14 lobi migrena
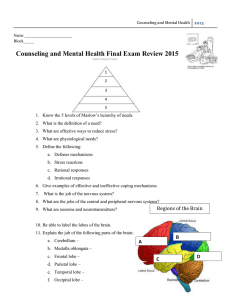
advertisement

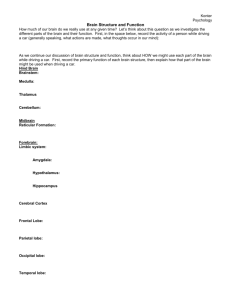
Parietal lobe Parietal lobe • Anterior somatosensory area, posterior association area • 4th neuron of sensory tracts (3, 1, 2 areas – primary somatosensory cortex • 5, 7, 39, 40 areas – somatosensory association areas; areas 5 and 7 are important for stereognosis • Parietal regions appear when the fingers were used for more than just mobility (catching, throwing) Parietal lobe syndromes • • • • Controlateral hemihypestesia (diminished sensation) Astereognosis (5 & 7 areas lesions) Sensory epilepsy (paresiae and sometimes paroxistical pain) Asomatognosia (left hemisphere lesions lead to one side asomatognosia, anosognosia, anosodiaforia, neglect of left body half) • Right parietal lobe – spatial component of activities – Apraxia – loss of the ability to execute or carry out learned purposeful movements, despite having the desire and the physical ability to perform the movements – Finger agnosia – Left-right agnosia Parietal lobe syndromes • Left parietal lobe – symbol and experiences comprehension – ideomotor (inability to carry out a motor command or a learned gesture, for example, "act as if you are brushing your teeth" or "salute") • limb apraxia when movements of the arms and legs are involved, • nonverbal-oral or buccofacial (inability to carry out facial movements on command, e.g., lick lips, whistle, cough, or wink), – ideational (inability to create a plan for or idea of a specific movement, for example, "pick up this pen and write down your name") – Inability to use the informations on spatial relations • Constructive apraxia • Topographic agnosia • Prosopagnosia Parietal lobe syndromes • Speech problems – frequently associated with writing problems • Motor abnormalities (diminishment of spontaneous movements, unstable hand, syncynesia) • Balance problems • Taste problems (area 43) • hemianopia Parietal lobe syndromes • Gerstmann syndrome (left angulary girus) • Digital agnosia • Left-right confusion • Agraphia • Acalculia Parietal lobe syndromes • Balint syndrome (bilateral posterior parietal lesions) – Patient looks only at 35-40 degrees to the right, and describes only the objects in that area – Can look at only one object a time – Neglect of left hemispace – Tactile functions impairment – Visual or tactile agnosia – Apraxia – Speech problems (alexia, aphasia) – Dyscalculia – Immediate memory impairment – Body scheme abnormalities – Left-right confusion – Problems with space orientation – Eye movements problems Parietal lobe Constructive apraxia • Adaptative possibilities of parietal lobes – blind boy “reads” with the tip of his nose Temporal lobe Temporal lobe • Below the sylvian sulcus, extends up to the limits of the parietal and occipital lobes • Primary and secondary auditory areas (41, 42), association areas (38, 20, 21, 22); – Taste (area 38) – Areas 41 and 42: perception and comprehension of sounds, comprehension of words • Lymbic system (hyppocampic uncus, hypocampus, girus cinguli, subcallosal areas, olfactory areas)- emotions and affect • Optic radiations • Left temporal lobe – comprehension and recognition of words, language • Right temporal lobe – intonation, music • • Temporal lobe disfunction Lezarea lobului temporal – Functions in hearing, balance, taste, smell, spoken language, sight, food intake, sexual behaviour – Temporal seizures appear as asoociations of halucinations, consciousness/reason, abnormal behaviours (violent or detached, uncontrollable) Hearing disfunction – area 41 lesions; unilateral lesions – hipoacusia; bilateral lesions – cortical deafness – Iritative lesions – auditory ilusions/halucinations • Balance disfunctions – paroxistical vertigo, sometimes ataxia • Taste and smell disturbances – olfactory hallucinations (sometimes as an aura); anosmia • Visual disturbances – hemianopia, visual memory impairment • Speech disturbance – sensory aphasia (Wernicke) – lesions of the posteroinferior parts of the left superior temporal gyrus