Announcements
advertisement

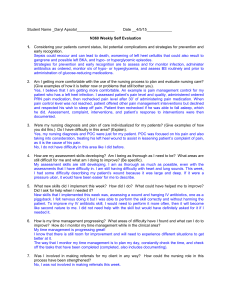
Announcements Here is the tentative blueprint for exam #3 • • • • • • • Sensory (eyes and ears): 3-7 Blood Transfusions: 3-7 Atherosclerosis and HTN: 15-20 DM: 15-20 Dosage calculations: 3 Skills labs: 5-8 (Blood Glucose; Pain; Meds through NG/G tube; Management/Communication NEW: 25 questions added for a cumulative final exam, so 75 questions in all. • 10 - 15 from Unit 1 • 10 - 15 from Unit 2 • Possibly 5 from Unit 3 • • • • The time for the exam will be adjusted accordingly. ATI assessment will be given during lab time. Report to your lab and you will proceed to the assigned rooms. Please remember to bring your ID and password that you used to create your account with ATI. You will not be able to take the assessment without it. Sensory may be self study. Students who need accommodation, please arrange with special services to start your exam at 12pm. Best of luck with your studying. NUR 133 faculty Clarification of terms • • • • DOSE RATE CONCENTRATION PCA – BASAL = CONTINUOUS – PCA = DEMAND –BOLUS • Total medication delivered • Total volume delivered The knowledge of frontline nurses that they gather from their interactions with patients is critical to reducing medical errors and improving patient outcomes. • Involving nurses at a variety of levels across the acute care setting in decision making and leadership benefits the patient, improves the organizations in which nurses practice, and strengthens the health care system in general. • Increasing the time that nurses can spend at the bedside is an essential component of achieving the goal of patient-centered care. • High-quality acute care settings require integrated systems that use technology effectively while increasing the efficiency of nurses and affording them increased time to spend with patients. • Multidisciplinary care teams characterized by extensive and respectful collaboration among team members improve the quality, safety, and effectiveness of care. • Many of the innovations that need to be implemented in the health care system already exist somewhere in the United States, but barriers to their dissemination keep them from being adopted more widely. As Dr. Marilyn Chow observed, “the future is here, it just isn’t everywhere.” http://www.iom.edu/ The future is now Not-as-new TECHNOLOGY Not out of the wrapper yet… Can you read this? Atherosclerosis • http://www.youtube.com/watch?v=OHE1ig4k 64M&feature=relmfu CHAPTER 38 Care of Patients with Vascular Problems Ignatavicius Workman. Medical-Surgical Nursing, 800. Concept Map • Wait for it… CHAPTER 38 Care of Patients with Vascular Problems Ignatavicius Workman. Medical-Surgical Nursing, 800. Concept Map - Lifestyle Modifications • Health Teaching: Instruct the patient about sodium restriction, weight maintenance or reduction, alcohol restriction, stress management, and exercise. If necessary, also explain about the need to stop using tobacco, especially smoking. Provide oral and written information about the indications, dosage, times for administration, side effects, and drug interactions for antihypertensives. Stress that medication must be taken as prescribed and that when all of it has been consumed, the prescription must be renewed on a continual basis. Suddenly stopping drugs such as beta blockers can result in angina (chest pain), myocardial infarction (MI), or rebound hypertension. Also urge patients to report unpleasant side effects, such as excessive fatigue, cough, or sexual dysfunction. In many instances, an alternative drug can be prescribed to minimize certain side effects. Ignatavicius Workman. Medical-Surgical Nursing, 803. • Risk for Ineffective Therapeutic Regimen Management, 802 NURSING PROCESS • • • • • • • ASSESSMENT DATA FOR NURSING DIAGNOSIS NURSING DIAGNOSIS COLLABORATIVE PROBLEMS EXPECTED OUTCOMES WITH INDICATORS NURSING INTERVENTIONS SCIENTIFIC RATIONALE FOR NURSING INTERVENTIONS REALISTIC EVALUATION – Effectiveness of Nursing Interventions – Attainment of Expected Outcomes How do you know if he has hypertension? Categories for Blood Pressure Levels in Adults (in mmHg, or millimeters of mercury) Category Systolic (top number) Diastolic (bottom number) Normal Less than 120 And Less than 80 Prehypertension 120–139 Or 80–89 Stage 1 140–159 Or 90–99 Stage 2 160 or higher Or 100 or