ROSC! Now what??!! - Texas College of Emergency Physicians
advertisement

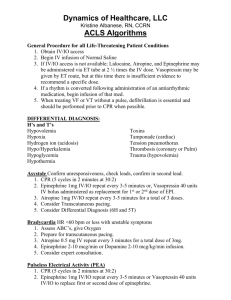
ROSC! Now what??!! An EMS Guide to the Management of Post Cardiac Arrest Syndrome Jay Lance Kovar, MD, FACEP Montgomery County Hospital District PHI Air Medical Texas Objectives o Review o Background and Epidemiology of Cardiac Arrest Survival o Detail o Pathophysiology of Post Cardiac Arrest Syndrome o Discuss o Monitoring, Therapeutic Strategies, and Protocols they apply to the Pre-Hospital Environment o Propose o Integrated EMS Protocols for Improved Intact Neurologic Survivability Background o 1966 Nat'l Academy Sciences Nat'l Research Council on CPR describes ABCD’s o 1972 Dr Valdimir Negovsky “The Second Step” o Advances in CPR and cardiac care has not resulted in improved survivability in 50 years o Post Cardiac Arrest Syndrome o Brain Injury o Myocardial Dysfunction o Systemic Ischemia/Reperfusion Response o Unresolved Pathological Process Background o Barriers to Optimal Outcomes oMultiple Teams/Hand-0ffs oWide variation in Treatments (multicenter trials) oEarly Prognostication Inaccuracies < 72 hrs oResearch focus on ROSC oImproved ROSC w/o Improved Survival Epidemiology o Early Mortality rates after ROSC varies greatly between studies, regions, and hospitals indicating variability in Post Cardiac Arrest Care o Advances in Critical Care over past 5 decades fails to produce improved outcomes o Data Definition Confusion o ROSC o Mortality Location o OOH/IH o Mortality Time Epidemiology o Physiologic Phases of Post Cardiac Arrest Care o Immediate = 0-20 minutes o CPR interventions o Early = 20 minutes – 6 to 12 hours o Early interventions most effective o Intermediate = 6 to 12 hours – 72 hours o Aggressive management of Injury pathways o Recovery = beyond 3 days o Prognostication Reliable o Outcomes Predictable Epidemiology o Mortality Rates Inadequate o Neurologic and Functional Outcomes o Cerebral Performance Category Epidemiology Quality of Life? o Limitation and Withdrawal of Therapy o 63% made DNR, 43% withdrew Therapy in Early and Intermediate time periods << Prognostic period o Can better Care w/i 72 hours result in improved Survivability or increased Organ Donation and Quality? Pathophysiology o Unique Process involving Multiple Organ Systems o Ischemic Injury o Additional Damage During and After Reperfusion o Additive to PreArrest Pathology o Post Cardiac Arrest brain Injury o Post Cardiac Arrest Myocardial Dysfunction o Systemic Ischemia/Reperfusion Response o Persistent Precipitating Pathology (P5) Brain Injury o 68% OOH Mortality 23% IH Mortality o Limited Tolerance of Ischemia o Unique Reperfusion Response post ROSC lasting Hours to Days o Excitotoxicity o Disrupted Ca++ Homeostasis o Free Radical Formation o Pathologic Protease Cascades o Activation of Cell Death Pathways Brain Injury o Protracted Injury Phase opens Broad Therapeutic Window o Cerebral Perfusion becomes dependent upon CePP not Autoregulation or Neuronal Activity o Migratory Intravascular Thrombosis with CPR > 15 minutes (No Reflow) o Hyperemic Flow increases Edema o Luxuriant Hyperperfusion o Excessive Oxygen Free radical Formation Brain Injury o Global CBF is reduced but adequate to meet Oxidative Metabolic Demands in first 48 hours o Transient Edema common post Arrest but rarely increases ICP o Delayed Edema attributable to Ischemic Neurodegradation o Pyrexia o – Poor Outcome Increases with each degree > 370C o Hyperglycemia o – Common and Potentially Mitigated with Insulin Rx o Seizures o – Associated with Worst Prognosis o -- Caused by and Exacerbates Injury Myocardial Dysfunction o Responsive to Therapy and Reversible o Detectible within minutes of ROSC o Decreased EF (stunned) o Increased LVEDP (stiff) o Coronary Blood Flow Normal = Myocardial Stunning o Nadir @ 8 Hrs, Improve @ 24 Hrs, Normal @ 72+ Hrs o Dobutamine improves LVEF and Diastolic Dysfunction Systemic Response o CPR generates