Temporal lobe syndrome • Memory impairment – – – Impairment of recent memory – bilateral inferior hippocampic lesions Long time memory impairment – mammilothalamic lesions, bylateral cortical lesions Storing of new memories and their comprehension depends on the Papez circuit (hippocampus, mammilary bodies, thalamus, gyrus cinguli) • Abnormal eating and sexual behaviours – both in temporal lobe lesions and hypothalamic lesions • Temporal lobe epilepsy – – – – Simple or complex psycho-sensorial hallucinations Episodic aphasia Olfactory or auditory hallucinations Mnestic (recognition and recall) disorders– déjà vu, deja pense, jamais vu • • • • Papez circuit James Papez in 1937 One of the major pathways of the limbic system Chiefly involved in the cortical control of emotion. Role in storing memories Kluver-Bucy syndrome • Heinrich Kluver si Paul Bucy, 1939 • Bilateral temporal lobectomy – proof of the role of the Papez circuit in emotional expression • Lack of affect, visual agnosia, indiscriminate sexual expression, severe memory loss Occipital lobe Occipital lobe • Part of the dorsolateral face of the hemispheres • Brodmann areas 17, 18, 19 • Sight – Visual perception – Recognition in relation to space and time – Area 17 (striate) – center of visual information perception - color, shape, dimansion, light, transparency, movement – Area 18 (parastriate) and area 19 (peristriate) – the rest of interhemispheric surface in the occipital lobe • Association cortex • Disfunctions of the occipital lobe can be irritative/destructive, uni- or billateral Occipital lobe syndromes • Irritative lesions: – Simple or complex visual halucinations • Elementary hallucinations: light flashes, colours, gemoetrical shapes, mobile or stationary • Complex hallucinations – objects, persons, animals of normal or abnormal (smaller or larger) dimensions • The patient is either aware of the false nature of these experiences, but he might also be convinced that they are real – Visual illusions (metamorphopsia) – distortions of objects (shape, size, colour, movement) • • • • Images may arouse visual memories The effect can be similar to "dream state" seen in temporal epilepsies Mycropsia, macropsia, moving objects, difformed objects Erithropsia (abnormal colours), lack of colour (acromatopsia), inverted vision, polyopia, irradiation of contours, illusions of movement of stationary objects • Loss of stereoscopic sight, periodic reapparence of visual images after they are no longer in sight (palinopia) • Occipital lobe epilepsy – elementary visual hallucinations, fixed or mobile in the visual field Occipital lobe syndromes • Destructive lesions/visual deficits • Colour agnosia – loss of correct colour perception, inability to name/recognize colours • Unilateral lesions - controlateral homonimous hemianopia (partial or complete loss of sight in the visual field projecting in the primary occipital visual area) • Cortical blindness – both primary visual areas are lesioned – Patients cannot process visual information and behave as in a peripheral blindness – Some patients try to behave as if they were able to see (do not aknowledge the blindness) – Anton syndrome – associates parietal lesions and sensory neglect, sometimes for other types of sensory information Occipital lobe syndromes • • Lesions in the areas 18, 19 of the dominant hemisphere : visual agnosia (objects can be recognized through other senses, but not sight); ussualy associated with verbal agnosia ant homonimous hemianopia Dislexia – impairde written words recognition – • • Word blindness is rare (intact primary visual cortex, but lesions in the association visual cortex in the dominant hemisphere) Prosopagnozia – lesions of the associations areas (ventromedial and occipitotemporal); frequently associated with colour agnosia Balint syndrome – Bilateral occipital lobe lesions, most often in the border areas (19 and 17) of the parieto-occipital region – Failure too properly direct the oculomotor function in exploration of space – Inability to look voluntarily