 Example of branching logic for selecting assessment questions: This figure shows how to ask better, more relevant questions based on client’s verbal and nonverbal cues and previous answers. (note: not that important, but I said to include such things) Types of Data 1. Subjective Data: From client’s verbal descriptions about themselves (feelings, perceptions, symptoms) 2. Objective Data: observations or measurements about client’s health status (wound size, BP, behavioural characteristics: fear, anxiety) Sources of Data From variety of sources; provides info on: level of wellness, strengths, anticipated prognosis, risk factors, health practices, goals, patterns of health and illness Client Best source of info when client is conscious and alert because they will generally answer questions correctly. If the client is experiencing acute symptoms in emergency generally do not give as much information, so be interested to coax more information out of them. Family and Significant Others 1. Family and significant others are primary sources of information if the client is an infant, child, critically ill adult, mentally handicapped, disoriented or unconscious. 2. Family and significant others are secondary sources for adult patients in healthy mindsets; secondary sources provide such info on medications taking practices, and sleeping and eating irregularities Health Care Team -Pass and obtain information to other members of the health care team about client because each has different view points and backgrounds (other nurses from next shift, physicians, physical therapists, social workers, other pertinent staff consultants) Medical Records 4 Medical history, lab and diagnostic tests, current physical findings, medical treatment plan (confidential) Info obtained: Baseline and ongoing information about client’s response to illness and progress (Tool for checking the consistency and similarity of personal observations) Literature Assessments based on (medical, pharmacological, etc lit) Nurses Experience Refines your assessing abilities in subsequent interactions with differing patients with similar symptoms Methods of Data Collection Interview Orientation phase: -Introduce yourself to the client, explain your role, confidentiality, and explain the role of other health care professionals during care -Establish a caring therapeutic relationship with the client Working phase: -gather info about health status using nursing health history -explore client’s current illness, health history, and expectations of care and worries -objective: identify patterns of health and illness, risk factors for behavioural health problems, changes from normal function, available resources for adaptation -1st interview is most extensive because you are updating their info Termination phase: -give a cue that the interview is ending, “so I’m gonna ask you 2 more questions” -this gives the client the opportunity to ask questions -be sure to summarize important points and emphasize important ones Cultural considerations in Assessment Be wary of client’s culture and value system, and their ways of communicating (Spanish and French use strong eye contact; Asians, Middle Easterners and North Americans let their eyes wander); but don’t for opinions on client based on culture alone Use open ended questions when you need them to elaborate on a matter (long drawn out answers) Use close ended questions when you don’t need additional info (yes/no answers) Box 13-2: Examples of Open and Close Ended Questions Open ended: How are you feeling? Close ended: Are you having pain now? Nursing Health History See above, Box 13-1: Guidelines for Documenting a Comprehensive Nursing History You don’t have to go through all questions, as you are more experienced you’ll focus on the pertinent stuff according to what the patient shows you 5 The health history is just meant to have as much data as possible to draw patterns and inferences from. The more someone knows the more prepared they will be... Family History Purpose is to obtain data about immediate and blood relatives to see an illness is genetic or familial in nature, and find ways of preventing it in client and other potential family members. Also provides history on family interaction and function (is the family supportive or stress causing) Documentation of History Findings Make sure the info you obtain is clear, concise, uses appropriate terminology so subsequent lookers can get a clear picture of the client’s status. This information will be the baseline against which you evaluate any future changes. Physical Examination Investigation of the body to determine state of health (using techniques: inspection, palpation, percussion, auscultation, smell; measurements: height, weight, vital signs, body system) Observation of Client Behaviour Observing verbal and nonverbal behaviour allows you to verify data: see if they match (e.g. adult male client says injury doesn’t hurt but is bawling like child). Also allows you to gather additional data like level of function (physical, developmental, psychological and social) Diagnostic and Laboratory Data Diagnostic or lab tests verify, clarify questions you have form the nursing health history and physical exam. (client comes in bc he is coughs up brown sputum and has a cough; examination shows elevated temp and respiration; blood test shows elevated WBC count; X ray shows lower lobe infiltrate = add all together and you get pneumonia) Interpreting Assessment Data and Making Nursing Judgments Again... collect data, analyze and interpret it be noting patterns (critical thinking aspect), then make a decision on how to proceed with client’s are. Data Validation Comparison of data with another source