higher High blood pressure • What are you going to do about it? Hypertension case study Hypertension Algorithm • Hypertension algorithm • File • JNC VII phycard • http://www.nhlbi.nih.gov/health/dci/index.html • ATP III Guidelines TOD • Target Organ Damage • What is an aneurysm? http://www.mayoclinic.com/health/aorticaneurysm/DS00017 • http://www.sts.org/patientinformation/aneurysm-surgery/aortic-aneurysms *** • http://www.mayoclinic.com/health/food-andnutrition/AN00413 grapefruit interactions • http://hp2010.nhlbihin.net/atpiii/calculator.asp? usertype=prof Where does the salt come from? How Much Salt??? • http://www.iom.edu/Reports/2010/Strategies-to-Reduce-Sodium-Intakein-the-United-States/Report-Recommendations-Strategies-to-ReduceSodium-Intake.aspx • http://www8.nationalacademies.org/onpinews/newsitem.aspx?RecordID= 12818 • http://www.mayoclinic.com/health/sodium/nu00284 • http://www.library.umc.edu/pe-db/pe-noaddsalt.pdf • http://www.library.umc.edu/pe-db/pe-sodium.pdf • http://nutritioncaremanual.org/vault/editor/Docs/2gramsodiumdiet_FINA L.pdf Tobacco dependence syndrome http://www.ncbi.nlm.nih.gov/pubmed/1859602 • World Health Forum. 1991;12(1):70-2. • Implications of the tobacco dependence syndrome for smoking control programmes. • Ramström LM, Masironi R. • Institute for Tobacco Studies, Stockholm, Sweden. • Abstract • Motivational and psychosocial treatments for tobacco dependence, while valuable, are not sufficient to solve nicotine-related problems, which usually require a pharmacological approach. There is also a need for training programmes for health workers and major educational campaigns on the nature of tobacco dependence to be directed at opinion leaders, teachers and the public at large. • PMID: 1859602 [PubMed - indexed for MEDLINE] Five Keys for Quitting Smoking Studies have shown that these five steps will help you quit and quit for good. You have the best chances of quitting if you use them together. • Get Ready. Get Support. Learn new skills and behaviors. Get medication and use it correctly. Be prepared for relapse or difficult situations. • http://www.cdc.gov/tobacco/quit_smoking/how_to _quit/you_can_quit/five_keys/ Diagnosis Assess Monitor Do Risk for ineffective therapeutic regimen management: o Smoking cessation o Blood pressure control o Lipid management o Physical activity o Weight management o Diabetic management o Anti platelets o ACEI o Beta blockers o Influenza vaccination o o o o o o o o o o o Assess the client tobacco use and exposure to tobacco at each visit. Assess for presence of prehypertension SBP=120-129 and DBP= 80-89 if not already diagnosed Assess for SBP< 130140 And DBP< 80 if diabetic or CKD if currently receiving HTN treatment (JNC goal for treatment is 130/80 for CKD and DM vs 140/90 otherwise) Assess if LDL-C < 100 or < 70 for diabetic clients and clients post MI Assess if moderate intensity activities are preformed for 30 minutes per day on most if not all days of the week Assess if BMI 18.524.9 and waist circumference according to gender Men < 40 inches Women< 35 inches Assess fasting blood glucose <100 and if required HgAiC < 7% Assess for compliance and tolerance of antiplatelet therapy Assess for use of ACEI in presence of o o o o o o monitor tolerance to and compliance with antihypertensive therapy monitor tolerance to and compliance with antilipemic therapy monitor tolerance and compliance with TLC diet http://www. nhlbi.nih.go v/cgibin/chd/ste p2intro.cgi monitor compliance with antidiabetic therapy if indicated monitor tolerance to and compliance with anticoagulant therapy monitor tolerance to and compliance with ACE inhibitor therapy monitor tolerance to and compliance with beta blocker therapy o o o o o o o o o Call If indicated; provide referral to Tobacco cessation program for individual counseling Discuss strategies to manage and minimize unique side effects to antihypertensives Instruct client in side effects of antilipemic: o Review side effects for each agent o Review s/s of liver dysfunction o Review s/s of myopathy Review activity recommendations Administer TLC diet Reinforce instruction in bleeding precautions Review management of orthostatic hypotension in response to ACEI Review pulse check and reporting requirements for HR <60 Teach client s/s to report Administer flu vaccine as ordered o o o o o o o o Consult