into and scan the peripheral field, failure to grasp or touch an object under visual guidance – Visual innatention that mainly affects the periphery of the visual field Migraine Migraine • Periodic paroxysmal attack of headache • Familial / hereditary; • Females • Usually starts during adolescence • Usually normal imagistic aspects Clinical features of headache • • • • • • Hemicrania Duration (untreated) - 4 – 72 h Pulsatile Medium / severe intensity fono- / foto- / osmofobia Frequently nausea and/or vomiting • Autonomic phenomena (pallor, mydriasis, elevated blood pressure, conjunctival hyperemia, pappiloedema) • Accentuated by physical activity • 3-5 such episodes in history Classification 1.1 Migraine without aura 1.2 Migraine with aura 1.2.1 Typical migraine with aura 1.2.2 Typical aura but no headache 1.2.4 familial hemiplegic migraine 1.2.5 sporadic hemiplegic migraine 1.2.6 basilar migraine 1.3. paroxistical childhood syndromes – migraine precursors 1.3.1 repeated vomiting 1.3.2 abdominal migraine 1.3.3 paroxistical benign vertigo of chilhood 1.4 ophtalmoplegic migraine 1.5. migraine complications 1.5.1 chronic migraine 1.5.2 status migrainosus 1.5.3 prolonged aura but no infarct 1.5.4 migraine associated infarctus 1.5.5 migraine triggered seizures Physiopathological mechanisms • Vasomotor theory – – – • Theory of vascular neuroactive substances – • During the acute phase of migraine kinines, acethylcholine, substance P induce a vasodilatator effect an hyperalgia Diencephalic theory – – • Central blood flow is reduced in some territories during the prodromal phase In the acute phase there is vasodilation and arterial distension Adventitial edema Initial disturbance in the hypothalamic structures and limbic cortex that activate noradrenergic mechanisms Reduction of serotonin activity Allergic theory – Association with coryza, frequent urticaria, Quincke oedema, bronchial asthma attacks • Cortical depression theory – – Depolarization wave that spreads on the cortex from the occipital areas at a speed of 3-5 mm/min. Starts with an excitation wave followed by a long period of neuronal depression that associates metabolic disfunctions and diminished local blood perfusion • Integrative theory – Unitary mechanism that explains the apparition of migraine attacks – Unifies all the othe theories – Stress, strong light, carotid artery dilation maight activate specific structures in the midbrain Treatment – acute phase • Triptanes: s.c., oral, nasal spray – Sumatriptan, naratriptan, rizatriptan • Aspirin, paracetamol in high doses • Nonsteroidal antiinflamatory drugs (Ibuprofen, Naproxen, Diclofenac, Tolfenamic acid, Indomethacin suppository • When to treat? – EARLY – Within 2 hours – Treatment during prodrome or aura is even more effective Treatment: Triptans • First line – More effective – Less nausea • Contraindications – CAD – Cost • Routes – Oral – Intranasal – Subcutaneous Treatment: Triptans • Mechanism of Action – Selective serotonin agonist – 5HT1B/1D • Pharmacokinetics/dynamics – Both long and short acting available – Long acting more effective during aura but take longer to act – Short acting have more side effects Treatment: Adjuncts • Anti-emetics – Metoclopromide both as adjunct and monotherapy – Ondansetron IV/oral/ODT • Caffeine – Rebound • Steroids – Dexamethasone – Prednisone Treatment: Non-Pharmacologic • Behavioral – Shown to be effective • 30-50% reduction of migraine frequency • Modalities – – – – Relaxation training Thermal biofeedback with relaxation training Electromyogram biofeedback Cognitive behavioral therapy – No data to guide selection of modality… Treatment: Non-Pharmacologic • Diet – Some benefit to elimination diets – 20% of patients report dietary triggers – Common triggers: Caffeine withdrawal Packaged meats MSG Dairy Fatty foods Aged cheese Red wine Beer Champagne Chocolate Background therapy • If there are more than 2 attaccks/month • Beta-blockers • Antiepileptics: valproic acid, topiramate • Antiserotoninergic drugs • Tricyclic antidepressants