to determine accuracy, so validate findings from the physical examination and observation of client behaviour by comparing data in the medical record and by consulting with other nurses or health care team members and family members. This is to make sure that the client’s data base of info is correct when you analyze it Analysis and Interpretation After collecting data about the client interpret it by recognizing patterns and trends in clustered data, comparing them with standards and formulate a reasonable conclusion Box 13-3 Steps to data analysis 1. Recognize a pattern or trend by cues: Turns slowly, unable to bend over, walks with hesitation 2. Compare with normal standards: has normal range of motion, initiates movement w/o hesitation 3. Make a reasoned conclusion: has limited mobility, has reduced activity level 6 Data Documentation Last part of complete assessment, record everything seen, heard, smelled. When entering data don’t generalize or form judgments through written communication. Concept mapping: A visual way of showing connection between health problems Figure 13-4: sample of concept map: (pretty much a regular mind map) Client with medical assessment in middle, symptoms with possible connections to the medical assessment radiating from middle (positioned by similarity) Middle: medical diagnosis: herniated disc, scheduled for lumbar laminectomy, Surrounding connections: back pain reported at 10, grimacing; moves awkwardly, client scared of surgery; unfamiliar with surgery Nursing diagnosis Next step diagnostic conclusion. Diagnostic conclusions include problems treated primarily by and problems necessitating treatment by several disciplines Medical diagnosis – identification of a disease on the basis of a specific evaluation of physical signs, symptoms, the client’s medical history and the results of diagnostic tests and procedures (ie. Diabetes Mellitus) Nursing diagnosis – clinical judgment about individual, family, or community responses to actual and potential health problems or life processes that is within the domain of nursing (no example given) Collaborative problem – potential physiological complication that nurses monitor to detect the onset of changes in a client’s status. Nurses intervene in collaboration with other disciplines such as physician and nursing diagnosis (i.e surgical wound infection on client; Dr prescribes antibiotics; nurses monitor fever and and apply wound care) Figure 13-5: Critical thinking and the nursing process Nursing process: 1. Assessment; 2. Diagnosis; 3. Planning; 4. Implementation; 5. Evaluation; back to 1 During Diagnosis you just incorporate Experience, Knowledge, Standards and Qualities (similar to figure 13-2) Nursing diagnoses provides the basis for selection of nursing interventions to achieve outcomes for which, a nurse, is accountable. Nursing diagnosis serves several purposes: 1. Provide a precise definition that give all members of the health care team a common language for understanding a client’s needs 2. They allow nurses to communicate their actions amount themselves, to other health care professionals 3. They distinguish the nurse’s role from that of the physician or other health care professionals 7 4. They foster the development of nursing knowledge Figure 13-6 Differentiating nursing diagnosis from collaborative programs: Nurses do not give primary interventions, doctors do; they provide interventions for prevention, treatment or promotion Nurses are part of the collaborative process: prescribe and implement interventions that are in the domain of nursing; monitor and evaluate conditions, implement prescriptive orders of medicine or dentistry Critical Thinking and the Nursing Diagnostic Process Using assessment data to logically explain a clinical judgment, a nursing diagnosis. (steps: data clustering, identifying client needs to formulating the diagnosis) Clusters and patterns of data that help confirm an actual nursing diagnosis. Clinical criteria – objective or subjective signs and symptoms, clusters of signs and cues (symptoms), or risk factors that lead to a diagnostic conclusion Box 13-4: Examples of NANDA nursing diagnoses (not a full list, these are generally easy diagnoses, not like in “House”): Activity tolerance, latex allergy, risk for falls, diarrhea, acute confusion, contamination, disturbed body image, risk of aspiration, deficient in knowledge (condition or surgery) -------------How to: first you cluster similar data, see if they are defining characteristics then based on similar data you draw on conclusion = diagnosis Example: defining characteristics (dyspnea, abnormal respiratory rate, abnormal depth of breathing) = diagnosis (impaired gas exchange or ineffective breathing) From your assessment, the symptoms (cues) that equate to defining characteristics will lead you towards your diagnosis But if client uses accessory muscles to breath and demonstrates pursed lip breathing, the correct diagnosis is not impaired gas exchange but ineffective breather pattern (from Table 13-1) --------------Check other patterns, and see if they are within healthy norms, and make not of them if they are not Formulation of Nursing Diagnosis (created by NANDA International, another governing body) 1. Actual Nursing Diagnosis: responses to health conditions or life processes that exist for individual, family or community; defining characteristics (manifestations, signs, and symptoms) that cluster in patterns of related cues or inferences support this diagnostic judgment (client says back pain is at an 8 = acute pain) 8 2. Risk nursing diagnosis: human responses to health conditions that will probably develop in a vulnerable individual, family or community (i.e. a