PT/exercise physiologist for exercise prescription Refer to nutritionist for dietary consultation Call MD if fasting blood glucose > 100 if not previously diagnosed with DM Refer to diabetic educator for f/u Hold antilipemic and call cardiologist if myopathy or liver dysfunction is present Hold antihypertensives and call cardiologist if SBP < 90 Hold beta blockers and call cardiologist if HR < 50-60 Call MD if bleeding times are prolonged or s/s of bleeding are present Diagnosis Assess PC: arterial ischemia CAD AAA PAD CVA Mesenteric ischemia Rationale: The client with atherosclerosis is at risk for or may be experiencing the complications of arterial ischemia that may manifest throughout the vascular system as indicated by the disorders listed above. Assess for s/s of arterial ischemia CAD: Chest discomfort, shortness of breath, nausea, diaphoresis, activity intolerance Monitor Do Call CAD Mon for the presence of chest discomfort Be aware that female clients, diabetics and clients of non-white ethnic background may not present with complaints of chest pain. If present Perform 12 lead EKG stat with complaints of chest discomfort to document degree of ischemia Initiate ST elevation MI protocol if indicated Initiate continuous cardiac monitoring Initiate continuous pulse oximetry Mon VS q 4 hours and prn (increase frequency during acute phase and if receiving IV medication that has vasoactive properties) Mon troponin I and cardiac enzymes q 8 hours as ordered for signs of infarction Assess baseline bleeding times Mon electrolytes to determine renal function, hydration and levels of potassium and magnesium Alterations in potassium and magnesium are proarrhythmic Perform lipid measurement if not already performed CAD Initiate measure to restore perfusion Apply oxygen therapy& titrate sao2 > 95% Administer medications to increase myocardial perfusion: Aspirin Thrombolytic therapy Antiplatelet therapy Nitrates Sublingual nitroglyceri n versus IV nitroglyceri n (Tridil) Heparin therapy Administer medications to reduce cardiac workload IV beta blockers followed by beta blockers Mon s/s of CHF and perform echocardiogram as indicated Administer ACEI or ARB for LSVD (left systolic ventricular dysfunction) if ordered Prepare client for reperfusion strategies utilizing percutaneous interventions (PCI) or revascularization (CAGB) Initiate protocol to monitor for complications of myocardial infarction Otherwise: Administer as ordered: Antilipemic Antihyperte nsives antiplatelet s CAD Collaborate with cardiologist, interventionalist and cardiac surgeon as indicated Diagnosis PC: arterial ischemia CAD AAA PAD Mesenteric ischemia CVA (Continued) Assess AAA: Assess for abdominal or back pain with a Pulsatile abdominal mass that is severe, sudden, persistent, or constant; may radiate to groin, buttocks, or legs review appearance of Assess for presence of abdominal bruit on auscultation. Assess for necrotic lesion of toes and feet secondary to distal emboli. Assess for s/s of s/s of shock PAD: Complaints of intermittent claudication, Decreased peripheral pulses, peripheral arterial bruits, pallor, peripheral cyanosis, gangrene, ulceration Monitor Do Call AAA Mon vital signs and blood pressure q 4 hours and prn Increase frequency upon initial complaint and if vasoactive agents are in use Perform abdominal exam q 4 hours and prn Do not palpate a pulsating mass if present Mon peripheral pulses q 4 hours and prn for signs of emboli Prepare client for CAT scan if required to document size Perform 12 lead EKG and continuous cardiac monitoring Mon urine output for signs of renal ischemia secondary to emboli Perform preoperative bloodwork; type cross, CBC, metabolic panel, cardiac workup, PT/PTT PAD Assess for presence of acute arterial occlusion manifesting with extremity pain unrelieved by narcotic analgesia Assess brachial ankle index Perform peripheral vascular checks q 4 hours and prn Monitor lipid levels Assess bleeding times Prepare client for angiography Assess for s/s of gangrene and necrosis AAA Initiate hemorrhagic shock protocol if indicated Apply Oxygen therapy Establish IV access Administer blood products Administer IV antihypertensives Insert Foley catheter and mon hourly I/O Prepare for OR Otherwise: Administer as ordered: Antilipemic Antihyperte nsives antiplatelet s PAD Administer medications