Confrontational Visual Fields - University of Louisville Ophthalmology
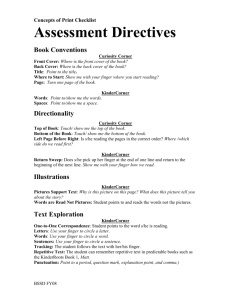
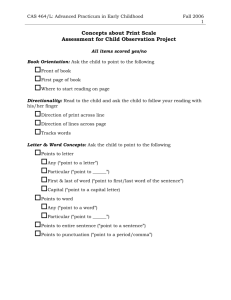
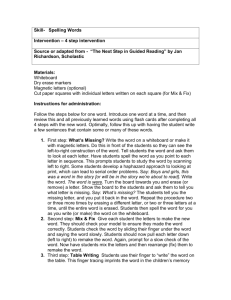
advertisement

Grand Rounds Conference Juan P. Fernandez de Castro, MD University of Louisville Department of Ophthalmology and Visual Sciences June 05, 2015 Subjective CC: Refraction re-check HPI: 76 yo M presents to clinic because of poor vision even with his new glasses; refracted six weeks ago. Previous visit he complained of right sided intermittent headache with associated flashes. No changes in vision. History Past Medical History DM, newly diagnosed. HbA1C 5.9 Hyperlipidemia Meds: Oral DM meds, statin NKDA History Past Ocular History Cataracts OU, not visually significant Glaucoma suspect C/D: 0.65 / 0.4 Tmax: 20mmHg / 20mmHg Central Corneal Thickness: 578 / 550μ Neg Family Hx Migraine with ocular aura Objective VAcc M Rx OD 20/20 OS 20/20-2 +1.00+0.75x008 +1.50+0.75x165 20/20 20/20 +1.25+0.75x007 +1.25+0.75x169 Objective Pupils OD 5→2mm OS 5→2mm NO rAPD IOP EOM 15mmHg Full 16mmHg Full Objective External/Lids Conj/Sclera Cornea Ant Chamber Iris Lens Vitreous WNL OU White OU Clear OU Deep and Quiet OU WNL +1 NS OU Clear Objective DFE OD: C/D 0.65 Sharp, No pallor Macula WNL Vessels WNL Periphery WNL OS: C/D 0.4 Sharp, No pallor Macula WNL Vessels WNL Periphery WNL Upon further questioning… “While driving I have missed a bridge in my property twice in the past month. It has never happened in 30 years” CVF OS OD Neurologic Exam Mental status: Alert and oriented x3 Fluid, appropriate speech No cranial nerve deficit No limb weakness or numbness No gait abnormalities Humphrey Visual Fields 24-2 OS OD Assessment 76 year old white male who presents with a bilateral homonymous visual field deficit. Differential Diagnosis Occipital lobe ischemic event, unknown timing Occipital lobe tumor Plan: Emergency Department for CNS imaging and neurology evaluation CT Head CT Head Hemorrhagic mass surrounded with large edema or acute ischemic injury with a foci of parenchymal heme located mainly in the right temporal and parietal lobe. Recommend MRI Pt transferred to UofL Hospital for further evaluation and treatment MRI Brain Heterogeneously-enhancing right occipital lobe mass measures up to 3.1 cm in maximal diameter, with extensive peritumoral infiltration into the subcortical and periventricular white matter of the right occipital, parietal, temporal, and to a lesser extent, frontal lobes. Brain tumor resection Pre-op Post-op Pathology Right Occipital Dural Base Tumor Biopsy: Metastatic carcinoma, consistent with renal cell carcinoma Postoperative CT Head Postoperative changes from posterior occipital craniotomy are noted with resection of the previously noted enhancing right cuneus mass with no residual enhancement noted to suggest residual enhancing tumor, consistent with gross total resection. CT Abdomen Large heterogeneously enhancing lesion arising from the upper pole of the right kidney, consistent with renal cell carcinoma. BONE SCINTIGRAPHY No convincing scintigraphic evidence of underlying osseous metastatic disease Injection site Bladder Nephrectomy 1 month later, patient undergoes Right laparoscopic radical nephrectomy 4.3 x 4.7 x 5.3 cm mass No complications Current Treatment Brain: Stereotactic Radiotherapy x1 completed Kidney: adjuvant chemotherapy (Pazonib) Follow up with ophthalmology Follow up 2 months VA 20/20 OU Vision is subjectively better HVF 24-2 Improvement 7 ways to do Confrontational Visual Fields Description of examiner’s face Finger counting Finger comparison Red comparison Static finger wiggle Kinetic finger wiggle Kinetic red target Description of examiner’s face Patients to examiner distance 30 cm (test 20 degrees) Are any parts missing OR distorted 20cm Finger counting 20° 60cm 90cm 22cm Use 1 or 2 fingers 20 °eccentric Finger comparison 20°20° 22cm 22cm Are both fingers equally sharp? Red comparison 20°20° 22cm 22cm Use atropine bottle caps Aprox 20mm Are both caps equally red? Static finger wiggle 20°20° 22cm 22cm Wiggle 1 finger Less than 5°oscillation Ask which finger is wiggling Kinetic finger wiggle When is the finger first visible? Kinetic red target 5mm 5mm 5mm 5mm When is the red target first visible? -6 Best 5 Combinations Conclusion Detection of field loss may be the first sign of sight-threatening or potentially life-threatening disease. CVF has limited sensitivity compared with Goldmann or Humphrey VF Even the best combination of CVF tests will fail to detect more than 20% of lesions, so it is important to use an appropriate technique to maximize sensitivity. References Kerr NM, Chew SS, Eady EK, Gamble GD, Danesh-Meyer HV. Diagnostic accuracy of confrontation visual field tests. Neurology. 2010 Apr13; 74(15): 1184-90 Elliott DB, North I, Flanagan J. Confrontation visual field tests. Ophthalmic Physiol Opt 1997;17 suppl 2:S17–S24. Pandit RJ, Gales K, Griffiths PG. Effectiveness of testing visual fields by confrontation. Lancet 2001;358:1339 –1340. Johnson LN, Baloh FG. The accuracy of confrontation visual field test in comparison with automated perimetry. J Natl Med Assoc 1991;83:895– 898.