poor Cardiac Output, O2 delivery ,and MetaboliteClearance o Oxygen Debt leads to Endothelial Activation and Systemic Inflammation o Predictive of MOSF and Death o Common Sepsis Features o Adrenal Insufficiency o Responsive to Therapy and Reversible o Early Goal Directed Therapy may Optimize Outcomes Persistent Pathology o Precipitating or Contributory Pathology o ACS o AMI >50% OOH Adult Arrests o 48% Acute Coronary Occlusion w/o apparent STEMI o Biomarker Specificity Reduced yet 96% Sensitive for AMI Persistent Pathology o Precipitating or Contributory Pathology o Pulmonary Embolism o Up to 10% Incidence in Sudden Death o Unknown ROSC Rate o COPD, Asthma, or Pneumonia o Pulmonary Function often Worsens post ROSC o Brain Injury and Edema more common after Asphyxic Arrest o Sepsis o Infections more common cause of In Hospital Arrests o Toxins o Environmental Therapeutic Strategy o Critical Care Standards for EMS and ED o Time Sensitive o Account for In/Out of Hospital Settings o Sequential care by multiple Diverse Teams o Accommodate Spectrum of patients o Awake, Stable to Unstable Comatose October 2007 Out-of-Hospital Cardiac Arrest Survival after the Sequential Implementation of 2005 AHA Guidelines for Compressions, Ventilations, and Induced Hypothermia J. Brent Myers, MD MPH Medical Director Wake County EMS System 11.6% 16 14 12 10 8 6 8.2% P<0.05* 7.3% 4.6% 4 2 0 Baseline New CPR * when compared with baseline ITD Hypo I want a new drug • A study of ventricular fibrillation victims, 75% of the surviving patients had a return of spontaneous circulation without injection of a vasopressor; the remaining 25% of patients who required a vasopressor indicated that, if basic life support does not restore spontaneous circulation, the general outcome is most probably poor. Bunch TJ, White RD, Gersh BJ, Meverden RA, Hodge DO, Ballman KV, Hammill SC, Shen WK, Packer DL: Long-term outcomes of out-of-hospital cardiac arrest after successful early defibrillation. N Engl J Med 2003, 348:2626-2633. • Accordingly, once advanced cardiac life support drugs are necessary, rescuers need to understand that the chance the patient will be discharged from the hospital is <10% Wenzel V, Krismer AC, Arntz HR, Sitter H, Stadlbauer KH, Lindner KH: A comparison of vasopressin and epinephrine for out-of-hospital cardiopulmonary resuscitation. N Engl J Med 2004, 350:105-113. Epinephrine • employed in CPR for 100 years • dosage "lumps together" of all etiologies despite differencesin myocardial energetics, postresuscitation function, neurological lesions, and mortality between ventricular fibrillation and other etiologies of arrest • ACLS dose of 1 mg bolus results in dosevariability corresponding to 10 µg/kg in a 100-kg person but 25 µg/kg in a 40-kg person. • increases myocardial oxygen consumption during cardiopulmonary resuscitation • increases the likelihood of cardiac failure after restoration of spontaneous circulation via diastolic dysfunction • "But if you don't have a smashing alternative to the drug, you often just keep using it." Vasopressin • successfully resuscitated cardiac-arrest patients found to have higher endogenous vasopressin levels than those patients who die • vasopressin increases blood pressure differently in the body, constricting the vessels in nonvital organs and dilating the blood vessels in the brain and in the heart • vasopressin appears to work best when ischemia is substantial • typically used only as alternative – and late • Vasopressin is an orphan drug • Is marketing of vasopressin essential to the drug being used by emergency physicians treating cardiac-arrest patients? Vasopressin versus continuous adrenaline during experimental cardiopulmonary resuscitation Resuscitation, Volume 62, Issue 1, Pages 61-69 2004 J.Johansson, R.Gedeborg, S.Rubertsson • Objective: – To evaluate the effects of a bolus dose of vasopressin compared to continuous adrenaline (epinephrine) infusion on vital organ blood