to maintain tissue perfusion: Aspirin Antiplatelets pentoxifylline Position client to maximize tissue perfusion to lower extremities Do not gatch bed Avoid heavy blankets/pressure on lower extremities Consider use of bed cradle Avoid exposure to extremes in temperature changes/air currents/unnecessary cooling Manage clients requiring revascularization procedures Administer as ordered: Antilipemic Antihyperte AAA Collaborate with vascular surgeon as indicated. PAD Obtain PT consult Collaborative with vascular surgeon if amputation required . Diagnosis Assess PC: arterial ischemia CAD AAA PAD Mesenteric ischemia CVA Rationale: The client with atherosclerosis is at risk for or may be experiencing the complications of arterial ischemia that may manifest throughout the vascular system as indicated by the disorders listed above. Assess for s/s of arterial ischemia MESENTERIC ISCHEMIA Sever abdominal pain, nausea, vomiting diarrhea Abdominal distention, Absent bowel sounds, peritoneal signs, frank blood in stool and emesis s/s shock CVA: Change in mental status headache, blurred vision, paralysis/paresis, change in sensation, nausea, vomiting neurological changes, unequal pupils seizures, slurred speech Monitor Do Call MESENTERIC ISCHEMIA Mon GI status q4 hours and prn Mon for elevated HR and decline in MAP q 4 hours and prn Monitor CBC for leukocytosis, metabolic panel for elevated BUN Assess for metabolic acidosis by ABG as ordered Prepare client for angiography as ordered CVA Monitor neuro checks q 4 hours and prn for neurological changes Monitor for increased blood pressure Prepare client for CAT scan/MRI/MRA as ordered Perform continuous cardiac monitoring to identify arrhythmias. Ands 12 lead EKG Prepare client for carotid Doppler as ordered Assess for presence of hyperglycemia MESENTERIC ISCHEMIA Initiate shock management if symptomatic according to standard protocols Oxygen, cardiac monitor, IV saline Maintain NPO Insert NG tube for gastric decompression as ordered Administer IV antibiotics as ordered Administer IV narcotic analgesic as ordered Prepare client for OR CVA If s/s present, obtain IV access Administer oxygen as per protocol Administer medications according to type of stroke. Prepare to initiate thrombolytic stroke protocol for a thrombotic stroke Administer antihypertensives according to MAP or SBP in collaboration with neurologist Administer anticoagulants if thrombotic stroke Elevate HOB to 15-30 degrees as tolerated Monitor for s/s of increased ICP Otherwise: Administer as ordered: Antilipemic Antihyperte nsives Antiplatelet s Prepare client for carotid endarterectomy if required. MESENTERIC ISCHEMIA Collaborate with vascular surgeon and interventional radiologist as indicated CVA Consult neurologist and neurosurgeons as indicated. Prepare for evacuation of bleeding if hemorrhagic stroke What about my patient? • my guy Telehealth • EBP box p 803 CHAPTER 38 Care of Patients with Vascular Problems Ignatavicius Workman. Medical-Surgical Nursing, 800. • Health Teaching: Instruct the patient about sodium restriction, weight maintenance or reduction, alcohol restriction, stress management, and exercise. If necessary, also explain about the need to stop using tobacco, especially smoking. Provide oral and written information about the indications, dosage, times for administration, side effects, and drug interactions for antihypertensives. Stress that medication must be taken as prescribed and that when all of it has been consumed, the prescription must be renewed on a continual basis. Suddenly stopping drugs such as beta blockers can result in angina (chest pain), myocardial infarction (MI), or rebound hypertension. Also urge patients to report unpleasant side effects, such as excessive fatigue, cough, or sexual dysfunction. In many in-stances, an alternative drug can be prescribed to minimize certain side effects. • Ignatavicius Workman. Medical-Surgical Nursing, 803. Medications • • • • • Page 801 Chart 38-6 Multidrug therapy The Polypill Managing “lots of pills” therapy NURSING PROCESS • • • • • • • ASSESSMENT DATA FOR NURSING DIAGNOSIS NURSING DIAGNOSIS COLLABORATIVE PROBLEMS EXPECTED OUTCOMES WITH INDICATORS NURSING INTERVENTIONS SCIENTIFIC RATIONALE FOR NURSING INTERVENTIONS REALISTIC EVALUATION – Effectiveness of Nursing Interventions – Attainment of Expected Outcomes