patient shows a vulnerability due to poor nutrition, is going to have a surgery and will be staying in the hospital = risk for infection) 3. health-promotion nursing diagnosis: clinical judgement of a person’s, family’s, or community’s motivation and desire to increase well-being and actualize human health potential, as expressed in their readiness to enhance specific health behaviours, such as nutrition and exercise (can be used in any health state) 4. Wellness nursing diagnosis: describes levels of wellness in an individual, family, or community that can be enhanced; when a client wants to achieve an optimum level of health (diagnosis: readiness for enhanced coping related to successful cancer treatment – nurse and family work together to adapt to the stressors associated with with cancer while incorporating clients strengths and resources. Components of a Nursing Diagnosis Nursing diagnoses are in a two part format: diagnostic label followed by a statement of related factors. Diagnostic Label: nursing diagnosis approved by NANDA (see above figure 13-4); diagnostic label descriptors to give additional meaning. For example impaired physical mobility, impaired is the descriptor (other descriptors (compromised, promised, decreased, deficient, delayed, effective, imbalanced, impaired and increased). Related Factors: a condition or origin identified from the client’s assessment data. (diagnosis = deficient in knowledge regarding post operative routines; cause = lack of exposure to instruction, client has not had surgery before) Figure 13-7: Diagnostic process of a client Assessment of client’s status: client is concerned about an upcoming back surgery; is worried about paralysis; showing signs of restlessness; uncertain about expectations Validate data: nursing staff says client has poor eye contact Do we need more data? No Interpret and analyze data: Grouped signs: restless + poor eye contact Grouped behaviours: concerned + uncertain of expectations Look for defining characteristics: reveals problem with coping Nursing diagnosis: anxiety related to surgery Table 13-3 Nursing diagnosis: Anxiety related to surgery Intervention: provide detailed instructions about surgical procedure, recovery process and post op care Figure 13-8: the relationship between etiology (origin) and problem isn’t one of cause and effect, they are just associated/related to each other. For example the problem, decreased physical functioning is 9 related to etiology, limited physical activity, strength, coordination, and nutrition. Etiology does not necessarily cause problem, but is related to it. Table 13-4 Defining characteristics and etiologies to confirm nursing diagnosis: Assessment activities: ask client to rate pain 0-10; observe positioning in bed Defining Characteristics: pain at 8; client bends knees while on back Nursing diagnosis: Acute pain Etiologies (“related to”): physical pressure on spinal nerves Definition: approved definition for a diagnosis that follows clinical use and testing Risk factors: environmental, physiological, psychological, genetic or chemical elements that increase the vulnerability of an individual, family or community to an unhealthy event (client shows signs of invasive procedure, trauma, malnutrition, immunosuppression and lack of knowledge to avoid pathogens = diagnosis: risk of infection) Support of the diagnostic statement: nursing assessment must support diagnostic label – make sure your diagnosis falls from the data you collected and clustered Concept mapping for Nursing Diagnosis Figure 13-9: this figure is just stating that when you do a concept map for a patient when you assess them and then analyze the data by clustering similar traits together, the cluster will be interconnected still. Concept mapping is just a way of seeing the big picture and possibly predicting problems. Sources of Diagnostic Errors (elaborated from box 13-5) Errors in Data collection Check for inaccuracy by: -reviewing your level of comfort and competency before conducting interview, physical exam and data collection -go through section by section (interview, phys exam, body systems, head to toe exam) -review clinical assessment in a clinical or class setting for constructive criticism for revision -have a more experienced worker validate your findings -be organized with appropriate forms and equipment, and the environment is comfortable for client Errors in Interpretation and Analysis of Data Review data collected, organize assessments; consider conflicting cues, also consider cultural background, developmental stage when determining meaning of cues (pain is expressed differently in differing cultures; misinterpreting data will lead to inaccurate diagnosis) Errors in Data Clustering -insufficient clustering of cues -premature or early closure of clustering 10 -incorrect clustering Errors in the Diagnostic Statement -use approved language Labelling -wrong diagnostic label selected -existence of evidence that another diagnosis is more likely -condition incorrectly overlooked as a collaborative problem -failure to validate nursing diagnosis with client -failure to seek guidance Documentation -once identifying a client’s nursing diagnosis, list it on plan of care, chronologically Nursing Diagnoses: Application to Care Planning The nursing diagnosis shows us what care is necessary for the clients and provides direction for the planning process and selection of interventions. The care plan is a map for nursing care and demonstrates your accountability for client care; subsequent care plans will assist in communicating to other professionals the client’s health care problems and ensure that you select relevant and appropriate nursing interventions. 11