flow during cardiopulmonary resuscitation (CPR). • Results: – Vasopressin generated higher cortical cerebral blood flow (P<0.001) and lower cerebral oxygen extraction (P<0.001) during CPR compared to continuous adrenaline. – Coronary perfusion pressure during CPR was higher in vasopressin-treated pigs (P<0.001) and successful resuscitation was achieved in 12/12 in the vasopressin group versus 5/12 in the adrenaline group (P=0.005). • Conclusions: – In this experimental model, vasopressin caused a greater increase in cortical cerebral blood flow and lower cerebral oxygen extraction during CPR compared to continuous adrenaline. Furthermore, vasopressin generated higher coronary perfusion pressure and increased the likelihood of restoring spontaneous circulation. Effects of epinephrine and vasopressin on end-tidal carbon dioxide tension and mean arterial blood pressure in out-of-hospital cardiopulmonary resuscitation: an observational study Stefan Mally , Alina Jelatancev and Stefek Grmec Centre for Emergency Medicine Maribor, Ljubljanska 5, 2000 Maribor, Slovenia Critical Care 2007, 11:R39doi:10.1186/cc5726 • 1 mg of epinephrine intravenously every three minutes only vs vasopressin/epinephrine group 40 units of vasopressin intravenously only or followed by 1 mg of epinephrine every three minutes during CPR. Values of end-tidal carbon dioxide and MAP were recorded, and data were collected according to the Utstein style. • Results – Final end-tidal carbon dioxide values and average values of MAP in patients with restoration of pulse were significantly higher in the vasopressin/epinephrine group (p < 0.01). End-tidal carbon dioxide values as well as MAP at admission to the hospital were associated with survival at 24 hours and improved hospital discharge. – In the vasopressin group, significantly more pulse restorations and a better rate of survival at 24 hours were observed (p < 0.05). Subgroup analysis of patients with initial asystole revealed a higher hospital discharge rate when vasopressin was used (p = 0.04). – Neurological outcome in discharged patients was better in the vasopressin group (p = 0.04). • Conclusion – End-tidal carbon dioxide and MAP are strong prognostic factors for the outcome of out-ofhospital cardiac arrest. This combination vasopressor therapy improves restoration of spontaneous circulation, short-term survival, and neurological outcome. In the subgroup of patients with initial asystole, it improves the hospital discharge rate. A Comparison of Vasopressin and Epinephrine for Out-of-Hospital Cardiopulmonary Resuscitation Volker Wenzel, M.D., Anette C. Krismer, M.D., H. Richard Arntz, M.D., Helmut Sitter, Ph.D., Karl H. Stadlbauer, M.D., Karl H. Lindner, M.D., for the European Resuscitation Council Vasopressor during Cardiopulmonary Resuscitation Study Group • Methods – 40 IU ofvasopressin vs 1 mg of epinephrine, followed by additional treatment with epinephrine if needed. • Results – A total of 1186 patients. – Among patients with asystole, however, vasopressin use was associated with significantly higher rates of hospital admission (29.0 percent, vs. 20.3; P=0.02) and hospital discharge (4.7 percent vs. 1.5 percent, P=0.04). – Among patients in whom spontaneous circulation was not restored with the two injections of the study drug, additional treatment with epinephrine resulted in significant improvement in the rates of survival to hospital admission and hospital discharge in the vasopressin group, but not in the epinephrine group (hospital admission rate, 25.7 percent vs. 16.4 percent; P=0.002; – hospital discharge rate, 6.2 percentvs. 1.7 percent; P=0.002). – Cerebral performance was similar in the two groups. • Conclusions The effects of vasopressin were similar to those of epinephrine in the management of ventricular fibrillation and pulseless electrical activity, but vasopressin was superior to epinephrine in patients with asystole. Vasopressin followed by epinephrine may be more effective than epinephrine alone in the treatment of refractory cardiac arrest. Combination vasopressin/epinephrine does not improve cardiac-arrest outcomes "The lack of superiority of combination therapy over epinephrine alone, regardless of the patient subgroup, suggests it may be futile to add vasopressin to epinephrine during cardiopulmonary resuscitation with advanced cardiac life support," Dr Pierre-Yves Gueugniaud et al,July 3, 2008 New England Journal of Medicine. • Investigators assigned 1442 adults to 1 mg of epinephrine and 40 IU of vasopressin and 1452 adults to 1 mg of epinephrine alone, with the combination of drugs repeated if spontaneous circulation was not restored within three minutes after the first administration. Patients were subsequently given additional epinephrine alone if needed. • The combination therapy with vasopressin and epinephrine did not result in any significant improvement over epinephrine alone. The rates of survival to hospital admission, return of spontaneous circulation, survival to hospital discharge, survival at one year, and neurologic recovery at discharge were similar in both treatment arms. • Gueugniaud and colleagues point out that very few patients in their study had ventricular fibrillation—less than 10% in both treatment arms—and this "precludes a definitive conclusion against the use of vasopressin." • Survivorship to hospital discharge average 2% for both groups Repeat? Repeated Administration of Vasopressin but Not Epinephrine Maintains Coronary Perfusion Pressure After Early and Late Administration During Prolonged Cardiopulmonary Resuscitation in Pigs Volker Wenzel, MD; Karl H. Lindner, MD; Anette C. Krismer, MD; Egfried A. Miller, BS; Wolfgang G. Voelckel, MD; Werner Lingnau, MD Question Should vasopressin be injected during CPR based on results from a subgroup analysis and retrospective studies? “The pragmatic answer is yes. Basic life support saves the 'best' cardiac arrest patients; any subsequent advanced cardiac life support intervention has a decreasing likelihood to restore spontaneous circulation over time. Vasopressin should therefore be employed rapidly if initial epinephrine does not restore spontaneous circulation. Our strategy is to alternate between an initial injection of 1 mg epinephrine i.v. and a subsequent injection of 40 IU vasopressin i.v. every 3–5 minutes during CPR “ Vasopressin combined with epinephrine during cardiac resuscitation: a solution for the future? Volker Wenzel Karl H Lindner Department of Anesthesiology and Critical Care Medicine, Innsbruck Medical University, Austria Critical Care 2006, 10:125doi:10.1186/cc4846 Steroids • Here we go again • Methylprednisolone – Enhances contractile function of heart during and after myocardial ischemia – Enhances contractile function of peripheral arteries during endotoxemia – Within 30 to 60 minutes • Myocardial dysfunction and vasoplegia are key components of post-resuscitation shock Vasopressin, Epinephrine, and Corticosteroids for In-Hospital Cardiac Arrest Mentzelopoulos, et al. Arch Internal Med; vol 1 Jan 12, 2009 • Single center, prospective trial 100 consecutive patients. • 20 IU Vaso + 1mg Epi + 40mg Methylprednisolone and Hydrocortisone taper vs. STD 1 mg Epi for up to 5 CPR cycles • ROSC 81% vs. 52% p=.003 • Survival to D/C 30% vs. 0% • Hymodynamics and Svo2 improved • Less MOSF • Independent of Induced Therapeutic Hypothermia Monitoring o General EMS capabilities o o o o o Pulse Oximetry Capnography EKG, Continuous Monitoring Core Temperature Mean Arterial Pressure Targets o Advanced o Biomarkers Oxygenation o 100% Oxygen o Good for CPR/ROSC o Bad post ROSC o Hyperoxia in early reperfusion harms Post-Ischemic Neurons o 100% FIO2 in 1st Hour post ROSC Worsened Outcome over Immediate Adjustment to 94-96% Ventilation o Autoregulation is dysfunctional yet Cerebrovascular Changes to PACO2 Preserved o Hyperventilation may cause Vasoconstriction and Further Ischemia o Hypoventilation/Hypoxia/Hypercarbia elevates ICP and Metabolic Acidosis o Adjust Rate and Tidal Volume to keep PACO2 near Normal Optimal Hemodynamics o Balance Oxygen Delivery and Demands o Should be Achieved in the Early Post Arrest Phase o Optimize (Not Maximize) o Preload o PaO2 o Afterload o Contractility o Systemic Oxygen Utilization Optimal Hemodynamics o Post Cardiac Arrest Syndrome shares Characteristics with Sepsis o EGDT in Post Cardiac Arrest Syndrome o Optimal MAP? o > 100 mmHg w/i 5 minutes of ROSC Bad o Cerebral perfusion dependant on MAP in Early Phase o No Reflow Phenomenon may require 90-100 mmHg Range o AMI or Myocardial Stunning maybe better at 65-75 mmHg Range Optimal Hemodynamics o Post Cardiac Arrest Syndrome shares Characteristics with Sepsis o EGDT in Post Cardiac Arrest Syndrome o Optimal CVP 8 – 12 mmHg o Relative Intravascular Volume Depletion Exists post ROSC o Account for Pathologies causing Elevated CVP’s o Cardiac Tamponade o RV Infarct o PE o Tension PTX Circulation Support o Hemodynamic instability manifests as Dysrhythmias, Hypotension, and poor Stroke Volume/Output o Early Reperfusion is Best AntiArhythmic Therapy o Optimize RV Filling Pressures 8 -12 mmHG o 3.5 – 6.5 Lt First 24 hours o Inotropes/Vasopressors After Volume Correction o Pressor Dependence up to 72 hours o Select Inotropes by BP, HR, CO, and SvO2 o Dopamine?? Therapeutic Hypothermia o The Only Post Cardiac Arrest Therapy Show to Increase Survival o Ongoing Evaluation of benefit in Patient Populations, Induction Techniques, Target Temperature, Duration of Therapy, and Rewarming Techniques. o Benefit Related to Time of Initiation of Therapy o Induction o IV Fluids and Cooling Pads o Maintenance o Cooling Pads and Catheters o ReWarming Therapeutic Hypothermia Sedation and Paralysis o Indicated for Failure to return to Awake Status w/i 5-10 minutes Post ROSC o Sedation reduces oxygen Consumption o Opoids and Hypnotics Required o EEG Monitoring for Sustained Neuromuscular Blockade Seizures o Increases Cerebral Metabolism 3 Fold o Exclude ICH & Electrolyte Imbalance o Myoclonus o Difficult to Control o Phenytoin Ineffective o Clonazepam most Effective o Improved Outcomes with Hypothermia despite Severe post Arrest Status Epilepticus Prognostication o Pre-Cardiac Arrest Factors o Many Factors Associated with Poor Outcome o Advanced Age o Race o Poor Pre-Arrest health o Diabetes o Sepsis o Metastatic cancer o Renal failure o Homebound Status o Stroke o APACHE II & III Scores o None are Reliable Predictors Prognostication o Intra-Cardiac Arrest Factors o Factors Associated with Poor ROSC o Time To CPR o Duration of CPR o Quality of CPR o Maximum ETCO2 < 10 mmHg o Asystole o Non cardiac Causes o None are Reliable Predictors Post ROSC Prognostication o Post–Cardiac Arrest Factors o Retention of Neurologic Function Immediately after ROSC Best Predictor o Absence of Neurologic Function Immediately after ROSC is Not a Reliable predictor of Poor Outcome o Reliable Predictors occur at 72 Hours Prognostication In the Age of Hypothermia o Therapeutic Hypothermia Improves Survival and Functional Outcome for 1 in every 6 Cardiac Arrest Survivors treated (NNT=6) o Alters Progression of Neurological Injury o Changes the Evolution of Recovery o Changes in Timing and Interpretations are Needed o Do Not Withdraw Support Prematurely Implementation o Clinical Guidelines Don’t Change Practice o Barriers o Structural o Human and Financial Resources o Organizational o Leadership o Scientific o Personal o Intellectual o Attitudinal o Motivation o Environmental o Political o Economic o Cultural o Social Implementation Protocol changes drop/downplay Epi Vasopressin early and repeat accept Pox 96-98% Follow eTCO2 Aim for MAP 65-95mmHg Volume resuscitate Dobutamine over Dopamine Induce Hypothermia Educate colleagues Demand Outcomes Transport to Resuscitation centers Questions o What Will You Do Different Monday?